Abstract
To examine the prevalence of sarcopenia and its association with antirheumatic drugs in adults with rheumatoid arthritis (RA). This review was registered on PROSPERO and followed PRISMA guidelines. Electronic databases were searched for studies reporting on the prevalence of sarcopenia in adults with RA using any muscle index (muscle mass, strength and/or physical performance) and cutpoints as recommended by established criteria (EWGSOP1/2, AWGS, FNIH, SDOC). The secondary objective was to investigate the relationship between RA, antirheumatic drugs, and sarcopenia. Among 2240 middle-aged and older adults with RA (mean age: 47.7 ± 5.5 to 75.0 ± 6.2 years, 83.8% women), the pooled prevalence of low muscle mass/sarcopenia was 30.2% [95% confidence interval (CI) 24.2–36.2%; 16 studies; I2: 89.2%]. Sub-group analysis showed a non-significant higher prevalence of low muscle mass alone (32.6%, 95% CI 25.0–40.3%; I2: 87.9%) versus consensus definitions of sarcopenia (25.4%, 95% CI 15.4–35.3%; I2: 91.2%, p = 0.255). In adults with RA, corticosteroid use was positively associated with sarcopenia [odds ratio (OR) 1.46, 95% CI 0.94–2.29, 7 studies; I2: 47.5%] while conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) was inversely associated (OR 0.70, 95% CI 0.52–0.94; 6 studies: I2: 0.00%) with this muscle disease. No association was found for biological/targeted synthetic disease-modifying antirheumatic drugs (b/tsDMARDs) (OR 0.83, 95% CI 0.54–1.30; 6 studies: I2: 47.6%). Sarcopenia is a common comorbidity of RA, and as such, clinicians should screen for this muscle disease in adults with RA. Further longitudinal studies are needed to understand the role of antirheumatic drugs (particularly type, dosing, and duration) in the development of sarcopenia.



Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Cruz-Jentoft AJ, Sayer AA (2019) Sarcopenia. Lancet 393:2636–2646. https://doi.org/10.1016/S0140-6736(19)31138-9
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31. https://doi.org/10.1093/ageing/afy169
Mayhew AJ, Amog K, Phillips S, Parise G, McNicholas PD, de Souza RJ, Thabane L et al (2019) The prevalence of sarcopenia in community-dwelling older adults, an exploration of differences between studies and within definitions: a systematic review and meta-analyses. Age Ageing 48:48–56. https://doi.org/10.1093/ageing/afy106
Tuttle CSL, Thang LAN, Maier AB (2020) Markers of inflammation and their association with muscle strength and mass: a systematic review and meta-analysis. Ageing Res Rev. https://doi.org/10.1016/j.arr.2020.101185
Wåhlin-Larsson B, Carnac G, Kadi F (2014) The influence of systemic inflammation on skeletal muscle in physically active elderly women. Age (Dordr) 36:9718. https://doi.org/10.1007/s11357-014-9718-0
Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, Nevitt M, Harris TB (2002) Relationship of Interleukin-6 and tumor necrosis factor-with muscle mass and muscle strength in elderly men and women: the health ABC study. J Gerontol A 57:M326–M332. https://doi.org/10.1093/gerona/57.5.m326
Bano G, Trevisan C, Carraro S, Solmi M, Luchini C, Stubbs B, Manzato E, Sergi G, Veronese N (2017) Inflammation and sarcopenia: a systematic review and meta-analysis. Maturitas 96:10–15. https://doi.org/10.1016/j.maturitas.2016.11.006
Smolen JS, Aletaha D, McInnes IB (2016) Rheumatoid arthritis. Lancet 388:2023–2038. https://doi.org/10.1016/S0140-6736(16)30173-8
Littlejohn EA, Monrad SU (2018) Early diagnosis and treatment of rheumatoid arthritis. Prim Care 45:237–255. https://doi.org/10.1016/j.pop.2018.02.010
Myasoedova E, Crowson CS, Kremers HM, Therneau TM, Gabriel SE (2010) Is the incidence of rheumatoid arthritis rising?: results from Olmsted county, Minnesota, 1955–2007. Arthritis Rheum 62:1576–1582. https://doi.org/10.1002/art.27425
