Abstract
Purpose
This study aimed to investigate the effect of antivirals ritonavir and lopinavir/ritonavir on the pharmacokinetics and pharmacodynamics of oral oxycodone, a widely used opioid receptor agonist used in the treatment of moderate to severe pain.
Methods
A randomized crossover study design with three phases at intervals of 4 weeks was conducted in 12 healthy volunteers. Ritonavir 300 mg, lopinavir/ritonavir 400/100 mg, or placebo b.i.d. for 4 days was given to the subjects. On day 3, 10 mg oxycodone hydrochloride was administered orally. Plasma concentrations of oxycodone, noroxycodone, oxymorphone, and noroxymorphone were determined for 48 h. Pharmacokinetic parameters were calculated with standard noncompartmental methods. Behavioral effects and experimental cold pain analgesia were assessed for 12 h. ANOVA for repeated measures was used for statistical analysis.
Results
Ritonavir and lopinavir/ritonavir increased the area under the plasma concentration–time curve of oral oxycodone by 3.0-fold (range 1.9- to 4.3-fold; P <0.001) and 2.6-fold (range 1.9- to 3.3-fold; P <0.001). The mean (± SD) elimination half-life increased after ritonavir and lopinavir/ritonavir from 3.6 ± 0.6 to 5.6 ± 0.9 h (P <0.001) and 5.7 ± 0.9 h (P <0.001), respectively. Both ritonavir (P <0.001) and lopinavir/ritonavir (P <0.05) increased the self-reported drug effect of oxycodone.
Conclusions
Ritonavir and lopinavir/ritonavir greatly increase the plasma concentrations of oral oxycodone in healthy volunteers and enhance its effect. When oxycodone is used clinically in patients during ritonavir and lopinavir/ritonavir treatment, reductions in oxycodone dose may be needed to avoid opioid-related adverse effects.
Similar content being viewed by others
Introduction
Pain is one of the most frequently reported symptoms associated with human immunodeficiency virus (HIV) infection. It has been estimated that in the developed world, depending on the stage of disease and study settings, 30–80% of people living with HIV/AIDS are affected with pain [1, 2]. Pain experienced by HIV patients can be acute or chronic, and it is usually multifactorial in origin. HIV-associated pain can be due, e.g., to HIV itself, antiretroviral treatment, opportunistic infections, HIV-associated cancers, rheumatic conditions, or peripheral polyneuropathy [3–5]. Unfortunately, these painful conditions are often underrecognized and undertreated.
Oxycodone is a semi-synthetic opioid agonist, which is effective in treating acute, cancer-related, and chronic pain [6, 7]. It is metabolized mainly via oxidative, but also via reductive pathways with only 10–14% being excreted in unchanged or conjugated forms in urine [8]. Oxycodone is principally a cytochrome P450 3A4/5 substrate, which makes it prone to the interactions with CYP3A inducers and inhibitors [9]. The main oxidative pathway includes N-demethylation to noroxycodone by CYP3A4/5 and further to noroxymorphone by CYP2D6 [9]. Approximately 11% of oxycodone is O-demethylated to oxymorphone by CYP2D6, which is further transformed to noroxymorphone by CYP3A4/5 and CYP2D6 [9]. Animal studies have given controversial results about the role of P-glycoprotein in the transport of oxycodone via blood-brain barrier (BBB) [10, 11]. However, the higher concentrations of oxycodone in rat and sheep brain tissue compared to plasma concentrations suggest that the influx protein is much more active than P-glycoprotein, which acts as an efflux protein limiting the concentrations of oxycodone in the brain [12–14].
HIV protease inhibitors, such as ritonavir and lopinavir, inflict the HIV-specific aspartic protease enzyme on processing the gag and gag-pol polyprotein precursor, which leads to the production of immature, noninfectious viral particles [15]. Ritonavir is a potent CYP3A, CYP2D6, and P-glycoprotein inhibitor [16–18]. It has been described to induce CYP1A2, CYP2B6, CYP2C9, and CYP2C19 [19, 20]. Difficult dosing regimens, the development of resistance, and adverse effects have restricted the use of ritonavir as an independent part of HIV treatment [21]. Lopinavir/ritonavir is a combination preparation, where lopinavir is combined with low-dose ritonavir to enhance its low bioavailability by favorable CYP3A inhibition [22]. Lopinavir/ritonavir has become a well-tolerated, effective, and preferred protease inhibitor in the treatment of HIV. It is a substrate and inhibitor of CYP3A4 and to a lesser extent CYP2D6, and an inducer of CYP1A2, 2B6, 2C9, and 2C19 [23, 24], which makes it prone to cytochrome P450-mediated interactions.
