Abstract
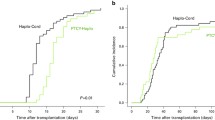
Haploidentical related (Haplo) and umbilical cord blood (UCB) donors are the main “alternative donor” options for allogeneic hematopoietic stem cell transplantation (HCT) for patients without identical donor. At our institution, UCB was the main alternative donor type until 2013, when HaploHCT was introduced as the preferred procedure. A common myeloablative conditioning regimen was used, based on thiotepa, busulfan, and fludarabine. We analyze the outcomes of 47 patients (61%) who received a single UCB transplantation (UCBT) and 30 patients (39%) who received a HaploHCT with post-transplant cyclophosphamide. No differences were found in the rate of neutrophil engraftment, whereas platelet recovery was earlier with HaploHCT. NRM was higher after UCBT at 3 months and 3 years (13% and 13% vs. 23% and 45% in HaploHCT and UCBT, respectively; p < 0.001 for both time points). The 3-year relapse incidence was 35% after HaploHCT vs. 17% after UCBT, respectively (p = 0.13). The 100-day incidence of grade 3–4 acute GVHD (3% vs. 11%) and the 3-year moderate-to-severe chronic GVHD (4% vs. 15%) did not differ between HaploHCT and UCBT, respectively (p > 0.2). There was a trend for higher overall survival at 1 and 3 years in HaploHCT recipients (69% vs. 45% and 64% vs. 38%, respectively; p = 0.055 for both time points). Despite the small sample sizes, multivariate analysis adjusted for patient age and disease status at transplant showed a better 3-year OS in HaploHCT recipients, mostly due to a lower NRM (p < 0.001). Our results support the use of HaploHCT when feasible when an identical donor is not available.


Similar content being viewed by others
References
Copelan EA (2006) Hematopoietic stem-cell transplantation. N Engl J Med 354:1813–1826
Alshemmari S, Ameen R, Gaziev J (2011) Haploidentical hematopoietic stem-cell transplantation in adults. Bone Marrow Res 2011:303487
Gragert L, Eapen M, Williams E et al (2014) HLA match likelihoods for hematopoietic stem-cell grafts in the U.S. registry. N Engl J Med 371:339–348
Ballen KK, Gluckman E, Broxmeyer HE (2013) Umbilical cord blood transplantation: the first 25 years and beyond. Blood 122(4):491–498
Slade M, Fakhri B, Savani BN, Romee R (2017) Halfway there: the past, present and future of haploidentical transplantation. Bone Marrow Transplant 52(1):1–6
Sanz J, Boluda JCH, Martín C et al (2012) Single-unit umbilical cord blood transplantation from unrelated donors in patients with hematological malignancy using busulfan, thiotepa, fludarabine and ATG as myeloablative conditioning regimen. Bone Marrow Transplant 47(10):1287–1293
O'Donnell PV, Luznik L, Jones RJ et al (2002) Nonmyeloablative bone marrow transplantation from partially HLA-mismatched related donors using post-transplantation cyclophosphamide. Biol Blood Marrow Transplant 8(7):377–386
Luznik L, O'Donnell PV, Symons HJ et al (2008) HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, post-transplantation cyclophosphamide. Biol Blood Marrow Transplant 14(6):641–650
Solomon SR, Sizemore CA, Sanacore M et al (2012) Haploidentical transplantation using T cell replete peripheral blood stem cells and myeloablative conditioning in patients with high-risk hematologic malignancies who lack conventional donors is well tolerated and produces excellent relapse-free survival: results of a prospective phase II trial. Biol Blood Marrow Transplant 18(12):1859–1866
Raiola AM, Dominietto A, Ghiso A et al (2013) Unmanipulated haploidentical bone marrow transplantation and post-transplantation cyclophosphamide for hematologic malignancies after myeloablative conditioning. Biol Blood Marrow Transplant 19(1):117–122
Bacigalupo A, Dominietto A, Ghiso A et al (2015) Unmanipulated haploidentical bone marrow transplantation and post-transplant cyclophosphamide for hematologic malignancies following a myeloablative conditioning: an update. Bone Marrow Transplant 50(Suppl 2):S37–S39
