Abstract
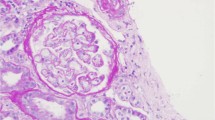
The correct diagnosis, classification and therapeutic management of thrombotic microangiopathies (TMA) continue to be a challenge for the clinician. We report a rare case of eosinophilic granulomatosis with polyangiitis (EGPA) as a trigger for complement-mediated TMA in a 57-year-old man who was successfully treated with corticoids, cyclophosphamide and therapeutic plasma exchange. Additionally, we review few other cases reported in the literature and the pathophysiological pathway of association between TMA and EGPA. We found that the mutual relationships between the inflammation triggered by vasculitis, the exacerbated complement activation, together with hypereosinophilia and endothelial damage seem to be the key in explaining the connection between both entities. We suggest that an understanding of the multi-causal nature of TMAs is crucial for the correct diagnosis and treatment of these patients.
Similar content being viewed by others
References
Greco A, Rizzo MI, De Virgilio A et al (2015) Churg-Strauss syndrome. Autoimmun Rev 14:341–348
George JN, Nester CM (2014) Syndromes of thrombotic microangiopathy. N Engl J Med 371:654–666. https://doi.org/10.1056/NEJMra1312353
Masias C, Vasu S, Cataland SR (2017) None of the above: thrombotic microangiopathy beyond TTP and HUS. Blood 129:2857–2863. https://doi.org/10.1182/blood-2016-11-743104
Scully M, Cataland S, Coppo P et al (2017) Consensus on the standardization of terminology in thrombotic thrombocytopenic purpura and related thrombotic microangiopathies. J Thromb Haemost 15:312–322. https://doi.org/10.1111/jth.13571
Åkesson A, Zetterberg E, Klintman J (2017) At the cross section of thrombotic microangiopathy and atypical hemolytic uremic syndrome: a narrative review of differential diagnostics and a problematization of nomenclature. Ther Apher Dial 21:304–319. https://doi.org/10.1111/1744-9987.12535
Masi AT, Hunder GG, Lie JT et al (1990) The American College of Rheumatology 1990 criteria for the classification of Churg–Strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheum 33:1094–1100
Gasparyan AY, Ayvazyan L, Blackmore H, Kitas GD (2011) Writing a narrative biomedical review: considerations for authors, peer reviewers, and editors. Rheumatol Int 31:1409–1417. https://doi.org/10.1007/s00296-011-1999-3
Fukui S, Iwamoto N, Tsuji S et al (2015) Eosinophilic granulomatosis with polyangiitis with thrombotic microangiopathy: is simultaneous systemic lupus erythematosus associated with clinical manifestations?: A case report and review of the literature. Medicine (Baltimore) 94:e1943. https://doi.org/10.1097/MD.0000000000001943
Cao M, Ferreiro T, Leite BN et al (2017) Two cases of atypical hemolytic uremic syndrome (aHUS) and eosinophilic granulomatosis with polyangiitis (EGPA): a possible relationship. CEN Case Rep 6:91–97. https://doi.org/10.1007/s13730-017-0251-8
Song D, Wu L, Wang F et al (2013) The spectrum of renal thrombotic microangiopathy in lupus nephritis. Arthritis Res Ther 15:R12. https://doi.org/10.1186/ar4142
Mathew RO, Nayer A, Asif A (2016) The endothelium as the common denominator in malignant hypertension and thrombotic microangiopathy. J Am Soc Hypertens 10:352–359. https://doi.org/10.1016/j.jash.2015.12.007
Fujimura Y, Matsumoto M (2010) Registry of 919 patients with thrombotic microangiopathies across Japan: database of Nara Medical University during 1998–2008. Intern Med 49:7–15
