Abstract
Objectives
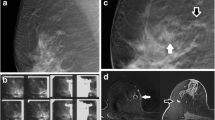
Compare prone and upright, stereotactic, and tomosynthesis-guided vacuum-assisted breast biopsies (prone DM-VABB, prone DBT-VABB, upright DM-VABB, and upright DBT-VABB) in a community-practice setting and review outcomes of ultrasound-occult architectural distortions (AD).
Methods
Consecutive biopsies performed at two community-based breast centers from 2016 to 2019 were retrospectively reviewed. Technical details of each procedure and patient outcomes were recorded. Separate analyses were performed for ultrasound-occult ADs. Two sample t-tests and Fisher’s exact test facilitated comparisons.
Results
A total of 1133 patients underwent 369 prone DM-VABB, 324 prone DBT-VABB, 437 upright DM-VABB, and 123 upright DBT-VABB with 99.2%, 100%, 99.3%, and 99.2% success, respectively (p-values > 0.25). Mean lesion targeting times were greater for prone biopsy (minutes: 6.94 prone DM-VABB, 8.54 prone DBT-VABB, 5.52 upright DM-VABB, and 5.51 upright DBT-VABB; p-values < 0.001), yielding longer total prone procedure times for prone biopsy (p < 0.001). Compared to DM-VABB, DBT-VABB used fewer exposures (p < 0.001) and more commonly targeted AD, asymmetries, or masses (p < 0.001). Malignancy rates were similar between procedures: prone DM-VABB 22.4%, prone DBT-VABB 21.9%, upright DM-VABB 22.8%, and upright DBT-VABB 17.2% (p-values > 0.19). One hundred forty of the 1133 patients underwent 145 biopsies for ultrasound-occult AD (143 DBT-VABB and 2 DM-VABB). Biopsy yielded 27 malignancies and 47 high-risk lesions (74 of 145, 51%). Malignancy rate was 20.7% after surgical upgrade of one benign-discordant and two high-risk lesions.
Conclusions
All biopsy procedure types were extremely successful. The 20.7% malignancy rate for ultrasound-occult AD confirms a management recommendation for tissue diagnosis. Upright biopsy was faster than prone biopsy, and DBT-VABB used fewer exposures than DM-VABB.
Clinical relevance
Our results highlight important differences between prone DM-VABB, prone DBT-VABB, upright DM-VABB, and upright DBT-VABB. Moreover, the high likelihood of malignancy for ultrasound-occult AD will provide confidence in recommending tissue diagnosis in lieu of observation or clinical follow-up.
Key Points
• Upright and prone stereotactic and tomosynthesis-guided breast biopsies were safe and effective in the community-practice setting.
• The malignancy rate for ultrasound-occult architectural distortion of 20.7% confirms the management recommendation for biopsy.
• Upright procedures were faster than prone procedures, and tomosynthesis-guided biopsy used fewer exposures than stereotactic biopsy.