In previous studies it has been shown that CYP3A inhibitors voriconazole [25], itraconazole [26], and telithromycin [27] increased the concentrations of oxycodone and oxymorphone, but only minor changes have been observed in the pharmacological action of oxycodone following single doses in healthy volunteers. As HIV patients are often affected with moderate to severe pain, there is an obvious need for the concomitant use of antivirals and strong opioids, such as oxycodone. The aim of this study was to investigate the effects of ritonavir and lopinavir/ritonavir on the pharmacokinetics and effects of oxycodone in healthy volunteers.
Methods
Participants
The study protocol was approved by the Ethics Committee of the Hospital District of Southwest Finland and by the Finnish National Agency for Medicines and was thereby reported to the EudraCT clinical trial register. In view of our previous studies, it was calculated that 10 subjects would be required to detect a 30% difference in the area under the oxycodone concentration–time curves (AUC0–∞) at a level of significance P = 0.05 and power of 80% [25–27]. To allow a drop-out rate of 20%, we decided to recruit 12 subjects. Twelve healthy volunteers, four women and eight men (age 18–26 years; weight 52–84 kg), were studied according to the revised Declaration of Helsinki. Informed consent was obtained from all subjects before study screening. All participants were ascertained to be healthy by means of medical history and clinical examination, and they were tested using routine laboratory tests. Urine screens for drugs with abuse risk were negative and 12-lead electrocardiograms (ECG) were within normal limits. Pregnancy tests for women were negative. None of the participants were receiving any continuous medication including hormonal contraception, and all were nonsmokers. Women in need of contraception were instructed to use nonhormonal methods during the study.
A Finnish translation of Abuse Questions [28] was used to assess risk for drug abuse. The consumption of any product with potential CYP3A effect such as herbal remedies or grapefruit juice was forbidden for 4 weeks and all other drugs for 2 weeks before and during the study. Consumption of coffee, tea, alcohol, and cola drinks was not allowed in the study facility during the study days. Genotyping for CYP2D6 was conducted by a two-step multiplex primer extension method [29]. This method enables the detection of the 11 most relevant polymorphic positions, the definition of whole-gene deletion, duplication, and the allele combination in case of gene duplication.
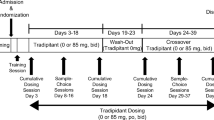
Study design and drug dosing
We used a randomized, crossover study design with three phases at intervals of 4 weeks. During each phase, the volunteers were given four capsules or tablets b.i.d. at 7 a.m. and 7 p.m. for 4 days. The capsules and tablets were packed into sealed coded envelopes which contained one of the following:
-
1.
Two lopinavir/ritonavir 200 mg/50 mg tablets (Kaletra®, Abbott Laboratories, Queenborough, UK) and two placebo capsules
-
2.
Three ritonavir 100 mg capsules (Norvir®, Abbott Laboratories, Queenborough, UK) and one placebo capsule
-
3.
Four placebo capsules
An oral dose of 10 mg oxycodone hydrochloride (Oxynorm® 10 mg capsule, Mundipharma, Bard Pharmaceuticals, Cambridge, UK) was administered on day 3 at 8 a.m. with 150 ml warm water. The participants arrived at the study facility 1 h before oxycodone administration and were under supervision 12 h after the dosing.
The volunteers fasted for 8 h before oxycodone hydrochloride administration and received a standard meal 4 and 8 h after dosing. Drinking was allowed only during the meals. Adherence to the pretreatment medication schedule was ensured with mobile phone text messages, which the volunteers sent to the investigator after taking each pretreatment dose outside the study facility.
Sampling and determination of drug concentrations
In the study facility, a cubital vein was cannulated for blood sampling. The samples (10 ml each) were collected into EDTA-containing tubes before and 0.5, 1, 1.5, 2, 3, 4, 5, 6, 8, 10, 12, 24, and 48 h after the oxycodone hydrochloride dose. Plasma was separated within 30 min and stored at −70°C until analysis.
Plasma concentrations of oxycodone, noroxycodone, oxymorphone, and noroxymorphone were analyzed with the liquid chromatography-tandem mass spectrometric (LC-MS/MS) method as described earlier [30]. The lower limits of quantification (LLQ) were 0.1 ng/mL for oxycodone and oxymorphone, and 0.25 ng/mL for noroxycodone and noroxymorphone. The interday coefficient of variation was less than 6% for parent oxycodone and less than 13% for the metabolites at relevant plasma concentrations.
The concentrations of ritonavir and lopinavir just before and 2 h after the administration of the dose of pretreatment on the day 3 were determined with the LC-MS/MS method [31]. Saquinavir was used as internal standard. The LLQ was 0.1 μg/ml for ritonavir and 0.4 μg/ml for lopinavir. The interday CVs were <5.4% and <7.0% for ritonavir and lopinavir, respectively, at relevant concentrations (n = 3).
