Abstract
Purpose
This study aimed to analyse the molecular imaging (MI) phenotype of typical carcinoid (TC) and atypical carcinoid (AC) by 68Ga-DOTATATE (GaTATE) and 18F-FDG (FDG) PET/CT with the emphasis on its potential theranostic implications for peptide receptor radionuclide therapy (PRRT).
Methods
Retrospective review of patients with biopsy-proven TC or AC undergoing both GaTATE and FDG PET/CT at presentation. Based on correlative CT or MRI, positive lesions on either scan were defined by uptake above liver parenchyma. Per patient MI phenotypic pattern was classified as score 1, if all lesions were negative on both scans; score 2, if all were GaTATE positive/FDG negative; score 3, if all lesions were GaTATE positive but some or all were also FDG positive and score 4, if there were any GaTATE negative/FDG positive lesions. Scores 1 and 4 were deemed unsuitable for PRRT.
Results
Of 56 patients (median age 66.5 years, 32 female), 22 had TC, and 34 had AC. Distant metastases were seen in 32% of TC and 94% of AC. At a median follow-up of 37 months for TC and 38 months for AC, 100% and 63% were alive, respectively. Median OS for AC was 56 months (95% CI 43, not reached [NR]), and TC was NR. On inter-patient dual-tracer analysis, scores 1, 2, 3 and 4 were 23%, 18%, 36% and 23% in TC and 3%, 15%, 32% and 50% in AC, respectively. In 16 patients (score 2, N = 3; score 3, N = 12; score 4, N = 1) who were treated with PRRT, disease control rate at 3 months and OS were, 85% and 54.6 months (95% CI 44–70), respectively.
Conclusions
TC and AC showed a wide inter-patient phenotypic heterogeneity on GaTATE and FDG with around half of patients (46% TC and 53% AC) having an unsuitable phenotype for PRRT. Dual-tracer MI phenotype can be used to select the most suitable patients for PRRT.







Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Oberg K, Hellman P, Ferolla P, Papotti M, Group EGW. Neuroendocrine bronchial and thymic tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(Suppl 7):vii120–3. https://doi.org/10.1093/annonc/mds267.
Travis WD, Rush W, Flieder DB, Falk R, Fleming MV, Gal AA, et al. Survival analysis of 200 pulmonary neuroendocrine tumors with clarification of criteria for atypical carcinoid and its separation from typical carcinoid. Am J Surg Pathol. 1998;22:934–44. https://doi.org/10.1097/00000478-199808000-00003.
Travis WD. Lung tumours with neuroendocrine differentiation. Eur J Cancer. 2009;45(Suppl 1):251–66. https://doi.org/10.1016/S0959-8049(09)70040-1.
Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, et al. The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015;10:1243–60. https://doi.org/10.1097/JTO.0000000000000630.
Garg R, Bal A, Das A, Singh N, Singh H. Proliferation marker (Ki67) in sub-categorization of neuroendocrine tumours of the lung. Turk Patoloji Derg. 2019;35:15–21. https://doi.org/10.5146/tjpath.2018.01436.
Pelosi G, Sonzogni A, Harari S, Albini A, Bresaola E, Marchio C, et al. Classification of pulmonary neuroendocrine tumors: new insights. Transl Lung Cancer Res. 2017;6:513–29. https://doi.org/10.21037/tlcr.2017.09.04.
Hann CL, Forde PM. Lung and thymic carcinoids. Endocrinol Metab Clin N Am. 2018;47:699–709. https://doi.org/10.1016/j.ecl.2018.04.011.
Gugger M, Burckhardt E, Kappeler A, Hirsiger H, Laissue JA, Mazzucchelli L. Quantitative expansion of structural genomic alterations in the spectrum of neuroendocrine lung carcinomas. J Pathol. 2002;196:408–15. https://doi.org/10.1002/path.1065.
Reubi JC, Waser B. Concomitant expression of several peptide receptors in neuroendocrine tumours: molecular basis for in vivo multireceptor tumour targeting. Eur J Nucl Med Mol Imaging. 2003;30:781–93. https://doi.org/10.1007/s00259-003-1184-3.
Melosky B. Advanced typical and atypical carcinoid tumours of the lung: management recommendations. Curr Oncol. 2018;25:S86–93. https://doi.org/10.3747/co.25.3808.