Chen S-F, Wang H, Huang Y-M et al (2015) Clinicopathologic characteristics and outcomes of renal thrombotic microangiopathy in anti-neutrophil cytoplasmic autoantibody-associated glomerulonephritis. Clin J Am Soc Nephrol 10:750–758. https://doi.org/10.2215/CJN.07910814
Rosove MH (2014) Thrombotic microangiopathies. Semin Arthritis Rheum 43:797–805. https://doi.org/10.1016/j.semarthrit.2013.11.004
van Timmeren MM, Heeringa P (2012) Pathogenesis of ANCA-associated vasculitis: recent insights from animal models. Curr Opin Rheumatol 24:8–14. https://doi.org/10.1097/BOR.0b013e32834bde57
Blanchard C, Rothenberg ME (2009) Biology of the eosinophil. Adv Immunol 101:81–121. https://doi.org/10.1016/S0065-2776(08)01003-1
Maino A, Rossio R, Cugno M et al (2012) Hypereosinophilic syndrome, Churg–Strauss syndrome and parasitic diseases: possible links between eosinophilia and thrombosis. Curr Vasc Pharmacol 10:670–675
Akuthota P, Weller PF (2015) Spectrum of eosinophilic end-organ manifestations. Immunol Allergy Clin N Am 35:403–411. https://doi.org/10.1016/j.iac.2015.04.002
Ames PRJ, Margaglione M, Mackie S, Alves JD (2010) Eosinophilia and thrombophilia in churg strauss syndrome: a clinical and pathogenetic overview. Clin Appl Thromb Hemost 16:628–636. https://doi.org/10.1177/1076029609348647
Liapis H, Ho AK, Brown D et al (2005) Thrombotic microangiopathy associated with the hypereosinophilic syndrome. Kidney Int 67:1806–1811. https://doi.org/10.1111/j.1523-1755.2005.00278.x
Yuste C, Quiroga B, Verde E et al (2012) The non-casual relation between eosinophilia and thrombotic microangiopathy. Transfus Apher Sci 47:365–367. https://doi.org/10.1016/j.transci.2012.07.021
Ohguchi H, Sugawara T, Harigae H (2009) Thrombotic thrombocytopenic purpura complicated with hypereosinophilic syndrome. Intern Med 48:1687–1690
Le Quintrec M, Roumenina L, Noris M, Frémeaux-Bacchi V (2010) Atypical hemolytic uremic syndrome associated with mutations in complement regulator genes. Semin Thromb Hemost 36:641–652. https://doi.org/10.1055/s-0030-1262886
Kavanagh D, Goodship T (2010) Genetics and complement in atypical HUS. Pediatr Nephrol 25:2431–2442. https://doi.org/10.1007/s00467-010-1555-5
Loirat C, Noris M, Fremeaux-Bacchi V (2008) Complement and the atypical hemolytic uremic syndrome in children. Pediatr Nephrol 23:1957–1972. https://doi.org/10.1007/s00467-008-0872-4
Noris M, Galbusera M, Gastoldi S et al (2014) Dynamics of complement activation in aHUS and how to monitor eculizumab therapy. Blood 124:1715–1726. https://doi.org/10.1182/blood-2014-02-558296
Xiao H, Schreiber A, Heeringa P et al (2007) Alternative complement pathway in the pathogenesis of disease mediated by anti-neutrophil cytoplasmic autoantibodies. Am J Pathol 170:52–64. https://doi.org/10.2353/ajpath.2007.060573
Xing G, Chen M, Liu G et al (2009) Complement activation is involved in renal damage in human antineutrophil cytoplasmic autoantibody associated pauci-immune vasculitis. J Clin Immunol 29:282–291. https://doi.org/10.1007/s10875-008-9268-2
Gou S-J, Yuan J, Chen M et al (2013) Circulating complement activation in patients with anti-neutrophil cytoplasmic antibody-associated vasculitis. Kidney Int 83:129–137. https://doi.org/10.1038/ki.2012.313
Manenti L, Vaglio A, Gnappi E et al (2015) Association of serum C3 concentration and histologic signs of thrombotic microangiopathy with outcomes among patients with ANCA-associated renal vasculitis. Clin J Am Soc Nephrol 10:2143–2151. https://doi.org/10.2215/CJN.00120115
Bresin E, Rurali E, Caprioli J et al (2013) Combined complement gene mutations in atypical hemolytic uremic syndrome influence clinical phenotype. J Am Soc Nephrol 24:475–486. https://doi.org/10.1681/ASN.2012090884