Pharmacokinetic analysis
The pharmacokinetics of oxycodone and its metabolites were determined by standard noncompartmental methods using a pharmacokinetic program WinNonlin (version 4.1, Pharsight, Mountain View, CA, USA). The peak plasma concentrations (Cmax) and the corresponding time to Cmax (tmax) were observed directly from the data. The elimination rate constant (ke) was determined by log-linear regression. The elimination half-life t1/2 was calculated from ln2/ke. The areas under the oxycodone, noroxycodone, oxymorphone, and noroxymorphone concentration-time curves (AUC0–∞) were calculated by trapezoidal rule with extrapolation to infinity. Whenever ke could not be estimated because of low plasma concentrations of the metabolite, AUC0–48 was used instead of AUC0–∞. The metabolite-to-parent drug AUC ratios (AUCm/AUCp) were calculated to compare the relative abundance of each metabolite.
Analysis of pharmacological effects
Behavioral effects
The behavioral measures were performed before and at 1, 2, 3, 4, 5, 6, 8, 10, and 12 h after oxycodone as described earlier [32]. Subjective assessment of drowsiness, deterioration of performance, self-reported drug effect, pleasantness, and nausea or vomiting was quantified using visual analog scales (VAS) and scored 0–100. Attributes assessed included alert/drowsy, good/poor performance, no/strong drug effect, unpleasant/pleasant feeling, and no/extreme nausea or vomiting [33]. Maddox wing test was used to estimate the central coordination of extraocular muscles [34], digit symbol substitution test (DSST) to estimate the central processing of sensory information [35], and Cogan’s pupillometry to measure pupil diameter [36]. All reported and observed adverse effects were recorded.
Experimental pain
The analgesic effect was studied in an experimental cold pressor test, which is sensitive to opioid effects [37]. The subjects placed their left hand up to the wrist into the ice water bath (temperature 0–2°C) for 1 min and reported the first sensation of pain (cold pain threshold, CPT), which was measured in seconds with a stopwatch. The intensity of cold pain at 60 s (CPI) was assessed using numerical rating scale (NRS 0–100). The area under the drug effect–time curve (AUEC0–12) from 0 to 12 h was calculated with linear trapezoidal rule based on the observations by the use of WinNonlin (version 4.1, Pharsight Corporation, Mountain View, CA, USA) software for all effect variables.
Statistics
The results are expressed as mean ± SD, except for tmax, where medians with minimum and maximum values are reported. In figures, for clarity, mean ± SEM are given. Descriptive and comparative statistics were calculated with use of SYSTAT for Windows (version 10.2; Systat software, Richmond, CA, USA). The pharmacokinetic and pharmacodynamic variables were compared with the use of analysis of variance for repeated measures, and a posteriori testing was performed with Tukey’s test. Pharmacokinetic data were logarithmically transformed before statistical comparisons. Analysis of variance was used to determine the contributions of treatment, CYP2D6 genotype, gender, phase, and sequence on overall variance. The tmax was analyzed by Friedman’s test, and Wilcoxon signed rank test was used for pair wise comparisons. P was considered significant at the level of <0.05. We also calculated geometric mean ratios with 90% confidence intervals (CI) for the pharmacokinetic parameters. Bioequivalence (i.e., the lack of an interaction) was concluded if the 90% CI of the geometric mean ratio (coadministration/oxycodone alone) was within the acceptance limit of 0.8 to 1.25.
Results
All subjects completed the study.
Pharmacokinetic results
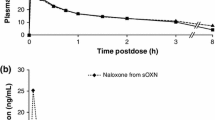
The pharmacokinetic results are presented in Fig. 1 and Table 1. During the ritonavir and lopinavir phases, all of the calculated pharmacokinetic parameters for oxycodone were outside the bioequivalence acceptance limits (Table 1). Compared with placebo, ritonavir and lopinavir/ritonavir increased the oxycodone AUC0–∞ (geometric mean ratio) by 3.0-fold (90% CI 2.6, 3.4; P <0.001) and 2.6-fold (90% CI 2.3, 2.9; P <0.001), respectively. Ritonavir increased the geometric mean ratio of oxycodone Cmax by 1.7-fold (90% CI 1.5, 2.0; P <0.001) and prolonged its elimination half-life from 3.6 ± 0.6 to 5.6 ± 0.9 h (P <0.001). Lopinavir/ritonavir increased the geometric mean ratio of oxycodone Cmax by 1.4-fold (90% CI 1.2, 1.7; P <0.05) and prolonged its elimination half-life to 5.7 ± 0.9 h (P <0.001). Gender had no significant influence on the pharmacokinetic parameters of oxycodone.
