Abstract
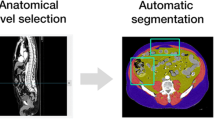
Accurate quantification of bone, muscle, and their components is still an unmet need in the musculoskeletal field. Current methods to quantify tissue volumes in 3D images are expensive, labor-intensive, and time-consuming; thus, a reliable, valid, and quick application is highly needed. Tissue Compass is a standalone software for semiautomatic segmentation and automatic quantification of musculoskeletal organs. To validate the software, cross-sectional micro-CT scans images of rat femur (n = 19), and CT images of hip and abdomen (n = 100) from the Osteoporotic Fractures in Men (MrOS) Study were used to quantify bone, hematopoietic marrow (HBM), and marrow adipose tissue (MAT) using commercial manual software as a comparator. Also, abdominal CT scans (n = 100) were used to quantify psoas muscle volumes and intermuscular adipose tissue (IMAT) using the same software. We calculated Pearson’s correlation coefficients, individual intra-class correlation coefficients (ICC), and Bland–Altman limits of agreement together with Bland–Altman plots to show the inter- and intra-observer agreement between Tissue Compass and commercially available software. In the animal study, the agreement between Tissue Compass and commercial software was r > 0.93 and ICC > 0.93 for rat femur measurements. Bland–Altman limits of agreement was − 720.89 (− 1.5e+04, 13,074.00) for MAT, 4421.11 (− 1.8e+04, 27,149.73) for HBM and − 6073.32 (− 2.9e+04, 16,388.37) for bone. The inter-observer agreement for QCT human study between two observers was r > 0.99 and ICC > 0.99. Bland–Altman limits of agreement was 0.01 (− 0.07, 0.10) for MAT in hip, 0.02 (− 0.08, 0.12) for HBM in hip, 0.05 (− 0.15, 0.25) for bone in hip, 0.02 (− 0.18, 0.22) for MAT in L1, 0.00 (− 0.16, 0.16) for HBM in L1, and 0.02 (− 0.23, 0.27) for bone in L1. The intra-observer agreement for QCT human study between the two applications was r > 0.997 and ICC > 0.99. Bland–Altman limits of agreement was 0.03 (− 0.13, 0.20) for MAT in hip, 0.05 (− 0.08, 0.18) for HBM in hip, 0.05 (− 0.24, 0.34) for bone in hip, − 0.02 (− 0.34, 0.31) for MAT in L1, − 0.14 (− 0.44, 0.17) for HBM in L1, − 0.29 (− 0.62, 0.05) for bone in L1, 0.03 (− 0.08, 0.15) for IMAT in psoas, and 0.02 (− 0.35, 0.38) for muscle in psoas. Compared to a conventional application, Tissue Compass demonstrated high accuracy and non-inferiority while also facilitating easier analyses. Tissue Compass could become the tool of choice to diagnose tissue loss/gain syndromes in the future by requiring a small number of CT sections to detect tissue volumes and fat infiltration.




Similar content being viewed by others
References
Kirk B, Zanker J, Bani Hassan E, Bird S, Brennan-Olsen S, Duque G (2021) Sarcopenia Definitions and Outcomes Consortium (SDOC) criteria are strongly associated with malnutrition, depression, falls, and fractures in high-risk older persons. J Am Med Dir Assoc 22:741–745
Soenen S, Chapman IM (2013) Body weight, anorexia, and undernutrition in older people. J Am Med Dir Assoc 14:642–648
Greco EA, Pietschmann P, Migliaccio S (2019) Osteoporosis and sarcopenia increase frailty syndrome in the elderly. Front Endocrinol (Lausanne) 10:255
Coll PP, Phu S, Hajjar SH, Kirk B, Duque G, Taxel P (2021) The prevention of osteoporosis and sarcopenia in older adults. J Am Geriatr Soc 69(5):1388–1398
Watts NB (2004) Fundamentals, and pitfalls of bone densitometry using dual-energy X-ray absorptiometry (DXA). Osteoporos Int 15(11):847–854
Bhasin S, Travison TG, Manini TM, Patel S, Pencina KM, Fielding RA, Magaziner JM, Newman AB, Kiel DP, Cooper C, Guralnik JM, Cauley JA, Arai H, Clark BC, Landi F, Schaap LA, Pereira SL, Rooks D, Woo J, Woodhouse LJ, Binder E, Brown T, Shardell M, Xue QL, DʼAgostino RB Sr, Orwig D, Gorsicki G, Correa-De-Araujo R, Cawthon PM (2020) Sarcopenia definition: the position statements of the sarcopenia definition and outcomes consortium. J Am Geriatr Soc 68(7):1410–1418
