Abstract
Carbapenemase-producing Klebsiella pneumoniae (CP-Kp) is a real global health threat. Environmental reservoirs of resistance gene determinats, such as effluents of hospital wastewaters, are acquiring increased relevance in the selection of plasmid-encoded carbapenemase genes. The presence of Hg in environmental reservoirs may exert a positive selective pressure on tolerant bacteria, favoring the co-transfer of carbapenemase genes and mer operons. In our study, 63 CP-Kp isolates were screened for mer operons by whole genome sequencing (MySeq). Conjugation assays were performed with 24 out of 63 CP-Kp isolates harboring the mer operon. Ten transconjugants (Tc-Kp) were selected with Hg. Plasmid DNA of Tc-Kp was extracted and sequenced using single-molecule real-time (SMRT) technology (PacBio, Sequel II system) with later annotation. Plasmid analysis revealed that Tc-Kp from blaIMP-like (n = 3) showed a single plasmid belonging to IncC group with two complete mer operon next to blaIMP-like. Tc-Kp from blaVIM-1 (n = 2) harbored two plasmids, one with blaVIM-1 in an IncL, and mer operon was in an IncFIB plasmid. Tc-Kp from blaOXA-48-like (n = 5) showed 2 plasmids. blaOXA-48-like was found in an IncL plasmid, whereas mer operon was (i) in an IncR plasmid associated with blaCTX-M-15 in 3 Tc-Kp-OXA-48-like, (ii) in an IncC plasmid associated with blaCMY-2 in 1 Tc-Kp-OXA-48-like, (iii) and in an IncFIB plasmid associated with blaCTX-M-15 in 1 Tc-Kp-OXA-48-like. This is, to our knowledge, the first study to describe in K. pneumoniae producing plasmid-encoded carbapenemase, the potential impact of Hg in the co-transfer of mer operons and carbapenemase genes located in the same or different plasmids.
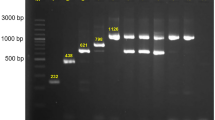
Graphical abstract

Key points
• Environmental reservoirs are playing an important role in the selection of carbapenemase genes.
• Conjugation assays, selecting with Hg, obtained 10 transconjugants with carbapenemase genes.
• mer operons were located in the same or different plasmids than carbapenemase genes.



Similar content being viewed by others
Availability of data and material
Illumina and PacBio sequence data of the 24 CP-Kp harboring plasmids of bla carbapenemase and mer operon are freely available from the NCBI BioProject database (https://www.ncbi.nlm.nih.gov/bioproject/) under accession number PRJNA738337.
Code availability
Not applicable.
References
Boyd E, Barkay T (2012) The mercury resistance operon: from an origin in a geothermal environment to an efficient detoxification machine. Front Microbiol 3:349
Cahill N, O’Connor L, Mahon B, Varley Á, McGrath E, Ryan P, Morris D (2019) Hospital effluent: a reservoir for carbapenemase-producing Enterobacterales? Sci Total Environ 672:618–624
Castanheira M, Deshpande LM, Mendes RE, Canton R, Sader HS, Jones RN (2019) Variations in the occurrence of resistance phenotypes and carbapenemase genes among Enterobacteriaceae isolates in 20 years of the SENTRY Antimicrobial Surveillance Program. Open Forum Infect Dis 6(Suppl. 1):S23–S33
Doyle D, Peirano G, Lascols C, Lloyd T, Church DL, Pitout JD (2012) Laboratory detection of Enterobacteriaceae that produce carbapenemases. J Clin Microbiol 50(12):3877–3880
Essa AM, Julian DJ, Kidd SP, Brown NL, Hobman JL (2003) Mercury resistance determinants related to Tn21, Tn1696, and Tn5053 in Enterobacteria from the preantibiotic era. Antimicrob Agents Chemother 47(3):1115–1119
European Committee for Standardization. Reference method for testing the in vitro activity of antimicrobial agents against rapidly growing aerobic bacteria involved in infectious diseases, ISO 20776–1:2006. European Committee For Standardization, Brussels, Belgium, 2006
Finley PJ, Norton R, Austin C, Mitchell A, Zank S, Durham P (2015) Unprecedented silver resistance in clinically isolated Enterobacteriaceae: major implications for burn and wound management. Antimicrob Agents Chemother 59:4734–4741
Gullberg E, Albrecht LM, Karlsson C, Sandegren L, Andersson DI (2014) Selection of a multidrug resistance plasmid by sublethal levels of antibiotics and heavy metals. Mbio 5(5):e01918-e2014
Hua X, Liang Q, Deng M, He J, Wang M, Hong W, Chen H (2021) BacAnt: a combination annotation server for bacterial DNA sequences to identify antibiotic resistance genes, integrons, and transposable elements. Front Microbiol. https://doi.org/10.3389/fmicb.2021.649969
Jutkina J, Marathe NP, Flach CF, Larsson DGJ (2018) Antibiotics and common antibacterial biocides stimulate horizontal transfer of resistance at low concentrations. Sci Total Environ 616:172–178