Plasma concentrations (mean ± SEM) of oxycodone and its metabolites in 12 healthy volunteers after administration of placebo (control), ritonavir (300 mg b.i.d.), or lopinavir/ritonavir (400/100 mg b.i.d.) for 4 days. Oxycodone hydrochloride (10 mg per os) was given on day 3 at 8 a.m. with 150 ml of warm water. For clarity, SEMs were used instead of SDs. SEMs can be converted into SDs by multiplying by the square root of 12 (3.46). Time = 0 refers to the time of oxycodone administration
Both ritonavir and lopinavir/ritonavir decreased the geometric mean ratio for noroxycodone AUC0–48 to 0.49 (90% CI 0.43, 0.58, P <0.001) and 0.44 (90% CI 0.38, 0.50; P <0.001), respectively. Ritonavir alone had no effect on oxymorphone but lopinavir/ritonavir increased geometric mean ratio for oxymorphone AUC0–48 by 2.7-fold (90% CI 2.0, 3.8; P <0.05). The geometric mean ratio for noroxymorphone AUC0–48 was 0.19 (90% CI 0.15, 0.24; P <0.01) after ritonavir and 0.24 (90% CI 0.16, 0.35; P <0.01) after lopinavir/ritonavir. Four subjects during the ritonavir phase and three subjects during the lopinavir/ritonavir phase had no detectable concentrations of noroxymorphone during the study period 0–48 h.
Nine volunteers were classified as extensive metabolizers (EM). Three of them were homozygous for CYP2D6*1 allele and the rest of the genotypes were CYP2D6*1/4 (n = 3), CYP2D6*1/5 (n = 2), and CYP2D6*1/41 (n = 1). Furthermore, there were two subjects with CYP2D6*1/1 × 2 genotype classified as ultrarapid metabolizer (UM) and one CYP2D6*10/*41 classified as intermediate metabolizer (IM). The IMs appeared to have lower oxymorphone AUC values than most of the extensive metabolizers during all phases (data not shown).
After pretreatment with ritonavir, plasma ritonavir concentrations (mean ± SD) measured 0.5 and 3 h after the morning dose on day 3 were 3.2 ± 1.6 and 8.7 ± 2.6 μg/ml, respectively. After lopinavir/ritonavir pretreatment, the corresponding plasma lopinavir concentrations were 9.0 ± 2.0 and 11.3 ± 2.9 μg/ml and ritonavir concentrations were 0.5 ± 0.3 and 1.0 ± 0.5 μg/ml, respectively. All volunteers had measurable values of ritonavir and ritonavir/lopinavir before the morning dose during active phases indicating compliance with the dosing schedule.
Pharmacodynamic results
Results from behavioral and analgesic tests are shown in Fig. 2. The self-reported drug effect AUEC0–12 increased significantly after ritonavir and lopinavir/ritonavir (P <0.001 and <0.05). Ritonavir increased also nausea and vomiting as measured by VAS (P <0.01), but no other statistically significant differences were observed in the pharmacological response to oxycodone.
Pharmacodynamic parameters in 12 healthy volunteers after administration of placebo (control), ritonavir (300 mg b.i.d.), or lopinavir/ritonavir (400/100 mg b.i.d.) for 4 days. Oxycodone hydrochloride (10 mg per os) was given on day 3 at 8 a.m. with 150 ml of warm water. The figures are presented as mean (± SEM) of self-reported drug effect and nausea (VAS 0–100), pupil size (mm), cold pain threshold (CPT in seconds), score for the digit symbol substitution test (DSST), and value for coordination of the extraocular muscles (diopters) in 12 healthy volunteers. For clarity, SEMs were used instead of SDs. SEMs can be converted into SDs by multiplying by the square root of 12 (3.46). Time = 0 refers to the time of oxycodone administration
The adverse effects reported are presented in Table 2. All three volunteers with vomiting were treated with 2 mg intravenous tropisetron 4, 8, or 12 h after oxycodone.
Discussion
This study convincingly demonstrates that short-term administration of ritonavir or lopinavir/ritonavir strongly inhibits the CYP3A-mediated N-demethylation of oxycodone, as reflected by an approximately two- to threefold increase in oxycodone AUC0–∞ and decrease in noroxycodone AUC0–48. When oxycodone was administered together with ritonavir or lopinavir/ritonavir, the mean concentration of oxycodone was still higher at 8 h than the Cmax during the control phase. These pharmacokinetic changes were accompanied by enhanced self-reported drug effects after both antiviral treatments.
