Abstract
Purpose
The aim of this study was to assess intraoperative, postoperative, and oncologic outcome in patients undergoing laparoscopic distal pancreatectomy (LDP) versus open distal pancreatectomy (ODP) for benign and malignant lesions of the pancreas.
Methods
Data from patients undergoing distal pancreatic resection were extracted from the StuDoQ|Pancreas registry of the German Society for General and Visceral Surgery. After propensity score case matching, groups of LDP and ODP were compared regarding demography, comorbidities, operative details, histopathology, and perioperative outcome.
Results
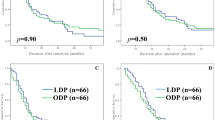
At the time of data extraction, the StuDoQ|Pancreas registry included over 3000 pancreatic resections from over 50 surgical departments in Germany. Data from 353 patients undergoing ODP (n = 254) or LDP (n = 99) from September 2013 to February 2016 at 29 institutions were included in the analysis. Baseline data showed a strong selection bias in LDP patients, which disappeared after 1:1 propensity score matching. A comparison of the matched groups disclosed a significantly longer operation time, higher rate of spleen preservation, more grade A pancreatic fistula, shorter hospital stay, and increased readmissions for LDP. In the small group of patients operated for pancreatic cancer, a lower lymph node yield with a lower lymph node ratio was apparent in LDP.
Conclusions
LDP needed more time but potential advantages include increased spleen preservation and shorter hospital stay, as well as a trend for less transfusion, ventilation, and mortality. LDP for pancreatic cancer was performed rarely and will need critical evaluation in the future. Data from a prospective randomized registry trial is needed to confirm these results.
Similar content being viewed by others
References
Cuschieri A, Jakimowicz JJ, van Spreeuwel J (1996) Laparoscopic distal 70% pancreatectomy and splenectomy for chronic pancreatitis. Ann Surg 223:280
Kooby DA, Hawkins WG, Schmidt CM et al (2010) A multicenter analysis of distal pancreatectomy for adenocarcinoma: is laparoscopic resection appropriate? J Am Coll Surg 210:779–785
de Rooij T, Jilesen AP, Boerma D et al (2015) A Nationwide comparison of laparoscopic and open distal pancreatectomy for benign and malignant disease. J Am Coll Surg 220:263–270
Mehrabi A, Hafezi M, Arvin J et al (2015) A systematic review and meta-analysis of laparoscopic versus open distal pancreatectomy for benign and malignant lesions of the pancreas: It’s time to randomize. Surgery 157:45–55
Venkat R, Edil BH, Schulick RD et al (2012) Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg 255:1048–1059. doi:10.1097/SLA.0b013e318251ee09
Pericleous S, Middleton N, McKay SC et al (2012) Systematic review and meta-analysis of case-matched studies comparing open and laparoscopic distal pancreatectomy: is it a safe procedure? Pancreas 41:993–1000
Shin SH, Kim SC, Song KB et al (2015) A comparative study of laparoscopic vs open distal pancreatectomy for left-sided ductal adenocarcinoma: a propensity score-matched analysis. J Am Coll Surg 220:177–185
Finan KR, Cannon EE, Kim EJ et al (2009) Laparoscopic and open distal pancreatectomy: a comparison of outcomes. Am Surg 75:671–680
Nakamura M, Nakashima H (2013) Laparoscopic distal pancreatectomy and pancreatoduodenectomy: is it worthwhile? A meta-analysis of laparoscopic pancreatectomy. J Hepato-Biliary-Pancreat Sci 20:421–428
Liang S, Hameed U, Jayaraman S (2014) Laparoscopic pancreatectomy: indications and outcomes. World J Gastroenterol WJG 20:14246
Nakamura M, Wakabayashi G, Miyasaka Y, et al. (2015) Multicenter comparative study of laparoscopic and open distal pancreatectomy using propensity score-matching. J Hepato-Biliary-Pancreat Sci
Kooby DA, Gillespie T, Bentrem D et al (2008) Left-sided pancreatectomy: a multicenter comparison of laparoscopic and open approaches. Ann Surg 248:438–446
Ricci C, Casadei R, Taffurelli G et al (2015) Laparoscopic versus open distal pancreatectomy for ductal adenocarcinoma: a systematic review and meta-analysis. J Gastrointest Surg Off J Soc Surg Aliment Tract 19:770–781. doi:10.1007/s11605-014-2721-z
Haukoos JS, Lewis RJ (2015) The propensity score. JAMA 314:1637–1638. doi:10.1001/jama.2015.13480
Bassi C, Dervenis C, Butturini G et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Wente MN, Veit JA, Bassi C et al (2007) Postpancreatectomy hemorrhage (PPH)—an international study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142:20–25. doi:10.1016/j.surg.2007.02.001
Wente MN, Bassi C, Dervenis C et al (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142:761–768
Mangram AJ, Horan TC, Pearson ML, et al. (1999) Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) hospital infection control practices advisory committee Am J Infect Control 27:97–132; quiz 133–134; discussion 96.
