Abstract
Purpose
Elevated serum proinflammatory cytokines are associated with the reduction of cytochrome P450 enzyme (CYP) activity. This study aimed to evaluate the oxycodone pharmacokinetics, central symptoms, and serum proinflammatory cytokines based on cachexia stage in cancer patients.
Methods
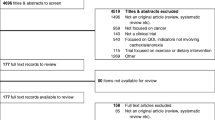
Forty-seven cancer patients receiving extended-release oxycodone were enrolled. Predose plasma concentrations of oxycodone and its metabolites were normalized with the daily dose and body weight. The central symptoms and serum level of proinflammatory cytokines were investigated at each cachexia stage.
Results
The plasma concentrations of oxycodone in patients with cachexia and refractory cachexia were significantly higher than that in patients with precachexia. The metabolic ratio to noroxycodone in patients with cachexia was significantly lower than that in patients with precachexia. The patients with a higher cachexia stage had a higher serum level of interleukin-6 (IL-6), but not tumor necrosis factor-α and interleukin-1β. The serum IL-6 level was correlated with the plasma concentration of oxycodone and inversely with the metabolic ratio to noroxycodone. The incidence of somnolence was not associated with the plasma oxycodone concentration. In contrast, the cachexia stage and its associated serum IL-6 level were correlated with the incidence of somnolence.
Conclusions
Cancer cachexia raised the plasma exposure of oxycodone through the reduction of CYP3A metabolic pathway. The reduction of CYP3A in cachectic cancer patients was associated with an elevation of serum IL-6. Although cachectic cancer patients with higher serum IL-6 levels had the symptom of somnolence, the alterations in oxycodone pharmacokinetics were not related to the incidence of symptom.

Similar content being viewed by others
References
Lalovic B, Phillips B, Risler LL, Howald W, Shen DD (2004) Quantitative contribution of CYP2D6 and CYP3A to oxycodone metabolism in human liver and intestinal microsomes. Drug Metab Dispos 32:447–454
Olkkola KT, Kontinen VK, Saari TI, Kalso EA (2013) Does the pharmacology of oxycodone justify its increasing use as an analgesic? Trends Pharmacol Sci 34:206–214
Leow KP, Smith MT, Williams B, Cramond T (1992) Single-dose and steady-state pharmacokinetics and pharmacodynamics of oxycodone in patients with cancer. Clin Pharmacol Ther 52:487–495
Samer CF, Daali Y, Wagner M, Hopfgartner G, Eap CB, Rebsamen MC, Rossier MF, Hochstrasser D, Dayer P, Desmeules JA (2010) The effects of CYP2D6 and CYP3A activities on the pharmacokinetics of immediate release oxycodone. Br J Pharmacol 160:907–918
Andreassen TN, Eftedal I, Klepstad P, Davies A, Bjordal K, Lundström S, Kaasa S, Dale O (2012) Do CYP2D6 genotypes reflect oxycodone requirements for cancer patients treated for cancer pain? A cross-sectional multicentre study. Eur J Clin Pharmacol 68:55–64
Naito T, Takashina Y, Yamamoto K, Tashiro M, Ohnishi K, Kagawa Y, Kawakami J (2011) CYP3A5*3 affects plasma disposition of noroxycodone and dose escalation in cancer patients receiving oxycodone. J Clin Pharmacol 51:1529–1538
Aoyagi T, Terracina KP, Raza A, Matsubara H, Takabe K (2015) Cancer cachexia, mechanism and treatment. World J Gastrointest Oncol 7:17–29
Suzuki H, Asakawa A, Amitani H, Nakamura N, Inui A (2013) Cancer cachexia—pathophysiology and management. J Gastroenterol 48:574–594
Slaviero KA, Clarke SJ, Rivory LP (2003) Inflammatory response: an unrecognised source of variability in the pharmacokinetics and pharmacodynamics of cancer chemotherapy. Lancet Oncol 4:224–232
Morgan ET (2009) Impact of infectious and inflammatory disease on cytochrome P450-mediated drug metabolism and pharmacokinetics. Clin Pharmacol Ther 85:434–438
Morgan ET, Goralski KB, Piquette-Miller M, Renton KW, Robertson GR, Chaluvadi MR, Charles KA, Clarke SJ, Kacevska M, Liddle C, Richardson TA, Sharma R, Sinal CJ (2008) Regulation of drug-metabolizing enzymes and transporters in infection, inflammation, and cancer. Drug Metab Dispos 36:205–216
Mimura H, Kobayashi K, Xu L, Hashimoto M, Ejiri Y, Hosoda M, Chiba K (2015) Effects of cytokines on CYP3A4 expression and reversal of the effects by anti-cytokine agents in the three-dimensionally cultured human hepatoma cell line FLC-4. Drug Metab Pharmacokinet 30:105–110