Ritonavir has been shown to be a strong inhibitor of CYP3A both in vitro [38, 39] and in vivo [16, 18, 40, 41]. In the present study, ritonavir caused a threefold mean increase in oxycodone AUC0–∞, which is somewhat smaller than that observed after the azole antimycotic voriconazole (3.6-fold increase in oxycodone AUC0–∞), but bigger than that observed for itrazonazole (2.4-fold increase) and telithromycin (1.8-fold increase) [25–27]. It can be speculated, although it seems doubtful, that the interaction between oxycodone and ritonavir would have been stronger, if a larger ritonavir dose as recommended by the manufacturer would have been used. However, because we wanted to minimize possible adverse effects in healthy volunteers, 300 mg b.i.d. was used and the treatment lasted only 4 days. This could lead to bias, as the steady-state was not reached [21]. Ritonavir has been reported to cause an enzyme induction after approximately 2 weeks administration, which can diminish the inhibitory effects [42, 43].
Interestingly, lopinavir/ritonavir resulted in an almost equal alteration in oxycodone pharmacokinetics as compared to ritonavir. The clinically used maintenance dose of ritonavir is 600 mg b.i.d., which is recommended to be attained over a 2 week period to avoid adverse effects. During the 4-day pretreatment, our volunteers were given 300 mg of ritonavir b.i.d., which is three times higher than the dose of ritonavir during the lopinavir/ritonavir phase. Still, the pharmacokinetics of oxycodone was very similar whether it was given together with ritonavir or lopinavir/ritonavir. A plausible explanation for the observed pharmacokinetic changes is the additional inhibitory effect by lopinavir. Lopinavir is a less potent inhibitor of CYP3A in vitro than ritonavir, but it might nonetheless contribute to net CYP3A inhibition in vivo during the treatment with the combination of lopinavir and ritonavir. The dose-response curve for CYP3A inhibition by ritonavir can be so flat in vivo that despite a threefold dose reduction, it causes a maximum inhibition of CYP3A when combined with a fourfold higher dose of lopinavir [44].
Ritonavir inhibits CYP2D6 in vitro, but to a lesser extent than it inhibits CYP3A [44, 45]. In the present study, oxymorphone concentrations were increased during both antiviral phases indicating the increased significance of the compensatory oxycodone metabolic route via CYP2D6 during CYP3A inhibition. In a previous study, coadministration of oxycodone and telithromycin, an inhibitor of CYP3A and CYP2D6, shifted the metabolism of oxycodone towards the CYP2D6-mediated route increasing oxymorphone concentrations [27]. After lopinavir/ritonavir, the geometric mean ratio for oxymorphone AUC was increased 2.7-fold. Earlier studies have reported CYP2D6 inhibition during lopinavir/ritonavir administration [17, 24]. The inhibition was not strong enough to totally hinder the compensation via the CYP2D6-mediated route after CYP3A inhibition. The formation of oxymorphone has recently been shown to be dependent on CYP2D6 genotype [46]. In our study with only 12 healthy volunteers, there were 9 extensive, 1 intermediate, 2 ultrarapid but no poor metabolizers. In the present small-scale study, these genotypes were not associated with changes in pharmacokinetic parameters of oxycodone or its metabolites.
The self-reported drug effect of oxycodone was significantly increased by both ritonavir and lopinavir/ritonavir. In addition to oxycodone, ritonavir was also involved in the side effects because approximately 25% of ritonavir users typically report nausea or vomiting [21]. Contrary to our previous studies, oxycodone reduced pain in the cold pressor test only in some subjects. As only a single dose of oxycodone was used in the current study in order to minimize the exposure of healthy volunteers to opioids, the drug effect remained smaller compared to the normal clinical setting. Moderate differences in drug concentrations do not necessarily affect the pharmacologic response because of the log-linear relationship between the drug concentration and effect. Furthermore, the power of this study was insufficient to show differences between ritonavir or lopinavir/ritonavir and placebo phases in pharmacodynamic parameters because our primary interest was a change in the oxycodone AUC and the calculation of the sample size was based on that endpoint.