Esquirol A, Pascual MJ, Ortiz M et al (2017) Single-agent GvHD prophylaxis with tacrolimus after post-transplant high-dose cyclophosphamide is a valid option for haploidentical transplantation in adults with hematological malignancies. Bone Marrow Transplant 52(9):1273–1279
Shouval R, Nagler A (2017) From patient centered risk factors to comprehensive prognostic models: a suggested framework for outcome prediction in umbilical cord blood transplantation. Stem Cell Investig 4:39
Querol S, Rubinstein P, Marsh SG et al (2009) Cord blood banking: “providing cord blood banking for a nation”. Br J Haematol 147(2):227–235
Gratwohl A (2012) The EBMT risk score. Bone Marrow Transplant 47:749–756
Sorror ML, Storb RF, Sandmaier BM, Maziarz RT, Pulsipher MA, Maris MB et al (2014) Comorbidity-age index: a clinical measure of biologic age before allogeneic hematopoietic cell transplantation. J Clin Oncol 32:3249–3256
Sorror ML (2013) How I assess comorbidities before hematopoietic cell transplantation. Blood 121:2854–2863
Barker JN, Scaradavou A, Stevens CE (2010) Combined effect of total nucleated cell dose and HLA match on transplantation outcome in 1061 cord blood recipients with hematologic malignancies. Blood 115(9):1843–1849
Brunstein CG, Fuchs EJ, Carter SL et al (2011) Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood 118(2):282–288
Raiola AM, Dominietto A, di Grazia C et al (2014) Unmanipulated haploidentical transplants compared with other alternative donors and matched sibling grafts. Biol Blood Marrow Transplant 20(10):1573–1579
Ruggeri A, Labopin M, Sanz G et al (2015) Comparison of outcomes after unrelated cord blood and unmanipulated haploidentical stem cell transplantation in adults with acute leukemia. Leukemia 29(9):1891–1900
Giannotti F, Labopin M, Shouval R et al (2018) Haploidentical transplantation is associated with better overall survival when compared to single cord blood transplantation: an EBMT-Eurocord study of acute leukemia patients conditioned with thiotepa, busulfan and fludarabina. J Hematol Oncol 11(1):11
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA et al (1974) Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation 18(4):295–304
Terwey TH, Vega-Ruiz A, Hemmati PG, Martus P, Dietz E, le Coutre P et al (2012) NIH-defined graft-versus-host disease after reduced intensity or myeloablative conditioning in patients with acute myeloid leukemia. Leukemia 26(3):536–542
Funding
This project has been funded by La Marató de TV3 Foundation file number: 20133230. AGAUR 2017 SGR 1395 from the Catalan Government and a grant from “Obra Social La Caixa” Barcelona Spain. PERIS SLT002/16/0043 from the Catalan Government and PI17/01246 from the Instituto de Salud Carlos III, Ministerio de Economía y Competitividad, Spain. Tercel RD16/0011/0028 Instituto de Salud Carlos III, Ministerio de Economía y Competitividad, Spain, and a grant from “Fundació Bancaria La Caixa.”
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Transplant were performed according the institutional protocols, national protocols and with the 1964 Helsinki declaration. All patients signed the informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 26 kb)
Rights and permissions
About this article
Cite this article
Esquirol, A., Querol, S., Garcia-Cadenas, I. et al. When an HLA identical donor is not available in adults with hematological neoplasms: single-center comparison of single-unit cord blood transplantation and haploidentical-related PBSC transplantation with PTCy using a standardized conditioning platform (thiotepa-busulfan-fludarabine). Ann Hematol 99, 157–165 (2020). https://doi.org/10.1007/s00277-019-03870-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-019-03870-0