Kaushik M, Kumar S, Kapoor RK (2018) Integrons in Enterobacteriaceae: diversity, distribution and epidemiology. Int J Antimicrob Agents 51(2):167–176
Kholodii GY, Yurieva OV, Lomovskaya OL, Gorlenko ZM, Mindlin SZ, Nikiforov VG (1993) Tn5053, a mercury resistance transposon with integron’s ends. J Mol Biol 230:1103–1107
Kholodii GY, Mindlin SZ, Bass IA, Yurieva OV, Minakhina SV, Nikiforov VG (1995) Four genes, two ends, and a res region are involved in transposition of Tn5053: a paradigm for a novel family of transposons carrying either a mer operon or an integron. Mol Microbiol 17(6):1189–1200
Kieser T (1984) Factors affecting the isolation of CCC DNA from Streptomyces lividans and Escherichia coli. Plasmid 12(1):19–36
Kremer AN, Hoffmann H (2012) Subtractive hybridization yields a silver resistance determinant unique to nosocomial pathogens in the Enterobacter cloacae complex. J Clin Microbiol 50:3249–3257
Laffite A, Kilunga PI, Kayembe JM, Devarajan N, Mulaji CK, Giuliani G, Pote J (2016) Hospital effluents are one of several sources of metal, antibiotic resistance genes, and bacterial markers disseminated in Sub-Saharan urban rivers. Front Microbiol 7:112
Lam MM, Wick RR, Wyres KL, Gorrie CL, Judd LM, Jenney AW, Holt KE (2018) Genetic diversity, mobilisation and spread of the yersiniabactin-encoding mobile element ICEKp in Klebsiella pneumoniae populations. Microb Genom 4(9):e000196
Larsen MV, Cosentino S, Rasmussen S, Friis C, Hasman H, Friis C, Hasman H, Marvig RL, Lund O (2012) Multilocus sequence typing of total genome sequenced bacteria. J Clin Micobiol 50:1355–1361. https://doi.org/10.1128/JCM.06094-11
Li P, Yang Y, Xiong W (2015) Impacts of mercury pollution controls on atmospheric mercury concentration and occupational mercury exposure in a hospital. Biol Trace Elem Res 168(2):330–334
Long H, Feng Y, Ma K, Liu L, McNally A, Zong, Z (2019) The co-transfer of plasmid-borne colistin-resistant genes mcr-1 and mcr-3.5, the carbapenemase gene blaNDM-5 and the 16S methylase gene rmtB from Escherichia coli. Sci Rep 9(1):1–6
López-Cerero L, Egea P, Gracia-Ahufinger I, González-Padilla M, Rodríguez-López F, Rodríguez-Baño J, Pascual A (2014) Characterisation of the first ongoing outbreak due to KPC-3-producing Klebsiella pneumoniae (ST512) in Spain. Int J Antimicrob Agents 44(6):538–540
Martínez JR, Díaz-de Alba P, Ruiz-Carrascoso G, Gomez-Gil R, Pascual A (2014) Presence of quinolone resistance to qnrB1 genes and blaOXA-48 carbapenemase in clinical isolates of Klebsiella pneumoniae in Spain. Enferm Infecc Microbiol Clin 32(7):441–442
Mills MC, Lee J (2019) The threat of carbapenem-resistant bacteria in the environment: evidence of widespread contamination of reservoirs at a global scale. Environ Pollut 255:113143
Navon-Venezia S, Kondratyeva K, Carattoli A (2017) Klebsiella pneumoniae: a major worldwide source and shuttle for antibiotic resistance. FEMS Microbiol Rev 41(3):252–275
Nordmann P, Naas T, Poirel L (2011) Global spread of carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis 17(10):1791
Oliveira TS, Al Aukidy M, Verlicchi P (2017) Occurrence of common pollutants and pharmaceuticals in hospital effluents. In: Verlicchi P (ed) Hospital Wastewaters. The Handbook of Environmental Chemistry. Springer, Cham, pp 17–32
Oteo J, Saez D, Bautista V, Fernández-Romero S, Hernández-Molina JM, Pérez-Vázquez M, Campos J (2013) Carbapenemase-producing Enterobacteriaceae in Spain in 2012. Antimicrob Agents Chemother 57(12):6344–6347
Pal C, Bengtsson-Palme J, Kristiansson E, Larsson DJ (2015) Co-occurrence of resistance genes to antibiotics, biocides and metals reveals novel insights into their co-selection potential. BMC Genomics 16(1):964
Parkes LO, Hota SS (2018) Sink-related outbreaks and mitigation strategies in healthcare facilities. Curr Infect Dis Rep 20(10):42
Rodrigues C, Machado E, Ramos H, Peixe NÂ (2014) Expansion of ESBL-producing Klebsiella pneumoniae in hospitalized patients: a successful story of international clones (ST15, ST147, ST336) and epidemic plasmids (IncR, IncFIIK). Int J Med Microbiol 304(8):1100–1108
Rustam I, Aminov RI, Mackie RI (2007) Evolution and ecology of antibiotic resistance genes. FEMS Microbiol Lett 271(2):147–161
Sandegren L, Linkevicius M, Lytsy B, Melhus Å, Andersson DI (2012) Transfer of an Escherichia coli ST131 multiresistance cassette has created a Klebsiella pneumoniae-specific plasmid associated with a major nosocomial outbreak. J Antimicrob Chemother 67:74–83