Similar content being viewed by others
Abbreviations
- AD:
-
Architectural distortion
- DBT:
-
Digital breast tomosynthesis
- DBT-VABB:
-
Tomosynthesis-guided vacuum-assisted breast biopsy
- DM:
-
Digital mammography
- DM-VABB:
-
Stereotactic vacuum-assisted breast biopsy
References
Rafferty EA, Park JM, Philpotts LE et al (2013) Assessing radiologist performance using combined digital mammography and breast tomosynthesis compared with digital mammography alone: results of a multicenter, multireader trial. Radiology 266:104–113
Friedewald SM, Rafferty EA, Rose SL et al (2014) Breast cancer screening using tomosynthesis in combination with digital mammography. JAMA 311:2499–2507
Cohen EO, Weaver OO, Tso HH, Gerlach KE, Leung JWT (2020) Breast cancer screening via digital mammography, synthetic mammography, and tomosynthesis. Am J Prev Med 58:470–472
Skaane P, Bandos AI, Niklason LT et al (2019) Digital mammography versus digital mammography plus tomosynthesis in breast cancer screening: the Oslo Tomosynthesis Screening Trial. Radiology 291:23–30
Roth RG, Maidment ADA, Weinstein SP, Roth SO, Conant EF (2014) Digital breast tomosynthesis: lessons learned from early clinical implementation. Radiographics 34:E89-e102
Durand MA, Wang S, Hooley RJ, Raghu M, Philpotts LE (2016) Tomosynthesis-detected architectural distortion: management algorithm with radiologic-pathologic correlation. Radiographics 36:311–321
Choudhery S, Johnson MP, Larson NB, Anderson T (2021) Malignant outcomes of architectural distortion on tomosynthesis: a systematic review and meta-analysis. AJR Am J Roentgenol 217:295–303
Bahl M, Lamb LR, Lehman CD (2017) Pathologic outcomes of architectural distortion on digital 2D versus tomosynthesis mammography. AJR Am J Roentgenol 209:1162–1167
Alshafeiy TI, Nguyen JV, Rochman CM, Nicholson BT, Patrie JT, Harvey JA (2018) Outcome of architectural distortion detected only at breast tomosynthesis versus 2D mammography. Radiology 288:38–46
Ahmed SA, Samy M, Ali AM, Hassan RA (2022) Architectural distortion outcome: digital breast tomosynthesis-detected versus digital mammography-detected. Radiol Med 127:30–38
Patel BK, Covington M, Pizzitola VJ et al (2018) Initial experience of tomosynthesis-guided vacuum-assisted biopsies of tomosynthesis-detected (2D mammography and ultrasound occult) architectural distortions. AJR Am J Roentgenol 210:1395–1400
Vijayaraghavan GR, Newburg A, Vedantham S (2019) Positive predictive value of tomosynthesis-guided biopsies of architectural distortions seen on digital breast tomosynthesis and without an ultrasound correlate. J Clin Imaging Sci 9:53
Walcott-Sapp S, Garreau J, Johnson N, Thomas KA (2019) Pathology results of architectural distortion on detected with digital breast tomosynthesis without definite sonographic correlate. Am J Surg 217:857–861
Ambinder EB, Plotkin A, Euhus D et al (2021) Tomosynthesis-guided vacuum-assisted breast biopsy of architectural distortion without a sonographic correlate: a retrospective review. AJR Am J Roentgenol 217:845–854
Linda A, Tarricone R, Londero V, Girometti R, Zuiani C (2022) Pathological outcome of sonographically occult architectural distortions (AD) visible only on digital breast tomosynthesis, and comparison with AD visible also on 2D mammography. Eur J Radiol 146:110075
Omofoye TS, Martaindale S, Teichgraeber DC, Parikh JR (2017) Implementation of upright digital breast tomosynthesis-guided stereotactic biopsy. Acad Radiol 24:1451–1455
Sim LS, Kei PL (2008) Upright stereotactic vacuum-assisted needle biopsy of suspicious breast microcalcifications. J Med Imaging Radiat Oncol 52:358–364
Georgian-Smith D, D’Orsi C, Morris E, Clark CF, Liberty E, Lehman CD (2002) Stereotactic biopsy of the breast using an upright unit, a vacuum-suction needle, and a lateral arm-support system. AJR Am J Roentgenol 178:1017–1024
Kirshenbaum KJ, Voruganti T, Overbeeke C et al (2003) Stereotactic core needle biopsy of nonpalpable breast lesions using a conventional mammography unit with an add-on device. AJR Am J Roentgenol 181:527–531
Scaperrotta GP, Boffelli G, Depretto C et al (2021) Guiding vacuum-assisted biopsy in prone position: digital breast tomosynthesis vs stereotactic. Tumori 108:326–330