The possibility of drug-drug interactions must be considered in the treatment of HIV-associated pain. In previous pharmacokinetic studies in healthy volunteers, for instance, the oral bioavailability of alfentanil was increased to 95% from 37% by steady-state ritonavir concentrations [18]. The acute administration of ritonavir reduced the clearance of intravenous fentanyl by 67% [16]. In HIV-negative subjects receiving buprenorphine/naloxone as opioid-replacement therapy, tipranavir/ritonavir reduced the formation of the CYP3A4-dependent active metabolite norbuprenorphine, but the AUC of the parent drug remained unchanged, and no clinical opioid withdrawal symptoms were noted [47]. Contrary to the above-mentioned studies, the concentrations of methadone decreased after ritonavir probably due to the induction of CYP2B6 [43]. Thus, the effect of ritonavir on important opioids can be opposite. Drug-drug interactions in HIV-associated pain management are not restricted only to opioids; concomitant administration of lopinavir/ritonavir caused a 46% reduction in the plasma concentrations of lamotrigine, which is an antiepileptic recommended as a second or third line drug for the treatment of neuropathic pain [6]. The mechanism behind this interaction might be the induction in lamotrigine of glucuronidation [48]. Theoretically, the induction of glucuronidation could have an influence on the metabolism of oxycodone and its metabolites, but these metabolic routes are of minor importance [49] and they were not investigated in this study. Additionally, it is unlikely that the short duration of ritonavir would have induced the glucuronidation of noroxycodone and oxymorphone significantly.
In conclusion, administration of lopinavir/ritonavir and ritonavir greatly increases plasma concentrations of oxycodone. Clinically, attention should be drawn to the concomitant use of oxycodone and ritonavir or lopinavir/ritonavir. Further studies are needed to extend the results to HIV or AIDS pain patients suffering from chronic pain.
References
Lee KA, Gay C, Portillo CJ, Coggins T, Davis H, Pullinger CR, Aouizerat BE (2009) Symptom experience in HIV-infected adults: a function of demographic and clinical characteristics. J Pain Symptom Manage 38:882–893
Frich LM, Borgbjerg FM (2000) Pain and pain treatment in AIDS patients: a longitudinal study. J Pain Symptom Manage 19:339–347
Gray G, Berger P (2007) Pain in women with HIV/AIDS. Pain 132(Suppl 1):S13–S21
Verma S, Estanislao L, Simpson D (2005) HIV-associated neuropathic pain: epidemiology, pathophysiology and management. CNS Drugs 19:325–334
Walker UA, Tyndall A, Daikeler T (2008) Rheumatic conditions in human immunodeficiency virus infection. Rheumatology (Oxford) 47:952–959
Freynhagen R, Bennett MI (2009) Diagnosis and management of neuropathic pain. BMJ 339:b3002
Kalso E (2005) Oxycodone. J Pain Symptom Manage 29:S47–S56
Pöyhiä R, Seppälä T, Olkkola KT, Kalso E (1992) The pharmacokinetics and metabolism of oxycodone after intramuscular and oral administration to healthy subjects. Br J Clin Pharmacol 33:617–621
Lalovic B, Phillips B, Risler LL, Howald W, Shen DD (2004) Quantitative contribution of CYP2D6 and CYP3A to oxycodone metabolism in human liver and intestinal microsomes. Drug Metab Dispos 32:447–454
Boström E, Simonsson US, Hammarlund-Udenaes M (2005) Oxycodone pharmacokinetics and pharmacodynamics in the rat in the presence of the P-glycoprotein inhibitor PSC833. J Pharm Sci 94:1060–1066
Hassan HE, Myers AL, Lee IJ, Coop A, Eddington ND (2007) Oxycodone induces overexpression of P-glycoprotein (ABCB1) and affects paclitaxel’s tissue distribution in Sprague Dawley rats. J Pharm Sci 96:2494–2506
Boström E, Simonsson US, Hammarlund-Udenaes M (2006) In vivo blood-brain barrier transport of oxycodone in the rat: indications for active influx and implications for pharmacokinetics/pharmacodynamics. Drug Metab Dispos 34:1624–1631
Villesen HH, Foster DJ, Upton RN, Somogyi AA, Martinez A, Grant C (2006) Cerebral kinetics of oxycodone in conscious sheep. J Pharm Sci 95:1666–1676