Hirschfeld HP, Kinsella R, Duque G (2017) Osteosarcopenia: where bone, muscle, and fat collide. Osteoporos Int 28(10):2781–2790
Bani Hassan E et al (2018) Marrow adipose tissue in older men: association with visceral and subcutaneous fat, bone volume, metabolism, and inflammation. Calcif Tissue Int 103(2):164–174
Hamrick MW, McGee-Lawrence ME, Frechette DM (2016) Fatty infiltration of skeletal muscle: mechanisms and comparisons with bone marrow adiposity. Front Endocrinol (Lausanne) 7:69
Al Saedi A, Hassan EB, Duque G (2019) The diagnostic role of fat in osteosarcopenia. J Lab Precis Med 4:7
Scott D, Johansson J, Ebeling PR, Nordstrom P, Nordstrom A (2020) Adiposity without obesity: associations with osteoporosis, sarcopenia, and falls in the Healthy Ageing Initiative Cohort Study. Obesity (Silver Spring) 28(11):2232–2241
Guerri S, Mercatelli D, Aparisi Gómez MP, Napoli A, Battista G, Guglielmi G, Bazzocchi A (2018) Quantitative imaging techniques for the assessment of osteoporosis and sarcopenia. Quant Imaging Med Surg 8(1):60–85
Kim DW, Kim KW, Ko Y, Park T, Khang S, Jeong H, Koo K, Lee J, Kim HK, Ha J, Sung YS, Shin Y (2020) Assessment of myosteatosis on computed tomography by automatic generation of a muscle quality map using a web-based toolkit: feasibility study. JMIR Med Inform 8(10):e23049
Wong AK, Beattie KA, Min KK, Gordon C, Pickard L, Papaioannou A, Adachi JD, Canadian Multicentre Osteoporosis Study (CaMos) Research Group (2014) Peripheral quantitative computed tomography-derived muscle density and peripheral magnetic resonance imaging-derived muscle adiposity: precision and associations with fragility fractures in women. J Musculoskelet Neuronal Interact 14(4):401–410
Wong AK, Chandrakumar A, Whyte R, Reitsma S, Gillick H, Pokhoy A, Papaioannou A, Adachi JD (2020) Bone marrow and muscle fat infiltration are correlated among postmenopausal women with osteoporosis: the AMBERS Cohort Study. J Bone Miner Res 35(3):516–527
Hokkanen A, Hämäläinen H, Laitinen TM, Laitinen TP (2021) Test-retest reliability of the assessment of fatty liver disease using low-dose computed tomography in cardiac patients. Front Med (Lausanne) 8:656658
Ngo-Huang A, Herbert A, Fontillas RC, Parker NH, Asumbrado R, Garg N, Dibaj S, Liu DD, Ng AH, Guo Y, Shin KY, Katz MHG, Bruera E (2021) Frequency of sarcopenia, sarcopenic obesity, and changes in physical function in surgical oncology patients referred for prehabilitation. Integr Cancer Ther 20:15347354211000118
Akce M, Liu Y, Zakka K, Martini DJ, Draper A, Alese OB, Shaib WL, Wu C, Wedd JP, Sellers MT, Bilen MA, El-Rayes BF (2021) Impact of sarcopenia, BMI, and inflammatory biomarkers on survival in advanced hepatocellular carcinoma treated with anti-PD-1 antibody. Am J Clin Oncol 44(2):74–81
Barbalho ER, Rocha IMGD, Medeiros GOC, Friedman R, Fayh APT (2020) Agreement between software programmes of body composition analyses on abdominal computed tomography scans of obese adults. Arch Endocrinol Metab 64(1):24–29
Meyer F (1994) Topographic distance and watershed lines. Signal Process 38(1):113–125
Canny J (1986) A computational approach to edge detection. IEEE Trans Pattern Anal Mach Intell 6:679–698
Demontiero O et al (2011) Validation of noninvasive quantification of bone marrow fat volume with microCT in aging rats. Exp Gerontol 46(6):435–440
Orwoll E et al (2005) Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study—a large observational study of the determinants of fracture in older men. Contemp Clin Trials 26(5):569–585
Blank JB et al (2005) Overview of recruitment for the osteoporotic fractures in men study (MrOS). Contemp Clin Trials 26(5):557–568
