Abstract
Objectives
To differentiate hypo-/hypertelorism (abnormal) from normal fetuses using automatic biometric measurements and machine learning (ML) classification based on MRI.
Methods
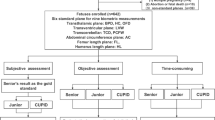
MRI data of normal (n = 244) and abnormal (n = 52) fetuses of 22–40 weeks’ gestational age (GA), scanned between March 2008 and June 2020 on 1.5/3T systems with various T2-weighted sequences and image resolutions, were included. A fully automatic method including deep learning and geometric algorithms was developed to measure the binocular (BOD), inter-ocular (IOD), ocular (OD) diameters, and ocular volume (OV). Two new parameters, BOD-ratio and IOD-ratio, were defined as the ratio between BOD/IOD relative to the sum of both globes’ OD, respectively. Eight ML classifiers were evaluated to detect abnormalities using measured and computed parameters.
Results
The automatic method yielded a mean difference of BOD = 0.70 mm, IOD = 0.81 mm, OD = 1.00 mm, and a 3D-Dice score of OV = 93.7%. In normal fetuses, all four measurements increased with GA. Constant values were detected for BOD-ratio = 1.56 ± 0.05 and IOD-ratio = 0.60 ± 0.05 across all GA and when calculated from previously published reference data of both MRI and ultrasound. A random forest classifier yielded the best results on an independent test set (n = 58): AUC-ROC = 0.941 and F1-Score = 0.711 in comparison to AUC-ROC = 0.650 and F1-Score = 0.385 achieved based on the accepted criteria that define hypo/hypertelorism based on IOD (< 5th or > 95th percentiles). Using the explainable ML method, the two computed ratios were found as the most contributing parameters.
Conclusions
The developed fully automatic method demonstrates high performance on varied clinical imaging data. The new BOD and IOD ratios and ML multi-parametric classifier are suggested to improve the differentiation of hypo-/hypertelorism from normal fetuses.
Key Points
• A fully automatic method for computing fetal ocular biometry from MRI is proposed, achieving high performance, comparable to that of an expert fetal neuro-radiologist.
• Two new parameters, IOD-ratio and BOD-ratio, are proposed for routine clinical use in ultrasound and MRI. These two ratios are constant across gestational age in normal fetuses, consistent across studies, and differentiate between fetuses with and without hypo/hypertelorism.
• Multi-parametric machine learning classification based on automatic measurements and the two new ratios improves the identification of fetal ocular anomalies beyond the accepted criteria (<5 th or >95 th IOD percentiles).






Similar content being viewed by others
Abbreviations
- BOD:
-
Binocular diameter
- GA:
-
Gestational age
- IOD:
-
Interocular diameter
- ML:
-
Machine learning
- OD:
-
Ocular diameter
- OV:
-
Ocular volume
References
Ondeck CL, Pretorius D, McCaulley J et al (2018) Ultrasonographic prenatal imaging of fetal ocular and orbital abnormalities. Surv Ophthalmol 63:745–753
Verdijk RM, Herwig-Carl MC (2020) Fetal and neonatal eye pathology. Springer Nature
Li XB, Kasprian G, Hodge JC et al (2010) Fetal ocular measurements by MRI. Prenat Diagn 30:1064–1071
Mayden KL, Tortora M, Berkowitz RL, Bracken M, Hobbins JC (1982) Orbital diameters: a new parameter for prenatal diagnosis and dating. Am J Obstet Gynecol 144:289–297
Batty R, Gawne-Cain ML, Mooney C et al (2019) Analysis of errors made on in utero MR studies of the foetal brain in the MERIDIAN study. Eur Radiol 29:195–201
Joskowicz L, Cohen D, Caplan N, Sosna J (2019) Inter-observer variability of manual contour delineation of structures in CT. Eur Radiol 29:1391–1399
Robinson AJ, Blaser S, Toi A et al (2008) MRI of the fetal eyes: morphologic and biometric assessment for abnormal development with ultrasonographic and clinicopathologic correlation. Pediatr Radiol 38:971–981
Velasco-Annis C, Gholipour A, Afacan O, Prabhu SP, Estroff JA, Warfield SK (2015) Normative biometrics for fetal ocular growth using volumetric MRI reconstruction. Prenat Diagn 35:400–408
Jeanty P, Dramaix-Wilmet M, Van Gansbeke D, Van Regemorter N, Rodesch F (1982) Fetal ocular biometry by ultrasound. Radiology 143:513–516
Odeh M, Feldman Y, Degani S, Grinin V, Ophir E, Bornstein J (2009) Fetal eyeball volume: relationship to gestational age and biparietal diameter. Prenat Diagn 29:749–752
Burns NS, Iyer RS, Robinson AJ, Chapman T (2013) Diagnostic imaging of fetal and pediatric orbital abnormalities. Am J Roentgenol 201:W797–W808
Litjens G, Kooi T, Bejnordi BE et al (2017) A survey on deep learning in medical image analysis. Med Image Anal 42:60–88
Dudovitch G, Link-Sourani D, Sira LB, Miller E, Bashat DB, Joskowicz L (2020) Deep learning automatic fetal structures segmentation in MRI scans with few annotated Datasets. In: Proc International Conference on Medical Image Computing and Computer-Assisted Intervention. Springer, pp 365–374
Ebner M, Wang G, Li W et al (2018) An automated localization, segmentation and reconstruction framework for fetal brain MRI. In: Proc International Conference on Medical Image Computing and Computer-Assisted Intervention. Springer, pp 313–320
