Abstract
Purpose
Off-label use of prostacyclins to manage congenital diaphragmatic hernia-associated pulmonary hypertension (CDH-PHTN) has been described over recent years, but use is not standardized across institutions. This study aims to describe trends in use of these medications in the CDH Study Group (CDHSG) patients.
Methods
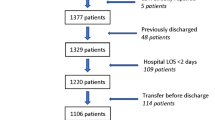
The CDHSG was queried for all patients born from 2007 to 2019. Records were reviewed to describe the number of patients receiving prostacyclins, the day of life on which the agent was started, start time relative to ECLS, the duration of medication use, and continuation of the medication at the time of discharge. Finally, trends in use by year of birth were evaluated to assess for changes in use over time.
Results
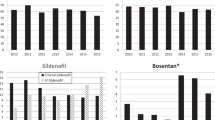
There were 6439 patients identified from the registry who were born during the study period. 4372 (68%) patients received medications to treat pulmonary hypertension. Of these, 604 (14%) received a prostacyclin at some point during their care. The median start time for prostacyclins was 7.5 days of life (mean 16.9 days, SD 32.5 days), and the median duration was 12.5 days (mean 25.1 days, SD 49.1 days). Among patients who received prostacyclins, 340 patients required ECLS during care, 53 (15.5%) of whom started the prostacyclin prior to ECLS, and 159 (46.8%) of whom started prostacyclin therapy during their ECLS run. Only a small cohort (26/604, 4.3%) required continuation of the prostacyclin at the time of discharge. The proportion of patients receiving a prostacyclin remained relatively stable over the study period.
Conclusions
While the proportion of patients receiving a prostacyclin for management of CDH-PHTN has remained relatively stable over the last 13 years, there is significant variation in timing of initiation and duration of use especially in the pre-ECLS period that warrants further investigation to describe optimal use in these patients.

Similar content being viewed by others
References
Keijzer R, Puri P (2010) Congenital diaphragmatic hernia. Semin Pediatr Surg 9:180–185
Mt H (2017) Congenital diaphragmatic hernia-associated pulmonary hypertension. Semin Pediatr Surg 26:147–153. https://doi.org/10.1053/j.sempedsurg.2017.04.008
Abman Steven H, Hansmann G, Archer Stephen L, Dunbar ID, Ian A, Chung Wendy K et al (2015) Pediatric pulmonary hypertension. Circulation 132:2037–2099. https://doi.org/10.1161/CIR.0000000000000329
Gomberg-Maitland M, Preston IR (2005) Prostacyclin therapy for pulmonary arterial hypertension: new directions. Semin Respir Crit Care Med 26:394–401. https://doi.org/10.1055/s-2005-916154
Carpentier E, Mur S, Aubry E, Pognon L, Rakza T, Flamein F et al (2017) Safety and tolerability of subcutaneous treprostinil in newborns with congenital diaphragmatic hernia and life-threatening pulmonary hypertension. J Pediatr Surg 52:1480–1483. https://doi.org/10.1016/j.jpedsurg.2017.03.058
Krishnan U, Takatsuki S, Ivy DD, Kerstein J, Calderbank M, Coleman E et al (2012) Effectiveness and safety of inhaled treprostinil for the treatment of pulmonary arterial hypertension in children. Am J Cardiol 110:1704–1709. https://doi.org/10.1016/j.amjcard.2012.07.037
Lawrence KM, Hedrick HL, Monk HM, Herkert L, Waqar LN, Hanna BD et al (2018) Treprostinil improves persistent pulmonary hypertension associated with congenital diaphragmatic hernia. J Pediatr 200:44–49. https://doi.org/10.1016/j.jpeds.2018.04.052
Olson E, Lusk LA, Fineman JR, Robertson L, Keller RL (2015) Short-term treprostinil use in infants with congenital diaphragmatic hernia following repair. J Pediatr 167:762–764. https://doi.org/10.1016/j.jpeds.2015.06.016
Skarda DE, Yoder BA, Anstadt EE, Lally PA, Greene T, McFadden M et al (2015) Epoprostenol does not affect mortality in neonates with congenital diaphragmatic hernia. Eur J Pediatr Surg 25:454–459. https://doi.org/10.1055/s-0034-1389096
Galiè N, Manes A, Branzi A (2003) Prostanoids for pulmonary arterial hypertension. Am J Respir Med 2:123–137. https://doi.org/10.1007/BF03256644
Acknowledgements