Verma S et al (2002) Adipocytic proportion of bone marrow is inversely related to bone formation in osteoporosis. J Clin Pathol 55(9):693–698
Meunier P et al (1971) Osteoporosis and the replacement of cell populations of the marrow by adipose tissue: a quantitative study of 84 iliac bone biopsies. Clin Orthop Relat Res (1976–2007) 80:147–154
Duque G et al (2009) Age-related bone loss in the LOU/c rat model of healthy ageing. Exp Gerontol 44(3):183–189
Singh L, Tyagi S, Myers D, Duque G (2018) Good, bad, or ugly: the biological roles of bone marrow fat. Curr Osteoporos Rep 16(2):130–137
Schafer AL et al (2010) Fat infiltration of muscle, diabetes, and clinical fracture risk in older adults. J Clin Endocrinol Metab 95(11):E368–E372
Marcus RL, Addison O, LaStayo PC (2013) Intramuscular adipose tissue attenuates gains in muscle quality in older adults at high risk for falling. A brief report. J Nutr Health Aging 17(3):215–218
Robles PG et al (2015) Intramuscular fat infiltration contributes to impaired muscle function in COPD. Med Sci Sports Exerc 47(7):1334–1341
Therkelsen KE et al (2016) Intramuscular fat and physical performance at the Framingham Heart Study. Age 38(2):31
Levine JA et al (2000) Measuring leg muscle and fat mass in humans: comparison of CT and dual-energy X-ray absorptiometry. J Appl Physiol 88(2):452–456
Maden-Wilkinson T et al (2013) Comparison of MRI and DXA to measure muscle size and age-related atrophy in thigh muscles. J Musculoskelet Neuronal Interact 13(3):320–328
Acknowledgements
The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute on Aging (NIA), the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Center for Advancing Translational Sciences (NCATS), and NIH Roadmap for Medical Research under the following Grant Numbers: U01 AG027810, U01 AG042124, U01 AG042139, U01 AG042140, U01 AG042143, U01 AG042145, U01 AG042168, U01 AR066160, and UL1 TR000128.’
Funding
This study was funded via a Seed Grant from the Australian Institute for Musculoskeletal Science (AIMSS). EB was supported by the Australian Medical Research Frontiers Fund fellowship (MRFF; Melbourne Academic Centre for Health: MACH-RART scheme, 2019).
Author information
Authors and Affiliations
Contributions
MI, EBH, and GD contributed to the study design. MI, EBH, ASTNC, SV, and GD contributed to the collection and interpretation of data. All authors contributed to the drafting and critical appraisal of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
Mahdi Imani, Ebrahim Bani Hassan, Sara Vogrin, Aaron Samuel Tze Nor Ch’Ng, Nancy E. Lane, Jane A. Cauley and Gustavo Duque have no conflict of interest to declare.
Human and Animal Rights
All human and animal studies have been approved by the appropriate ethics committee and have therefore been performed following the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplemental video 1 (MP4 26580 kb)
Supplemental video 2 (MP4 67888 kb)
223_2021_914_MOESM3_ESM.tiff
Supplemental Figure 1 – Comparison between Tissue Compass (on the left) and SliceOmatic’s (on the right) user interface. (TIFF 1364 kb)
223_2021_914_MOESM4_ESM.tiff
Supplemental Figure 2 – Agreement between methods (SliceOmatic vs. Tissue Compass) for a) MAT, b) HBM, and c) bone volume in micro-CT scan of the rat femur bone. The difference in the plots is the difference between Tissue Compass and SliceOmatic. Dashed lines represent mean difference, and gray area shows ±1.96 standard deviation below and above mean difference. (TIFF 335 kb)
Rights and permissions
About this article
Cite this article
Imani, M., Bani Hassan, E., Vogrin, S. et al. Validation of a Semiautomatic Image Analysis Software for the Quantification of Musculoskeletal Tissues. Calcif Tissue Int 110, 294–302 (2022). https://doi.org/10.1007/s00223-021-00914-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-021-00914-4