Okura T, Hattori A, Takano Y, Sato T, Hammarlund-Udenaes M, Terasaki T, Deguchi Y (2008) Involvement of the pyrilamine transporter, a putative organic cation transporter, in blood-brain barrier transport of oxycodone. Drug Metab Dispos 36:2005–2013
Debouck C (1992) The HIV-1 protease as a therapeutic target for AIDS. AIDS Res Hum Retroviruses 8:153–164
Olkkola KT, Palkama VJ, Neuvonen PJ (1999) Ritonavir’s role in reducing fentanyl clearance and prolonging its half-life. Anesthesiology 91:681–685
Aarnoutse RE, Kleinnijenhuis J, Koopmans PP, Touw DJ, Wieling J, Hekster YA, Burger DM (2005) Effect of low-dose ritonavir (100 mg twice daily) on the activity of cytochrome P450 2D6 in healthy volunteers. Clin Pharmacol Ther 78:664–674
Kharasch ED, Bedynek PS, Walker A, Whittington D, Hoffer C (2008) Mechanism of ritonavir changes in methadone pharmacokinetics and pharmacodynamics: II. Ritonavir effects on CYP3A and P-glycoprotein activities. Clin Pharmacol Ther 84:506–512
Liu P, Foster G, Gandelman K, LaBadie RR, Allison MJ, Gutierrez MJ, Sharma A (2007) Steady-state pharmacokinetic and safety profiles of voriconazole and ritonavir in healthy male subjects. Antimicrob Agents Chemother 51:3617–3626
Kharasch ED, Mitchell D, Coles R, Blanco R (2008) Rapid clinical induction of hepatic cytochrome P4502B6 activity by ritonavir. Antimicrob Agents Chemother 52:1663–1669
Hsu A, Granneman GR, Bertz RJ (1998) Ritonavir. Clinical pharmacokinetics and interactions with other anti-HIV agents. Clin Pharmacokinet 35:275–291
Cvetkovic RS, Goa KL (2003) Lopinavir/ritonavir: a review of its use in the management of HIV infection. Drugs 63:769–802
Yeh RF, Gaver VE, Patterson KB, Rezk NL, Baxter-Meheux F, Blake MJ, Eron JJ Jr, Klein CE, Rublein JC, Kashuba AD (2006) Lopinavir/ritonavir induces the hepatic activity of cytochrome P450 enzymes CYP2C9, CYP2C19, and CYP1A2 but inhibits the hepatic and intestinal activity of CYP3A as measured by a phenotyping drug cocktail in healthy volunteers. J Acquir Immune Defic Syndr 42:52–60
Wyen C, Fuhr U, Frank D, Aarnoutse RE, Klaassen T, Lazar A, Seeringer A, Doroshyenko O, Kirchheiner JC, Abdulrazik F, Schmeisser N, Lehmann C, Hein W, Schomig E, Burger DM, Fatkenheuer G, Jetter A (2008) Effect of an antiretroviral regimen containing ritonavir boosted lopinavir on intestinal and hepatic CYP3A, CYP2D6 and P-glycoprotein in HIV-infected patients. Clin Pharmacol Ther 84:75–82
Hagelberg NM, Nieminen TH, Saari TI, Neuvonen M, Neuvonen PJ, Laine K, Olkkola KT (2009) Voriconazole drastically increases exposure to oral oxycodone. Eur J Clin Pharmacol 65:263–271
Saari TI, Grönlund J, Hagelberg NM, Neuvonen M, Laine K, Neuvonen PJ, Olkkola KT (2010) Effects of itraconazole on the pharmacokinetics and pharmacodynamics of intravenously and orally administered oxycodone. Eur J Clin Pharmacol 66:387–397
Grönlund J, Saari T, Hagelberg N, Martikainen IK, Neuvonen PJ, Olkkola KT, Laine K (2010) Effect of telithromycin on the pharmacokinetics and pharmacodynamics of oral oxycodone. J Clin Pharmacol 50:101–108
Michna E, Ross EL, Hynes WL, Nedeljkovic SS, Soumekh S, Janfaza D, Palombi D, Jamison RN (2004) Predicting aberrant drug behavior in patients treated for chronic pain: importance of abuse history. J Pain Symptom Manage 28:250–258
Sistonen J, Fuselli S, Levo A, Sajantila A (2005) CYP2D6 genotyping by a multiplex primer extension reaction. Clin Chem 51:1291–1295
Neuvonen M, Neuvonen PJ (2008) Determination of oxycodone, noroxycodone, oxymorphone, and noroxymorphone in human plasma by liquid chromatography-electrospray-tandem mass spectrometry. Ther Drug Monit 30:333–340
Rezk NL, White NR, Jennings SH, Kashuba AD (2009) A novel LC-ESI-MS method for the simultaneous determination of etravirine, darunavir and ritonavir in human blood plasma. Talanta 79:1372–1378
Nieminen TH, Hagelberg NM, Saari TI, Pertovaara A, Neuvonen M, Laine K, Neuvonen PJ, Olkkola KT (2009) Rifampin greatly reduces the plasma concentrations of intravenous and oral oxycodone. Anesthesiology 110:1371–1378
Bond AJ, Lader MH (1974) The use of analoque scales in rating subjective feelings. Br J Med Psychol 47:211–218