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196. doi:10.1097/SLA.0b013e3181b13ca2
Ho D, Imai K, King G, Stuart E (2007) Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Polit Anal 15:199–236
Postlewait LM, Kooby DA (2015) Laparoscopic distal pancreatectomy for adenocarcinoma: safe and reasonable? J Gastrointest Oncol 6:406
Bausch D, Keck T (2013) Laparoscopic pancreatic resections. Langenbeck's Arch Surg 398:939–945
Yan J, Kuang T, Ji D, et al. (2015) Laparoscopic versus open distal pancreatectomy for benign or premalignant pancreatic neoplasms: a two-center comparative study. J Zhejiang Univ Sci B 1
Adam MA, Choudhury K, Goffredo P, et al. (2015) Minimally invasive distal Pancreatectomy for cancer: short-term oncologic outcomes in 1733 patients. World J Surg 1–9
Sharpe SM, Talamonti MS, Wang E et al (2015) The laparoscopic approach to distal pancreatectomy for ductal adenocarcinoma results in shorter lengths of stay without compromising oncologic outcomes. Am J Surg 209:557–563
Hilal MA, Jain G, Kasasbeh F et al (2009) Laparoscopic distal pancreatectomy: critical analysis of preliminary experience from a tertiary referral Centre. Surg Endosc 23:2743–2747
DiNorcia J, Schrope BA, Lee MK et al (2010) Laparoscopic distal pancreatectomy offers shorter hospital stays with fewer complications. J Gastrointest Surg 14:1804–1812
Zhou ZQ, Kim SC, Song KB et al (2014) Laparoscopic spleen-preserving distal pancreatectomy: comparative study of spleen preservation with splenic vessel resection and splenic vessel preservation. World J Surg 38:2973–2979
Malleo G, Salvia R, Mascetta G et al (2014) Assessment of a complication risk score and study of complication profile in laparoscopic distal pancreatectomy. J Gastrointest Surg 18:2009–2015
Weber SM, Cho CS, Merchant N et al (2009) Laparoscopic left pancreatectomy: complication risk score correlates with morbidity and risk for pancreatic fistula. Ann Surg Oncol 16:2825–2833
Ricci C, Casadei R, Taffurelli G et al (2015) Laparoscopic distal pancreatectomy in benign or premalignant pancreatic lesions: is it really more cost-effective than open approach? J Gastrointest Surg:1–10
Rutz DR, Squires MH, Maithel SK et al (2014) Cost comparison analysis of open versus laparoscopic distal pancreatectomy. HPB 16:907–914
Baker MS, Bentrem DJ, Ujiki MB, et al. (2011) Adding days spent in readmission to the initial postoperative length of stay limits the perceived benefit of laparoscopic distal pancreatectomy when compared with open distal pancreatectomy. Am J Surg 201:295–299-300. doi:10.1016/j.amjsurg.2010.09.014
Rehman S, John S, Lochan R et al (2014) Oncological feasibility of laparoscopic distal pancreatectomy for adenocarcinoma: a single-institution comparative study. World J Surg 38:476–483
Jayaraman S, Gonen M, Brennan MF et al (2010) Laparoscopic distal pancreatectomy: evolution of a technique at a single institution. J Am Coll Surg 211:503–509
Acknowledgements
This study has been conducted using the StuDoQ|Pancreas registry provided by the Study, Documentation, and Quality Center (Studien, Dokumentations- und Qualitätszentrum, StuDoQ) of the German Society for General and Visceral Surgery (Deutsche Gesellschaft für Allgemein- und Viszeralchirurgie, DGAV) with the ID StuDoQ|Pankreas-0001.