Seemann T (2014) Prokka: rapid prokaryotic genome annotation. Bioinform 30(14):2068–2069
Skurnik D, Ruimy R, Read D, Ruppe E, Bernede-Bauduin C, Djossou F, Andremont A (2010) Is exposure to mercury a driving force for the carriage of antibiotic resistance genes? J Med Microbiol 59(7):804–807
Solgi H, Nematzadeh S, Giske CG, Badmasti F, Westerlund F, Lin YL, Shahcheraghi F (2020) Molecular epidemiology of OXA-48 and NDM-1 producing Enterobacterales species at a University Hospital in Tehran, Iran, between 2015 and 2016. Front Microbiol 11:936
Streets DG, Horowitz HM, Jacob DJ, Lu Z, Levin L, Ter Schure AF, Sunderland EM (2017) Total mercury released to the environment by human activities. Environ Sci Technol 51(11):5969–5977
Suleyman G, Alangaden G, Bardossy AC (2018) The role of environmental contamination in the transmission of nosocomial pathogens and healthcare-associated infections. Curr Infect Dis Rep 20(6):12
Sütterlin S, Téllez-Castillo CJ, Anselem L, Yin H, Bray JE, Maiden MC (2018) Heavy metal susceptibility of Escherichia coli isolated from urine samples from Sweden, Germany, and Spain. Antimicrob Agents Chemother 62(5):e00209-e218
Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, Mickelsen PA, Murray BE, Persing DH, Swaminathan B (1995) Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol 33:2233
Vergara-López S, Domínguez MC, Conejo MC, Pascual Á, Rodríguez-Baño J (2013) Wastewater drainage system as an occult reservoir in a protracted clonal outbreak due to metallo-β-lactamase-producing Klebsiella oxytoca. Clin Microbiol Infect 19(11):E490–E498
Verlicchi P, Galletti A, Petrovic M, Barceló D (2010) Hospital effluents as a source of emerging pollutants: an overview of micropollutants and sustainable treatment options. J Hydrol 389(3–4):416–428
Woodford N, Turton JF, Livermore DM (2011) Multiresistant Gram-negative bacteria: the role of high-risk clones in the dissemination of antibiotic resistance. FEMS Microbiol Rev 35(5):736–755
Yang QE, Agouri SR, Tyrrell JM, Yang QE, Agouri SR, Tyrrell JM, Walsh TR (2018) Heavy metal resistance genes are associated with blaNDM-1 and blaCTX-M-15 carrying Enterobacteriaceae. Antimicrob Agents Chemother 62(5):e02642-e2717
Yuan L, Li ZH, Zhang MQ, Shao W, Fan YY, Sheng GP (2019) Mercury/silver resistance genes and their association with antibiotic resistance genes and microbial community in a municipal wastewater treatment plant. Sci Total Environ 657:1014–1022
Zhang Y, Gu AZ, Cen T, Li X, He M, Li D, Chen J (2018) Sub-inhibitory concentrations of heavy metals facilitate the horizontal transfer of plasmid-mediated antibiotic resistance genes in water environment. Environ Pollut 237:74–82
Zhu Y, Zhang W, Schwarz S, Wang C, Liu W, Chen F, Liu S (2019) Characterization of a blaIMP-4-carrying plasmid from Enterobacter cloacae of swine origin. J Antimicrob Chemother 74(7):1799–1806
Funding
This work was supported by the Ministerio de Sanidad y Consumo, Instituto de Salud Carlos III (project PI15-01172), and the Instituto de Salud Carlos III, Subdirección General de Redes y Centros de Investigación Cooperativa, Ministerio de Economía y Competitividad, the Spanish Network for Research in Infectious Diseases (REIPI RD12/0015) co-financed by European Development Regional Fund “A way to achieve Europe” ERDF.
Author information
Authors and Affiliations
Contributions
PPP wrote the paper, designed the study, and performed research, MDV and AGT performed the research and analyzed data, JOI contributed new methods, and AP and FFC review the manuscript and conceived and designed research.
Corresponding author
Ethics declarations
Ethical statement
This material is the authors’ own original work, which has not been previously published elsewhere. The paper is not currently being considered for publication elsewhere. The paper properly credits the meaningful contributions of co-authors and co-researchers. All authors have been personally and actively involved in substantial work leading to the paper and will take public responsibility for its content.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Perez-Palacios, P., Delgado-Valverde, M., Gual-de-Torrella, A. et al. Co-transfer of plasmid-encoded bla carbapenemases genes and mercury resistance operon in high-risk clones of Klebsiella pneumoniae. Appl Microbiol Biotechnol 105, 9231–9242 (2021). https://doi.org/10.1007/s00253-021-11684-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00253-021-11684-2