Kramer HR, Fontaine KR, Bathon JM, Giles JT (2012) Muscle density in rheumatoid arthritis: associations with disease features and functional outcomes. Arthritis Rheum 64:2438–2450. https://doi.org/10.1002/art.34464
Baker JF, Von Feldt J, Mostoufi-Moab S, Noaiseh G, Taratuta E, Kim W, Leonard MB (2014) Deficits in muscle mass, muscle density, and modified associations with fat in rheumatoid arthritis. Arthritis Care Res 66:1612–1618. https://doi.org/10.1002/acr.22328
Biolo G, Cederholm T, Muscaritoli M (2014) Muscle contractile and metabolic dysfunction is a common feature of sarcopenia of aging and chronic diseases: from sarcopenic obesity to cachexia. Clin Nutr 33:737–748. https://doi.org/10.1016/j.clnu.2014.03.007
Sokka T, Häkkinen A, Kautiainen H, Maillefert JF, Toloza S, Mørk Hansen T, Calvo-Alen J et al (2008) Physical inactivity in patients with rheumatoid arthritis: data from twenty-one countries in a cross-sectional, international study. Arthritis Rheum 59:42–50. https://doi.org/10.1002/art.23255
Klein GL (2015) The effect of glucocorticoids on bone and muscle. Osteoporos Sarcopenia 1:39–45. https://doi.org/10.1016/j.afos.2015.07.008
Tournadre A, Pereira B, Dutheil F, Giraud C, Courteix D, Sapin V, Frayssac T et al (2017) Changes in body composition and metabolic profile during interleukin 6 inhibition in rheumatoid arthritis. J Cachexia Sarcopenia Muscle 8:639–646. https://doi.org/10.1002/jcsm.12189
Subramaniam K, Fallon K, Ruut T, Lane D, McKay R, Shadbolt B, Ang S et al (2015) Infliximab reverses inflammatory muscle wasting (sarcopenia) in Crohn’s disease. Aliment Pharmacol Ther 41:419–428. https://doi.org/10.1002/jcsm.12189
Li TH, Chang YS, Liu CW, Su CF, Tsai HC, Tsao YP, Liao HT et al (2020) The prevalence and risk factors of sarcopenia in rheumatoid arthritis patients: a systematic review and meta-regression analysis. Semin Arthritis Rheum 51:236–245. https://doi.org/10.1016/j.semarthrit.2020.10.002
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC et al (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing 39:412–423. https://doi.org/10.1093/ageing/afq034
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY et al (2014) Sarcopenia in Asia: consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc 15:95–101. https://doi.org/10.1016/j.jamda.2013.11.025
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, Jang HC et al (2020) Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc 21:300–7.e2. https://doi.org/10.1016/j.jamda.2019.12.012
Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, Ferrucci L et al (2014) The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A 69:547–558. https://doi.org/10.1093/gerona/glu010
Bhasin S, Travison TG, Manini TM, Patel S, Pencina KM, Fielding RA, Magaziner JM et al (2020) Sarcopenia definition: the position statements of the sarcopenia definition and outcomes consortium. J Am Geriatr Soc 68:1410–1418. https://doi.org/10.1111/jgs.16372
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 349:g7647. https://doi.org/10.1136/bmj.g7647
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P (2019) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. The Ottawa hospital research institute. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 25 Sept 2020
Ryan R, Hill S (2016) How to GRADE the quality of the evidence. La Trobe University, Melbourne. http://cccrg.cochrane.org/author-resources. Accessed 1 Oct 2020
Newcombe RG (1998) Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med 17:857–872. https://doi.org/10.1002/(sici)1097-0258(19980430)17:8%3c857::aid-sim777%3e3.0.co;2-e
Higgins JP, Thompson SG, Deeks JJ, Altman D (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Baker JF, Long J, Ibrahim S, Leonard MB, Katz P (2015) Are men at greater risk of lean mass deficits in rheumatoid arthritis? Arthritis Care Res 67:112–119. https://doi.org/10.1002/acr.22396