Hannington-Kiff JG (1970) Measurement of recovery from outpatient general anaesthesia with a simple ocular test. Br Med J 3:132–135
Stone BM (1984) Pencil and paper tests—sensitivity to psychotropic drugs. Br J Clin Pharmacol 18:15S–20S
Cogan DG (1941) Simplifiied entoptic pupillometer. Am J Ophthalmol 24:1431–1433
Jones SF, McQuay HJ, Moore RA, Hand CW (1988) Morphine and ibuprofen compared using the cold pressor test. Pain 34:117–122
Ernest CS 2nd, Hall SD, Jones DR (2005) Mechanism-based inactivation of CYP3A by HIV protease inhibitors. J Pharmacol Exp Ther 312:583–591
Granfors MT, Wang JS, Kajosaari LI, Laitila J, Neuvonen PJ, Backman JT (2006) Differential inhibition of cytochrome P450 3A4, 3A5 and 3A7 by five human immunodeficiency virus (HIV) protease inhibitors in vitro. Basic Clin Pharmacol Toxicol 98:79–85
Greenblatt DJ, von Moltke LL, Harmatz JS, Durol AL, Daily JP, Graf JA, Mertzanis P, Hoffman JL, Shader RI (2000) Alprazolam-ritonavir interaction: implications for product labeling. Clin Pharmacol Ther 67:335–341
Ouellet D, Hsu A, Granneman GR, Carlson G, Cavanaugh J, Guenther H, Leonard JM (1998) Pharmacokinetic interaction between ritonavir and clarithromycin. Clin Pharmacol Ther 64:355–362
Hsu A, Granneman GR, Witt G, Locke C, Denissen J, Molla A, Valdes J, Smith J, Erdman K, Lyons N, Niu P, Decourt JP, Fourtillan JB, Girault J, Leonard JM (1997) Multiple-dose pharmacokinetics of ritonavir in human immunodeficiency virus-infected subjects. Antimicrob Agents Chemother 41:898–905
Kharasch ED, Hoffer C, Whittington D, Walker A, Bedynek PS (2009) Methadone pharmacokinetics are independent of cytochrome P4503A (CYP3A) activity and gastrointestinal drug transport: insights from methadone interactions with ritonavir/indinavir. Anesthesiology 110:660–672
Weemhoff JL, von Moltke LL, Richert C, Hesse LM, Harmatz JS, Greenblatt DJ (2003) Apparent mechanism-based inhibition of human CYP3A in-vitro by lopinavir. J Pharm Pharmacol 55:381–386
Kumar GN, Rodrigues AD, Buko AM, Denissen JF (1996) Cytochrome P450-mediated metabolism of the HIV-1 protease inhibitor ritonavir (ABT-538) in human liver microsomes. J Pharmacol Exp Ther 277:423–431
Zwisler ST, Enggaard TP, Mikkelsen S, Brosen K, Sindrup SH (2010) Impact of the CYP2D6 genotype on post-operative intravenous oxycodone analgesia. Acta Anaesthesiol Scand 54:232–240
Bruce RD, Altice FL, Moody DE, Lin SN, Fang WB, Sabo JP, Wruck JM, Piliero PJ, Conner C, Andrews L, Friedland GH (2009) Pharmacokinetic interactions between buprenorphine/naloxone and tipranavir/ritonavir in HIV-negative subjects chronically receiving buprenorphine/naloxone. Drug Alcohol Depend 105:234–239
van der Lee MJ, Dawood L, ter Hofstede HJ, de Graaff-Teulen MJ, van Ewijk-Beneken Kolmer EW, Caliskan-Yassen N, Koopmans PP, Burger DM (2006) Lopinavir/ritonavir reduces lamotrigine plasma concentrations in healthy subjects. Clin Pharmacol Ther 80:159–168
Lalovic B, Kharasch E, Hoffer C, Risler L, Liu-Chen LY, Shen DD (2006) Pharmacokinetics and pharmacodynamics of oral oxycodone in healthy human subjects: role of circulating active metabolites. Clin Pharmacol Ther 79:461–479
Acknowledgments
We want to thank Mrs. Elina Kahra, medical laboratory technologist, and Mrs. Mia Suppanen-Olkkola, RN, for their skilful technical assistance; Dr. Juha Grönlund, M.D., for his practical help during the data collection and Mrs. Kaisa J. Kurkinen, M.Sc., for the determination of ritonavir and lopinavir concentrations.
This study was supported by Turku University Hospital research fund EVO 13821 and Turku University Foundation, Turku, Finland; Sigrid Jusélius Foundation and Instrumentarium Research Foundation, Helsinki, Finland.
Conflicts of Interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nieminen, T.H., Hagelberg, N.M., Saari, T.I. et al. Oxycodone concentrations are greatly increased by the concomitant use of ritonavir or lopinavir/ritonavir. Eur J Clin Pharmacol 66, 977–985 (2010). https://doi.org/10.1007/s00228-010-0879-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-010-0879-1