Torrents-Barrena J, Piella G, Masoller N et al (2019) Segmentation and classification in MRI and US fetal imaging: recent trends and future prospects. Med Image Anal 51:61–88
Kojita Y, Matsuo H, Kanda T et al (2021) Deep learning model for predicting gestational age after the first trimester using fetal MRI. Eur Radiol 31:3775–3782
Avisdris N, Ben Bashat D, Ben-Sira L, Joskowicz L (2021) Fetal brain MRI measurements using a deep learning landmark network with reliability estimation. In: uncertainty for safe utilization of machine learning in medical imaging, and perinatal imaging, placental and preterm image analysis. Springer, pp 210–220
Uus A, Matthew J, Grigorescu I et al (2021) Spatio-temporal atlas of normal fetal craniofacial feature development and CNN-based ocular biometry for motion-corrected fetal MRI. Springer International Publishing, Cham, pp 168–178
Avisdris N, Yehuda B, Ben-Zvi O et al (2021) Automatic linear measurements of the fetal brain on MRI with deep neural networks. Int J Comput Assist Radiol Surg 16:1481–1492
Ronneberger O, Fischer P, Brox T (2015) U-net: Convolutional networks for biomedical image segmentation. In: Proc International Conference on Medical image computing and computer-assisted intervention. Springer, pp 234–241
He K, Zhang X, Ren S, Sun J (2016) Deep residual learning for image recognition. In: Proc IEEE conference on Computer Vision and Pattern Recognition, pp 770–778
Sudre CH, Li W, Vercauteren T, Ourselin S, Cardoso MJ (2017) Generalised dice overlap as a deep learning loss function for highly unbalanced segmentations. In: Deep learning in medical image analysis and multimodal learning for clinical decision support. Springer, pp 240–248
Smith LN (2018) A disciplined approach to neural network hyper-parameters: Part 1--learning rate, batch size, momentum, and weight decay. arXiv preprint arXiv:180309820
Deng J, Dong W, Socher R, Li L-J, Li K, Fei-Fei L (2009) Imagenet: a large-scale hierarchical image database. In: Proc IEEE conference on computer vision and pattern recognition. IEEE, pp 248–255
Frid-Adar M, Ben-Cohen A, Amer R, Greenspan H (2018) Improving the segmentation of anatomical structures in chest radiographs using u-net with an imagenet pre-trained encoder. In: Image Analysis for Moving Organ, Breast, and Thoracic Images. Springer, pp 159–168
Howard J, Gugger S (2020) fastai: a layered API for deep learning. Information 11:108
Bland JM, Altman D (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 327:307–310
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol 57:289–300
Breiman L (2001) Random forests. Mach Learn 45:5–32
Chang C-C, Lin C-J (2011) LIBSVM: a library for support vector machines. ACM Trans Intell Syst Technol (TIST) 2:1–27
Chen T, He T, Benesty M, Khotilovich V, Tang Y, Cho H (2015) Xgboost: extreme gradient boosting. R package version 04-2 1:1-4
Chawla NV, Bowyer KW, Hall LO, Kegelmeyer WP (2002) SMOTE: synthetic minority over-sampling technique. J Artif Intell Res 16:321–357
Chicco D, Jurman G (2020) The advantages of the Matthews correlation coefficient (MCC) over F1 score and accuracy in binary classification evaluation. BMC Genomics 21:1–13
Lundberg SM, Lee S-I (2017) A unified approach to interpreting model predictions. In: Proceedings of the 31st international conference on neural information processing systems, pp 4768–4777
Salomon LJ, Alfirevic Z, Berghella V et al (2011) Practice guidelines for performance of the routine mid-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol 37:116–126
American College of Radiology (2019) ACR-ACOG-AIUM-SMFM-SRU practice parameter for the performance of standard diagnostic obstetrical ultrasound. https://www.aium.org/resources/guidelines/obstetric.pdf
Whitehead MT, Vezina G (2016) Normal Developmental Globe Morphology on Fetal MR Imaging. AJNR Am J Neuroradiol 37:1733–1737
Prokopakis EP, Vlastos IM, Picavet V et al (2013) The golden ratio in facial symmetry. Rhinology 51:18–21
Abbas S (2017) Golden ratio. Resonance 22:51–60
Kuklisova-Murgasova M, Quaghebeur G, Rutherford MA, Hajnal JV, Schnabel JA (2012) Reconstruction of fetal brain MRI with intensity matching and complete outlier removal. Med Image Anal 16:1550–1564
Acknowledgements
We are grateful to Vicki Myers and Cassandra Kapoor for editorial assistance and MRI technicians for scanning the fetuses.
Funding
This study has received funding from Kamin grants 72126 and 72061 from the Israel Innovation Authority.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Dafna Ben Bashat.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Avisdris, N., Link Sourani, D., Ben-Sira, L. et al. Improved differentiation between hypo/hypertelorism and normal fetuses based on MRI using automatic ocular biometric measurements, ocular ratios, and machine learning multi-parametric classification. Eur Radiol 33, 54–63 (2023). https://doi.org/10.1007/s00330-022-08976-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08976-0