Pusceddu S, Lo Russo G, Macerelli M, Proto C, Vitali M, Signorelli D, et al. Diagnosis and management of typical and atypical lung carcinoids. Crit Rev Oncol Hematol. 2016;100:167–76. https://doi.org/10.1016/j.critrevonc.2016.02.009.
Kabasakal L, Demirci E, Ocak M, Decristoforo C, Araman A, Ozsoy Y, et al. Comparison of (6)(8)Ga-DOTATATE and (6)(8)Ga-DOTANOC PET/CT imaging in the same patient group with neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2012;39:1271–7. https://doi.org/10.1007/s00259-012-2123-y.
Velikyan I, Sundin A, Sorensen J, Lubberink M, Sandstrom M, Garske-Roman U, et al. Quantitative and qualitative intrapatient comparison of 68Ga-DOTATOC and 68Ga-DOTATATE: net uptake rate for accurate quantification. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2014;55:204–10. https://doi.org/10.2967/jnumed.113.126177.
Hofman MS, Kong G, Neels OC, Eu P, Hong E, Hicks RJ. High management impact of Ga-68 DOTATATE (GaTate) PET/CT for imaging neuroendocrine and other somatostatin expressing tumours. J Med Imaging Radiat Oncol. 2012;56:40–7. https://doi.org/10.1111/j.1754-9485.2011.02327.x.
Hicks RJ. Use of molecular targeted agents for the diagnosis, staging and therapy of neuroendocrine malignancy. Cancer Imaging. 2010;10 Spec no A:S83–91. doi:https://doi.org/10.1102/1470-7330.2010.9007.
Lococo F, Treglia G, Cesario A, Paci M, Filice A, Versari A, et al. Functional imaging evaluation in the detection, diagnosis, and histologic differentiation of pulmonary neuroendocrine tumors. Thorac Surg Clin. 2014;24:285–92. https://doi.org/10.1016/j.thorsurg.2014.04.004.
Treglia G, Giovanella L, Lococo F. Evolving role of PET/CT with different tracers in the evaluation of pulmonary neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2014;41:853–5. https://doi.org/10.1007/s00259-014-2695-9.
Hofman MS, Lau WF, Hicks RJ. Somatostatin receptor imaging with 68Ga DOTATATE PET/CT: clinical utility, normal patterns, pearls, and pitfalls in interpretation. Radiographics : a review publication of the Radiological Society of North America, Inc. 2015;35:500–16. https://doi.org/10.1148/rg.352140164.
Van Essen M, Krenning EP, De Jong M, Valkema R, Kwekkeboom DJ. Peptide receptor radionuclide therapy with radiolabelled somatostatin analogues in patients with somatostatin receptor positive tumours. Acta Oncol. 2007;46:723–34. https://doi.org/10.1080/02841860701441848.
Hofman MS, Hicks RJ. Changing paradigms with molecular imaging of neuroendocrine tumors. Discov Med. 2012;14:71–81.
Werner RA, Weich A, Kircher M, Solnes LB, Javadi MS, Higuchi T, et al. The theranostic promise for neuroendocrine tumors in the late 2010s - where do we stand, where do we go? Theranostics. 2018;8:6088–100. https://doi.org/10.7150/thno.30357.
Hofman MS, Hicks RJ. Peptide receptor radionuclide therapy for neuroendocrine tumours: standardized and randomized, or personalized? Eur J Nucl Med Mol Imaging. 2014;41:211–3. https://doi.org/10.1007/s00259-013-2621-6.
Kong G, Grozinsky-Glasberg S, Hofman MS, Akhurst T, Meirovitz A, Maimon O, et al. Highly favourable outcomes with peptide receptor radionuclide therapy (PRRT) for metastatic rectal neuroendocrine neoplasia (NEN). Eur J Nucl Med Mol Imaging. 2019;46:718–27. https://doi.org/10.1007/s00259-018-4196-8.
Carideo L, Prosperi D, Panzuto F, Magi L, Pratesi MS, Rinzivillo M, et al. Role of combined [(68)Ga]Ga-DOTA-SST analogues and [(18)F]FDG PET/CT in the management of GEP-NENs: a systematic review. J Clin Med. 2019;8. https://doi.org/10.3390/jcm8071032.
Pattison DA, MacFarlane LL, Callahan J, Kane EL, Akhurst T, Hicks RJ. Personalised insulin calculator enables safe and effective correction of hyperglycaemia prior to FDG PET/CT. EJNMMI Res. 2019;9:15. https://doi.org/10.1186/s13550-019-0480-2.