Members of the StuDoQ|Pancreas study group who contributed to this study, in order of enrolled cases:
Prof. Dr. Thomas Kraus, Allgemeine, Viszeral und Minimalinvasive Chirurgie, Nordwestkrankenhaus Frankfurt, Frankfurt, Germany
Prof. Dr. Michael Ghadimi, Klinik für Allgemein-, Viszeral- und Kinderchirurgie, Universitätsmedizin Göttingen, Göttingen, Germany
Prof. Dr. Carsten Gutt, Allgemein-, Visceral-, Gefäß- und Thoraxchirurgie, Klinikum Memmingen, Memmingen, Germany
Prof. Dr. Thomas Manger, Abteilung für Allgemeine-, Viszeral- und Kinderchirurgie, SRH Waldklinikum Gera, Gera, Germany
Prof. Dr. Jens Werner, Klinik für Allgemeine, Viszeral-, Transplantations-, Gefäß- und Thoraxchirurgie, Klinikum der LMU München, Klinikum Großhadern, München, Germany
Prof. Dr. Helmut Witzigmann, Allgemein- und Viszeralchirurgie, Städtisches Klinikum Dresden Friedrichstadt, Dresden, Germany
Prof. Dr. Christoph-Thomas Germer, Klinik & Poliklinik für Allgemein-, Viszeral-, Gefäß- und Kinderchirurgie, Universitätsklinik Würzburg, Würzburg, Germany
Prof. Dr. Jörg-Peter Ritz, Klinik für Allgemein- und Viszeralchirurgie, Helios Kliniken Schwerin, Schwerin, Germany
Dr. Ute Tröbs, Allgemein- und Viszeralchirurgie, Kreiskrankenhaus Delitzsch, Delitzsch, Germany
Prof. Dr. Winfried Padberg, Allgemein-, Viszeral-, Thorax-, Transplantations- und Kinderchirurgie, Universitätsklinikum Gießen Marburg Standort Gießen, Giessen, Germany
Prof. Dr. Matthias Glanemann, Klinik für Allgemein-, Viszeral-, Gefäß- und Kinderchirurgie, Universitätsklinikum des Saarlandes, Homburg an der Saar, Germany
Prof. Dr. Jörg C. Kalff, Abteilung für Viszerale/kolorektale Chirurgie und Proktologie, Universitätsklinikum Bonn, Bonn, Germany
Prof. Dr. Anton J. Kroesen, Klinik für Allgemein-, Viszeral- und Unfallchirurgie, Krankenhaus Porz am Rhein, Köln, Germany
Prof. Dr. Pompiliu Piso, Chirurgie I, Barmherzige Brüder Regensburg, Regensburg, Germany
Prof. Dr. Stefan Post, Chirurgische Klinik, Universitätsmedizin Mannheim, Mannheim, Germany
Prof. Dr. Hans-Bernd Reith, Allgemein- und Viszeralchirurgie, Agaplesion Diakoniekliniken Kassel, Kassel, Germany
Prof. Dr. Norbert Senninger, Klinik und Poliklinik für Allgemein- und Viszeralchirurgie, Universitätsklinikum Münster, Münster, Germany
Prof. Dr. Ernst Klar, Allgemeine-, Thorax-, Gefäß- und Transplantationschirurgie, Universitätsmedizin Rostock, Rostock, Germany
Dr. Franz-Josef Schumacher, Klinik für Allgemein- und Viszeralchirurgie, Katholische Kliniken Oberhausen, Oberhausen, Germany
Prof. Dr. Albrecht Stier, Klinik für Allgemein- und Viszeralchirurgie, Helios-Klinik Erfurt, Erfurt, Germany
Prof. Dr. Elke Wagler, Allgemein-, Visceral- und Onkochirurgie, Pleißental-Klinik GmbH, Werdau, Germany
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors are members of the German Society for General and Visceral Surgery (DGAV).
Ethical approval
For this type of study, a formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wellner, U.F., Lapshyn, H., Bartsch, D.K. et al. Laparoscopic versus open distal pancreatectomy—a propensity score-matched analysis from the German StuDoQ|Pancreas registry. Int J Colorectal Dis 32, 273–280 (2017). https://doi.org/10.1007/s00384-016-2693-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-016-2693-4