Data for this study were obtained from the CDH Study Group. The following institutions contributed data: Alberta Children’s Hospital, Arkansas Children’s Hospital, Astrid Lindgren Children’s Hospital, BC Children’s & Women’s Health Centre, Cairo University Pediatric Hospital, Chiba University Hospital, Children’s Hospital Colorado, Childrens Hospital at Skanes University Hospital, Children’s Hospital Boston, Children’s Hospital of Akron, Children’s Hospital of Georgia-AU Health, Children’s Hospital of Illinois at OSF St. Francis Medical Center, Children’s Hospital of Los Angeles, Children’s Hospital of Orange County, Children’s Hospital of Wisconsin, Children’s Hospital of Omaha, Children’s Hospital of Bonn, Children’s Hospitals and Clinics (Minneapolis), Children’s Memorial Hermann Hospital, Children’s of Alabama, Cincinnati Children’s Hospital Medical Center, Dell Children’s Medical Center of Central Texas, Duke University Medical Center, Golisano Children’s Hospital at Strong, Hospital Clinico Universidad Católica de Chile, IRCSSS Fondazione Ca’ Granda Ospedale Maggiore Policlinico, James Whitcomb Riley Children’s Hospital, Johns Hopskins All Children’s Hospital, Johns Hopkins Hospital, Juan P. Garrahan Children Hospital, Juntendo University Hospital, Juntendo University Urayasu Hospital, Kanagawa Children’s Medical Center, Kindai University Hospital, Kobe Children’s Hospital, Kyoto Prefectural University of Medicine, Kyusyu University Hospital, La Paz University Hospital, Le Bonheur Children’s Medical Center, Loma Linda University Children’s Hospital, Lucile Salter Packard Children’s Hospital, Manchester University Hospitals, Mattel Children’s Hospital at UCLA, Medical University of South Carolina, Mie University School of Medicine Hospital, Nagoya University Hospital, National Center for Child Health and Development, NICU Health Sciences Centre, Norton Children’s Hospital, Ochsner Clinic Foundation Hospital, Osaka University Hospital, Osaka Women’s and Children’s Hospital, Ospedale Pediatrico Bambino Gesù, Palmetto Health Richland, Phoenix Children’s Hospital, Polish Mother’s Memorial Hospital Research Institute, Primary Children’s Hospital, Radboud University Nijmegen Medical Centre, Rady Children’s Hospital, Research Institute at Nationwide Children’s Hospital, Royal Children’s Hospital, Royal Hospital for Sick Children, Seattle Children’s Hospital, Shands Children’s Hospital/University of Florida, Shizuoka Children’s Hospital, Sophia Children’s Hospital, St. Francis Children’s Hospital, St. Louis Children’s Hospital, St. Louis University School of Medicine Cardinal Glennon Children’s Hospital, Stollery Children’s Hospital, Sydney Children’s Hospital, The Children’s Hospital at OU Medical Center, The Children’s Hospital of Pittsburgh of UPMC, The Queen Silvia Children’s Hospital SU/Östra, Tsukuba University Hospital, Tufts Medical Center, UNC School of Medicine, University Children’s Hospital Upssala, University Malaya Medical Centre, University of Michigan C.S. Mott Children’s Hospital, University of Padua, University of Texas Medical Branch at Galveston, University of Virginia Medical School, Vanderbilt Children’s Hospital, Vladivostok State Medical University, Winnie Palmer Hospital for Women & Babies, Wolfson Children’s Hospital, and Yale New Haven Children’s Hospital.
Funding
No study funding to declare/disclose.
Author information
Authors and Affiliations
Consortia
Contributions
Study conception/design: ABR, AHE, RAS. Acquisition of data: ABR, CLF, AHE. Analysis/interpretation: ABR, RAS, Drafting of manuscript: ABR, Critical revision: SER-T, DY, EOJ, RAS.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial disclosures or conflicts of interest related to this work. The study does discuss off-label use of medication for alternate indications.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Meeting Presentation: Presented at the 2021 Annual Meeting of the American Pediatric Surgical Association, Virtual Conference. Critical Care Committee APSAsode.
Rights and permissions
About this article
Cite this article
Ramaraj, A.B., Rice-Townsend, S.E., Foster, C.L. et al. Trends in use of prostacyclin analogs for management of CDH-associated pulmonary hypertension. Pediatr Surg Int 38, 1241–1247 (2022). https://doi.org/10.1007/s00383-022-05176-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05176-1