Barrington SF, Mikhaeel NG, Kostakoglu L, Meignan M, Hutchings M, Mueller SP, et al. Role of imaging in the staging and response assessment of lymphoma: consensus of the international conference on malignant lymphomas imaging working group. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014;32:3048–58. https://doi.org/10.1200/JCO.2013.53.5229.
Kong G, Callahan J, Hofman MS, Pattison DA, Akhurst T, Michael M, et al. High clinical and morphologic response using (90)Y-DOTA-octreotate sequenced with (177)Lu-DOTA-octreotate induction peptide receptor chemoradionuclide therapy (PRCRT) for bulky neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2017;44:476–89. https://doi.org/10.1007/s00259-016-3527-x.
Hubble D, Kong G, Michael M, Johnson V, Ramdave S, Hicks RJ. 177Lu-octreotate, alone or with radiosensitising chemotherapy, is safe in neuroendocrine tumour patients previously treated with high-activity 111In-octreotide. Eur J Nucl Med Mol Imaging. 2010;37:1869–75. https://doi.org/10.1007/s00259-010-1483-4.
Hicks RJ, Kwekkeboom DJ, Krenning E, Bodei L, Grozinsky-Glasberg S, Arnold R, et al. ENETS consensus guidelines for the standards of care in neuroendocrine neoplasia: peptide receptor radionuclide therapy with radiolabeled somatostatin analogues. Neuroendocrinology. 2017;105:295–309. https://doi.org/10.1159/000475526.
Kong G, Johnston V, Ramdave S, Lau E, Rischin D, Hicks RJ. High-administered activity in-111 octreotide therapy with concomitant radiosensitizing 5FU chemotherapy for treatment of neuroendocrine tumors: preliminary experience. Cancer Biother Radiopharm. 2009;24:527–33. https://doi.org/10.1089/cbr.2009.0644.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
Lococo F, Perotti G, Cardillo G, De Waure C, Filice A, Graziano P, et al. Multicenter comparison of 18F-FDG and 68Ga-DOTA-peptide PET/CT for pulmonary carcinoid. Clin Nucl Med. 2015;40:e183–9. https://doi.org/10.1097/RLU.0000000000000641.
Ianniello A, Sansovini M, Severi S, Nicolini S, Grana CM, Massri K, et al. Peptide receptor radionuclide therapy with (177)Lu-DOTATATE in advanced bronchial carcinoids: prognostic role of thyroid transcription factor 1 and (18)F-FDG PET. Eur J Nucl Med Mol Imaging. 2016;43:1040–6. https://doi.org/10.1007/s00259-015-3262-8.
Sabet A, Haug AR, Eiden C, Auernhammer CJ, Simon B, Bartenstein P, et al. Efficacy of peptide receptor radionuclide therapy with (177)Lu-octreotate in metastatic pulmonary neuroendocrine tumors: a dual-centre analysis. American journal of nuclear medicine and molecular imaging. 2017;7:74–83.
Parghane RV, Talole S, Prabhash K, Basu S. Clinical response profile of metastatic/advanced pulmonary neuroendocrine tumors to peptide receptor radionuclide therapy with 177Lu-DOTATATE. Clin Nucl Med. 2017;42:428–35. https://doi.org/10.1097/RLU.0000000000001639.
Brabander T, van der Zwan WA, Teunissen JJM, Kam BLR, Feelders RA, de Herder WW, et al. Long-term efficacy, survival, and safety of [(177)Lu-DOTA(0),Tyr(3)]octreotate in patients with gastroenteropancreatic and bronchial neuroendocrine tumors. Clinical cancer research : an official journal of the American Association for Cancer Research. 2017;23:4617–24. https://doi.org/10.1158/1078-0432.CCR-16-2743.
Panagiotidis E, Alshammari A, Michopoulou S, Skoura E, Naik K, Maragkoudakis E, et al. Comparison of the impact of 68Ga-DOTATATE and 18F-FDG PET/CT on clinical management in patients with neuroendocrine tumors. J Nucl Med. 2017;58:91–6. https://doi.org/10.2967/jnumed.116.178095.
Zhang P, Yu J, Li J, Shen L, Li N, Zhu H, et al. Clinical and prognostic value of PET/CT imaging with combination of (68)Ga-DOTATATE and (18)F-FDG in gastroenteropancreatic neuroendocrine neoplasms. Contrast Media Mol Imaging. 2018;2018:2340389. https://doi.org/10.1155/2018/2340389.