Schrading S, Distelmaier M, Dirrichs T et al (2015) Digital breast tomosynthesis-guided vacuum-assisted breast biopsy: initial experiences and comparison with prone stereotactic vacuum-assisted biopsy. Radiology 274:654–662
Catelli A, Santoro A, Antignani E, Venetucci P, Minelli S (2022) Safety and efficacy of tomosynthesis-guided breast biopsies in the prone position: monocentric study and review of the literature. J Cancer Res Clin Oncol 148:967–974
Weinfurtner RJ, Carter T (2021) Transition to digital breast tomosynthesis-guided biopsies: results and complications compared to stereotactic biopsies. Breast J 27:21–26
Bahl M, Maunglay M, D’Alessandro HA, Lehman CD (2019) Comparison of upright digital breast tomosynthesis-guided versus prone stereotactic vacuum-assisted breast biopsy. Radiology 290:298–304
Waldherr C, Berclaz G, Altermatt HJ et al (2016) Tomosynthesis-guided vacuum-assisted breast biopsy: A feasibility study. Eur Radiol 26:1582–1589
Bohan S, Ramli Hamid MT, Chan WY, et al (2021) Diagnostic accuracy of tomosynthesis-guided vacuum assisted breast biopsy of ultrasound occult lesions. Sci Rep 11:129
Choudhery S, Johnson M, Fazzio RT (2020) Prone versus upright digital tomosynthesis-guided biopsy. AJR Am J Roentgenol 215:760–764
Amir T, Zuckerman SP, Barufaldi B, Maidment AD, Conant EF (2021) Comparison of radiation dose between 2D digital stereotactic versus digital breast tomosynthesis-guided breast biopsies. Eur J Radiol 134:109407
Rochat CJ, Baird GL, Lourenco AP (2020) Digital mammography stereotactic biopsy versus digital breast tomosynthesis-guided biopsy: differences in biopsy targets, pathologic results, and discordance rates. Radiology 294:518–527
Weaver O, Cohen EO, Perry RE, et al (2021) Does lateral arm technique decrease the rate of clip migration in stereotactic and tomosynthesis-guided biopsies? Insights Imaging 12:193
Youk JH, Kim EK, Kim MJ et al (2011) Concordant or discordant? Imaging-pathology correlation in a sonography-guided core needle biopsy of a breast lesion. Korean J Radiol 12:232–240
Mainiero MB, Gareen IF, Bird CE, Smith W, Cobb C, Schepps B (2002) Preferential use of sonographically guided biopsy to minimize patient discomfort and procedure time in a percutaneous image-guided breast biopsy program. J Ultrasound Med 21:1221–1226
Acknowledgements
The authors thank Scientific Publications, Research Medical Library at The University of Texas MD Anderson Cancer Center and the staff of Memorial Hermann Health System, Texas Medical Center for their assistance with this article. We would also like to acknowledge support by the NIH/NCI under award number P30 CA016672.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ethan Cohen, MD.
Conflict of Interest
The authors declare no competing interests.
Statistics and Biometry
One of the authors, Jia Sun, PhD, has significant statistical expertise.
Informed Consent
Written informed consent was waived by the Institutional Review Board.
Ethical Approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Our study population overlapped with one prior study (Weaver et al, Insights into Imaging 2021;12(1):193) that compared rates of biopsy clip migration and hematoma formation during conventional and lateral-arm biopsy approach for mammographically guided breast biopsies. That study took place at one of the two breast centers included in this study (389 biopsies in 356 patients), and that study time period was August 2016 through April 2018. Our study included all consecutive mammographically guided breast biopsies performed at two breast centers from January 2016 through December 2019. Moreover, our analysis included more than just biopsy clip migration and hematoma formation.
Methodology
• Retrospective
• observational
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cohen, E.O., Korhonen, K.E., Sun, J. et al. Comparison of prone and upright, stereotactic, and tomosynthesis-guided biopsies with secondary analysis of ultrasound-occult architectural distortions. Eur Radiol 33, 6189–6203 (2023). https://doi.org/10.1007/s00330-023-09581-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09581-5