Kavanagh D, Goodship THJ (2011) Atypical hemolytic uremic syndrome, genetic basis, and clinical manifestations. Hematol Am Soc Hematol Educ Progr 2011:15–20. https://doi.org/10.1182/asheducation-2011.1.15
Noris M, Caprioli J, Bresin E et al (2010) Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype. Clin J Am Soc Nephrol 5:1844–1859. https://doi.org/10.2215/CJN.02210310
Vieira-Martins P, El Sissy C, Bordereau P et al (2016) Defining the genetics of thrombotic microangiopathies. Transfus Apher Sci 54:212–219. https://doi.org/10.1016/j.transci.2016.04.011
Pickering MC, de Jorge EG, Martinez-Barricarte R et al (2007) Spontaneous hemolytic uremic syndrome triggered by complement factor H lacking surface recognition domains. J Exp Med 204:1249–1256. https://doi.org/10.1084/jem.20070301
Fremeaux-Bacchi V, Fakhouri F, Garnier A et al (2013) Genetics and outcome of atypical hemolytic uremic syndrome: a nationwide French series comparing children and adults. Clin J Am Soc Nephrol 8:554–562. https://doi.org/10.2215/CJN.04760512
Servais A, Noël L-H, Roumenina LT et al (2012) Acquired and genetic complement abnormalities play a critical role in dense deposit disease and other C3 glomerulopathies. Kidney Int 82:454–464. https://doi.org/10.1038/ki.2012.63
Manenti L, Gnappi E, Vaglio A et al (2013) Atypical haemolytic uraemic syndrome with underlying glomerulopathies. A case series and a review of the literature. Nephrol Dial Transplant 28:2246–2259. https://doi.org/10.1093/ndt/gft220
Monteferrante G, Brioschi S, Caprioli J et al (2007) Genetic analysis of the complement factor H related 5 gene in haemolytic uraemic syndrome. Mol Immunol 44:1704–1708. https://doi.org/10.1016/j.molimm.2006.08.004
Westra D, Vernon KA, Volokhina EB et al (2012) Atypical hemolytic uremic syndrome and genetic aberrations in the complement factor H-related 5 gene. J Hum Genet 57:459–464. https://doi.org/10.1038/jhg.2012.57
Li A, Makar RS, Hurwitz S et al (2016) Treatment with or without plasma exchange for patients with acquired thrombotic microangiopathy not associated with severe ADAMTS13 deficiency: a propensity score-matched study. Transfusion 56:2069–2077. https://doi.org/10.1111/trf.13654
Cataland SR, Wu HM (2014) How I treat: the clinical differentiation and initial treatment of adult patients with atypical hemolytic uremic syndrome. Blood 123:2478–2484. https://doi.org/10.1182/blood-2013-11-516237
Mache CJ, Acham-Roschitz B, Frémeaux-Bacchi V et al (2009) Complement inhibitor eculizumab in atypical hemolytic uremic syndrome. Clin J Am Soc Nephrol 4:1312–1316. https://doi.org/10.2215/CJN.01090209
Legendre CM, Licht C, Muus P et al (2013) Terminal complement inhibitor eculizumab in atypical hemolytic-uremic syndrome. N Engl J Med 368:2169–2181. https://doi.org/10.1056/NEJMoa1208981
Author information
Authors and Affiliations
Contributions
All the authors have contributed to patient management and clinical procedures, have drafted and revised the manuscript and have approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
JB, NNN and JMS declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from the patient to publish this case report.
Rights and permissions
About this article
Cite this article
Badiola, J., Navarrete-Navarrete, N. & Sabio, J.M. Thrombotic microangiopathy in a patient with eosinophilic granulomatosis with polyangiitis: case-based review. Rheumatol Int 39, 359–365 (2019). https://doi.org/10.1007/s00296-018-4228-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-018-4228-5