Aitken AE, Morgan ET (2007) Gene-specific effects of inflammatory cytokines on cytochrome P450 2C, 2B6 and 3A4 mRNA levels in human hepatocytes. Drug Metab Dispos 35:1687–1693
Naito T, Tashiro M, Ishida T, Ohnishi K, Kawakami J (2013) Cancer cachexia raises the plasma concentration of oxymorphone through the reduction of CYP3A but not CYP2D6 in oxycodone-treated patients. J Clin Pharmacol 53:812–818
Laird BJ, Scott AC, Colvin LA, McKeon AL, Murray GD, Fearon KC, Fallon MT (2011) Pain, depression, and fatigue as a symptom cluster in advanced cancer. J Pain Symptom Manag 42:1–11
Breitbart W, Alici Y (2012) Evidence-based treatment of delirium in patients with cancer. J Clin Oncol 30:1206–1214
Naito T, Tashiro M, Yamamoto K, Ohnishi K, Kagawa Y, Kawakami J (2012) Impact of cachexia on pharmacokinetic disposition of and clinical responses to oxycodone in cancer patients. Eur J Clin Pharmacol 68:1411–1418
Dunlop RJ, Campbell CW (2000) Cytokines and advanced cancer. J Pain Symptom Manag 20:214–232
Farkas G, Márton J, Nagy Z, Mándi Y, Takács T, Deli MA, Abrahám CS (1998) Experimental acute pancreatitis results in increased blood-brain barrier permeability in the rat: a potential role for tumor necrosis factor and interleukin 6. Neurosci Lett 242:147–150
Saija A, Princi P, Lanza M, Scalese M, Aramnejad E, De Sarro A (1995) Systemic cytokine administration can affect blood-brain barrier permeability in the rat. Life Sci 56:775–784
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, Jatoi A, Loprinzi C, MacDonald N, Mantovani G, Davis M, Muscaritoli M, Ottery F, Radbruch L, Ravasco P, Walsh D, Wilcock A, Kaasa S, Baracos VE (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12:489–495
McMillan DC (2008) An inflammation-based prognostic score and its role in the nutrition-based management of patients with cancer. Proc Nutr Soc 67:257–262
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A (2010) AJCC cancer staging manual (7th edition). Springer, New York, NY
Schmitt C, Kuhn B, Zhang X, Kivitz AJ, Grange S (2011) Disease-drug-drug interaction involving tocilizumab and simvastatin in patients with rheumatoid arthritis. Clin Pharmacol Ther 89:735–740
Chung SJ, Kwon YJ, Park MC, Park YB, Lee SK (2011) The correlation between increased serum concentrations of interleukin-6 family cytokines and disease activity in rheumatoid arthritis patients. Yonsei Med J 52:113–120
Netea MG, van der Meer JW, van Deuren M, Kullberg BJ (2003) Proinflammatory cytokines and sepsis syndrome: not enough, or too much of a good thing? Trends Immunol 24:254–258
Machavaram KK, Almond LM, Rostami-Hodjegan A, Gardner I, Jamei M, Tay S, Wong S, Joshi A, Kenny JR (2013) A physiologically based pharmacokinetic modeling approach to predict disease-drug interactions: suppression of CYP3A by IL-6. Clin Pharmacol Ther 94:260–268
Rivory LP, Slaviero KA, Clarke SJ (2002) Hepatic cytochrome P450 3A drug metabolism is reduced in cancer patients who have an acute-phase response. Br J Cancer 87:277–280
Dickmann LJ, Patel SK, Rock DA, Wienkers LC, Slatter JG (2011) Effects of interleukin-6 (IL-6) and an anti-IL-6 monoclonal antibody on drug-metabolizing enzymes in human hepatocyte culture. Drug Metab Dispos 39:1415–1422
Tallgren M, Olkkola KT, Seppälä T, Höckerstedt K, Lindgren L (1997) Pharmacokinetics and ventilatory effects of oxycodone before and after liver transplantation. Clin Pharmacol Ther 61:655–661
Acknowledgments
This work was supported by JSPS KAKENHI grant numbers 26460194 and 26927005.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was performed in accordance with the Declaration of Helsinki and its amendments, and the protocol (25-306) was approved by the Ethics Committee of Hamamatsu University School of Medicine. The patients received information about the scientific aim of the study and each patient provided written informed consent.
Informed consent
All the patients gave their written consent to their participation in the study.
Funding
This work was supported by JSPS KAKENHI Grant Numbers 26460194 and 26927005.
Rights and permissions
About this article
Cite this article
Sato, H., Naito, T., Ishida, T. et al. Relationships between oxycodone pharmacokinetics, central symptoms, and serum interleukin-6 in cachectic cancer patients. Eur J Clin Pharmacol 72, 1463–1470 (2016). https://doi.org/10.1007/s00228-016-2116-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-016-2116-z