Alkan Melikoğlu M (2017) Presarcopenia and its impact on disability in female patients with rheumatoid arthritis. Arch Rheumatol 32:53–59. https://doi.org/10.5606/ArchRheumatol.2017.6078
Ngeuleu A, Allali F, Medrare L, Madhi A, Rkain H, Hajjaj-Hassouni N (2017) Sarcopenia in rheumatoid arthritis: prevalence, influence of disease activity and associated factors. Rheumatol Int 37:1015–1020. https://doi.org/10.1007/s00296-017-3665-x
Delgado-Frías E, González-Gay MA, Muñiz-Montes JR, Gómez Rodríguez-Bethencourt MA, González-Díaz A, Díaz-González F, Ferraz-Amaro I (2015) Relationship of abdominal adiposity and body composition with endothelial dysfunction in patients with rheumatoid arthritis. Clin Exp Rheumatol 33:516–523
Doğan SC, Hizmetli S, Hayta E, Kaptanoğlu E, Erselcan T, Güler E (2015) Sarcopenia in women with rheumatoid arthritis. Eur J Rheumatol 2:57–61. https://doi.org/10.5152/eurjrheum.2015.0038
Giles JT, Ling SM, Ferrucci L, Bartlett SJ, Andersen RE, Towns M, Muller D, Fontaine KR, Bathon JM (2008) Abnormal body composition phenotypes in older rheumatoid arthritis patients: association with disease characteristics and pharmacotherapies. Arthritis Rheum 59:807–815. https://doi.org/10.1002/art.23719
Reina D, Gómez-Vaquero C, Díaz-Torné C, Solé JMN (2019) Assessment of nutritional status by dual X-ray absorptiometry in women with rheumatoid arthritis: a case-control study. Medicine (Baltimore) 98:e14361. https://doi.org/10.1097/MD.0000000000014361
Koo BS, Yoon B-H (2020) Characteristics of appendicular tissue components in patients with rheumatoid arthritis. J Bone Metab 27:35–42. https://doi.org/10.11005/jbm.2020.27.1.35
Lin JZ, Liang JJ, Ma JD, Li QH, Mo YQ, Cheng WM, He XL et al (2019) Myopenia is associated with joint damage in rheumatoid arthritis: a cross-sectional study. J Cachexia Sarcopenia Muscle 10:355–367. https://doi.org/10.1002/jcsm.12381
Vlietstra L, Stebbings S, Meredith-Jones K, Abbott JH, Treharne GJ, Waters DL (2019) Sarcopenia in osteoarthritis and rheumatoid arthritis: the association with self-reported fatigue, physical function and obesity. PLoS ONE 14:e0217462. https://doi.org/10.1371/journal.pone.0217462
Barone M, Viggiani MT, Anelli MG, Fanizzi R, Lorusso O, Lopalco G, Cantarini L et al (2018) Sarcopenia in patients with rheumatic diseases: prevalence and associated risk factors. J Clin Med 7:504. https://doi.org/10.3390/jcm7120504
Mochizuki T, Yano K, Ikari K, Okazaki K (2020) Sarcopenia in Japanese younger patients with rheumatoid arthritis: a cross-sectional study. Mod Rheumatol. https://doi.org/10.1080/14397595.2020.1740411
Torii M, Hashimoto M, Hanai A, Fujii T, Furu M, Ito H, Uozumi R et al (2019) Prevalence and factors associated with sarcopenia in patients with rheumatoid arthritis. Mod Rheumatol 29:589–595. https://doi.org/10.1080/14397595.2020.1740411
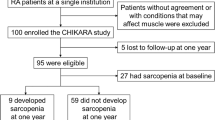
Tada M, Yamada Y, Mandai K, Hidaka N (2018) Matrix metalloprotease 3 is associated with sarcopenia in rheumatoid arthritis—results from the CHIKARA study. Int J Rheum Dis 21:1962–1969. https://doi.org/10.1111/1756-185X.13335
Mochizuki T, Yano K, Ikari K, Okazaki K (2019) Sarcopenia-associated factors in Japanese patients with rheumatoid arthritis: a cross-sectional study. Geriatr Gerontol Int 19:907–912. https://doi.org/10.1111/ggi.13747
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147:755–763. https://doi.org/10.1093/oxfordjournals.aje.a009520
Newman AB, Kupelian V, Visser M, Simonsick E, Goodpaster B, Nevitt M, Kritchevsky SB et al (2003) Sarcopenia: alternative definitions and associations with lower extremity function. J Am Geriatr Soc 51:1602–1609. https://doi.org/10.1046/j.1532-5415.2003.51534.x
Janssen I, Baumgartner RN, Ross R, Rosenberg IH, Roubenoff R (2004) Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. Am J Epidemiol 159:413–421. https://doi.org/10.1093/aje/kwh058