Jiang Y, Hou G, Cheng W. The utility of 18F-FDG and 68Ga-DOTA-Peptide PET/CT in the evaluation of primary pulmonary carcinoid: a systematic review and meta-analysis. Medicine (Baltimore). 2019;98:e14769. https://doi.org/10.1097/MD.0000000000014769.
Hindie E. The NETPET score: combining FDG and somatostatin receptor imaging for optimal management of patients with metastatic well-differentiated neuroendocrine tumors. Theranostics. 2017;7:1159–63. https://doi.org/10.7150/thno.19588.
Chan DL, Pavlakis N, Schembri GP, Bernard EJ, Hsiao E, Hayes A, et al. Dual somatostatin receptor/FDG PET/CT imaging in metastatic neuroendocrine tumours: proposal for a novel grading scheme with prognostic significance. Theranostics. 2017;7:1149–58. https://doi.org/10.7150/thno.18068.
Bahri H, Laurence L, Edeline J, Leghzali H, Devillers A, Raoul JL, et al. High prognostic value of 18F-FDG PET for metastatic gastroenteropancreatic neuroendocrine tumors: a long-term evaluation. J Nucl Med. 2014;55:1786–90. https://doi.org/10.2967/jnumed.114.144386.
Ramirez RA, Beyer DT, Diebold AE, Voros BA, Chester MM, Wang YZ, et al. Prognostic factors in typical and atypical pulmonary carcinoids. Ochsner J. 2017;17:335–40.
Chan DL, Bernard E, Schembri G, Roach P, Johnson M, Pavlakis N, et al. High metabolic tumour volume on FDG PET predicts poor survival from neuroendocrine neoplasms. Neuroendocrinology. 2019. https://doi.org/10.1159/000504673.
Tirosh A, Papadakis GZ, Millo C, Hammoud D, Sadowski SM, Herscovitch P, et al. Prognostic utility of total (68)Ga-DOTATATE-avid tumor volume in patients with neuroendocrine tumors. Gastroenterology. 2018;154:998–1008 e1. https://doi.org/10.1053/j.gastro.2017.11.008.
Hope TA, Calais J, Zhang L, Dieckmann W, Millo C. (111)In-pentetreotide scintigraphy versus (68)Ga-DOTATATE PET: impact on Krenning scores and effect of tumor burden. J Nucl Med. 2019;60:1266–9. https://doi.org/10.2967/jnumed.118.223016.
Gotthardt M, Behe MP, Grass J, Bauhofer A, Rinke A, Schipper ML, et al. Added value of gastrin receptor scintigraphy in comparison to somatostatin receptor scintigraphy in patients with carcinoids and other neuroendocrine tumours. Endocr Relat Cancer. 2006;13:1203–11. https://doi.org/10.1677/erc.1.01245.
Funding
This work was partly funded by the Peter Mac Foundation and supported by an NHMRC Practitioner Fellowship of the Australian Health and Medical Research Foundation to Professor Hicks (APP1108050).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study concept and design. Material preparation, data collection, and analysis were performed by LZ, AI, GK, TA, MM and RJH. The first draft of the manuscript was written by LZ and AI, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest relevant to this paper.
Ethical approval
Ethical approval was granted by the local Ethics Committee of Peter MacCallum Cancer Centre (Peter Mac Project No: 19/214R). In view of the retrospective nature of the study and all the procedures being performed were part of the routine care; the individual patient consent was waived by the Ethics Committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology - Chest
Lamiaa Zidan and Amir Iravani are co-first authors
Electronic supplementary material
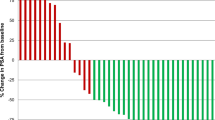
Supplementary Fig. 1
Inter-patient dual tracer scoring (a) in typical and atypical carcinoid. Comparison between GaTATE SUVmax (b) and FDG SUVmax (c) in typical and atypical carcinoid patients (JPG 168 kb)
Rights and permissions
About this article
Cite this article
Zidan, L., Iravani, A., Kong, G. et al. Theranostic implications of molecular imaging phenotype of well-differentiated pulmonary carcinoid based on 68Ga-DOTATATE PET/CT and 18F-FDG PET/CT. Eur J Nucl Med Mol Imaging 48, 204–216 (2021). https://doi.org/10.1007/s00259-020-04915-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-020-04915-7