Pacifico J, Geerlings MAJ, Reijnierse EM, Phassouliotis C, Lim WK, Maier AB (2020) Prevalence of sarcopenia as a comorbid disease: a systematic review and meta-analysis. Exp Gerontol 131:110801. https://doi.org/10.1016/j.exger.2019.110801
Sengul I, Akcay-Yalbuzdag S, Ince B, Goksel-Karatepe A, Kaya T (2015) Comparison of the DAS28-CRP and DAS28-ESR in patients with rheumatoid arthritis. Int J Rheum Dis 18:640–645. https://doi.org/10.1111/1756-185X.12695
Greenmyer JR, Stacy JM, Sahmoun AE, Beal JR, Diri E (2020) DAS28-CRP cutoffs for high disease activity and remission are lower than DAS28-ESR in rheumatoid arthritis. ACR Open Rheumatol 2:507–511. https://doi.org/10.1002/acr2.11171
Horsten NC, Ursum J, Roorda LD, van Schaardenburg D, Dekker J, Hoeksma AF (2010) Prevalence of hand symptoms, impairments and activity limitations in rheumatoid arthritis in relation to disease duration. J Rehabil Med 42:916–921. https://doi.org/10.2340/16501977-0619
Wang R, Jiao H, Zhao J, Wang X, Lin H (2016) Glucocorticoids enhance muscle proteolysis through a myostatin-dependent pathway at the early stage. PLoS ONE 11:e0156225. https://doi.org/10.1371/journal.pone.0156225
Kirk B, Feehan J, Lombardi G, Duque G (2020) Muscle, bone, and fat crosstalk: the biological role of myokines, osteokines, and adipokines. Curr Osteoporos Rep 18:388–400. https://doi.org/10.1007/s11914-020-00599-y
Benjamin O, Bansal P, Goyal A, Lappin SL (2020) Disease modifying anti-rheumatic drugs (DMARD). StatPearls [Internet]. StatPearls Publishing, Treasure Island
Friedman B, Cronstein B (2019) Methotrexate mechanism in treatment of rheumatoid arthritis. Joint Bone Spine 86:301–307. https://doi.org/10.1016/j.jbspin.2018.07.004
Smolen JS, Landewé RBM, Bijlsma JWJ, Burmester GR, Dougados M, Kerschbaumer A, McInnes IB et al (2020) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis 79:685–699. https://doi.org/10.1136/annrheumdis-2019-216655
Kirk B, Zanker J, Duque G (2020) Osteosarcopenia: epidemiology, diagnosis, and treatment-facts and numbers. J Cachexia Sarcopenia Muscle 11:609–618. https://doi.org/10.1002/jcsm.12567
Lane NE (2019) Glucocorticoid-induced osteoporosis: new insights into the pathophysiology and treatments. Curr Osteoporos Rep 17:1–7. https://doi.org/10.1007/s11914-019-00498-x
Brance ML, Pons-Estel BA, Quagliato NJ, Jorfen M, Berbotto G, Cortese N, Raggio JC et al (2021) Trabecular and cortical bone involvement in rheumatoid arthritis by DXA and DXA-based 3D modelling. Osteoporos Int 32:705–714. https://doi.org/10.1007/s00198-020-05641-4
Dent E, Morley JE, Cruz-Jentoft AJ, Arai H, Kritchevsky SB, Guralnik J, Bauer JM et al (2018) International clinical practice guidelines for sarcopenia (ICFSR): screening, diagnosis and management. J Nutr Health Aging 22:1148–1161. https://doi.org/10.1007/s12603-018-1139-9
Acknowledgements
The authors would like to thank Evelyn Hutcheon (Clinical Services Librarian, Western Health Library Service, Western Health, Victoria, Australia), who assisted greatly with the construction of the search strategy.
Funding
No specific funding was received from any bodies in the public, commercial, or not-for-profit sectors to carry out the work described in this article.
Author information
Authors and Affiliations
Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published.
Corresponding author
Ethics declarations
Conflict of interest
Thang Dao, Ben Kirk, Steven Phu, Sara Vogrin, and Gustavo Duque declare that they have no conflict of interest.
Ethical Approval
Ethical approval was not applicable for this systematic review and meta-analysis.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dao, T., Kirk, B., Phu, S. et al. Prevalence of Sarcopenia and its Association with Antirheumatic Drugs in Middle-Aged and Older Adults with Rheumatoid Arthritis: A Systematic Review and Meta-analysis. Calcif Tissue Int 109, 475–489 (2021). https://doi.org/10.1007/s00223-021-00873-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-021-00873-w