Abstract
Purpose
The purpose of this study is to provide a web-based calculator predicting complication probabilities of patients undergoing colorectal cancer (CRC) surgery in Germany.
Methods
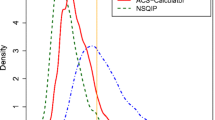
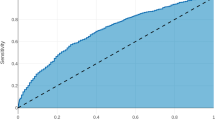
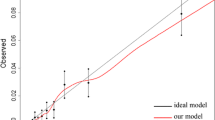
Analyses were based on records of first-time CRC surgery between 2010 and February 2017, documented in the database of the Study, Documentation, and Quality Center (StuDoQ) of the Deutsche Gesellschaft für Allgemein- und Viszeralchirurgie (DGAV), a registry of CRC surgery in hospitals throughout Germany, covering demography, medical history, tumor features, comorbidity, behavioral risk factors, surgical procedures, and outcomes. Using logistic ridge regression, separate models were developed in learning samples of 6729 colon and 4381 rectum cancer patients and evaluated in validation samples of sizes 2407 and 1287. Discrimination was assessed using c statistics. Calibration was examined graphically by plotting observed versus predicted complication probabilities and numerically using Brier scores.
Results
We report validation results regarding 15 outcomes such as any major complication, surgical site infection, anastomotic leakage, bladder voiding disturbance after rectal surgery, abdominal wall dehiscence, various internistic complications, 30-day readmission, 30-day reoperation rate, and 30-day mortality. When applied to the validation samples, c statistics ranged between 0.60 for anastomosis leakage and 0.85 for mortality after rectum cancer surgery. Brier scores ranged from 0.003 to 0.127.
Conclusions
While most models showed satisfactory discrimination and calibration, this does not preclude overly optimistic or pessimistic individual predictions. To avoid misinterpretation, one has to understand the basic principles of risk calculation and risk communication. An e-learning tool outlining the appropriate use of the risk calculator is provided.

Similar content being viewed by others
References
Cohen ME, Bilimoria KY, Ko CY, Hall BL (2009) Development of an American College of Surgeons National Surgery Quality Improvement Program: morbidity and mortality risk calculator for colorectal surgery. J Am Coll Surg 208(6):1009–1016. doi:10.1016/j.jamcollsurg.2009.01.043
Lawson EH, Wang X, Cohen ME, Hall BL, Tanzman H, Ko CY (2011) Morbidity and mortality after colorectal procedures: comparison of data from the American College of Surgeons case log system and the ACS NSQIP. J Am Coll Surg 212(6):1077–1085. doi:10.1016/j.jamcollsurg.2011.03.002
Osler M, Iversen LH, Borglykke A, Martensson S, Daugbjerg S, Harling H, Jorgensen T, Frederiksen B (2011) Hospital variation in 30-day mortality after colorectal cancer surgery in Denmark: the contribution of hospital volume and patient characteristics. Ann Surg 253(4):733–738. doi:10.1097/SLA.0b013e318207556f
Schootman M, Lian M, Pruitt SL, Deshpande AD, Hendren S, Mutch M, Jeffe DB, Davidson N (2014) Hospital and geographic variability in thirty-day all-cause mortality following colorectal cancer surgery. Health Serv Res 49(4):1145–1164. doi:10.1111/1475-6773.12171a
Hermanek P, Mansmann U, Staimmer DS, Riedl S, Hermanek P (2000) The German experience: the surgeon as a prognostic factor in colon and rectal cancer surgery. Surg Oncol Clin N Am 9(1):33–49 vi
Hohenberger W, Merkel S, Hermanek P (2013) Volume and outcome in rectal cancer surgery: the importance of quality management. Int J Color Dis 28(2):197–206. doi:10.1007/s00384-012-1596-2
Mansmann U, Rieger A, Strahwald B, Crispin A (2016) Risk calculators-methods, development, implementation, and validation. Int J Color Dis 31(6):1111–1116. doi:10.1007/s00384-016-2589-3
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15(4):361–387. doi:10.1002/(sici)1097-0258(19960229)15:4<361::aid-sim168>3.0.co;2-4
Anazawa T, Paruch JL, Miyata H, Gotoh M, Ko CY, Cohen ME, Hirahara N, Zhou L, Konno H, Wakabayashi G, Sugihara K, Mori M (2015) Comparison of national operative mortality in gastroenterological surgery using Web-based prospective data entry systems. Medicine 94(49):e2194. doi:10.1097/md.0000000000002194
Justice AC, Covinsky KE, Berlin JA (1999) Assessing the generalizability of prognostic information. Ann Intern Med 130(6):515–524
R Core Team (2016) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna https://www.R-project.org/
Hoffmann TC, Del Mar C (2017) Clinicians’ expectations of the benefits and harms of treatments, screening, and tests: a systematic review. JAMA Intern Med 177(3):407–419. doi:10.1001/jamainternmed.2016.8254
Hoffmann TC, Del Mar C (2015) Patients’ expectations of the benefits and harms of treatments, screening, and tests: a systematic review. JAMA Intern Med 175(2):274–286. doi:10.1001/jamainternmed.2014.6016
Stacey D, Legare F, Lewis K, Barry MJ, Bennett CL, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Thomson R, Trevena L (2017) Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 4:Cd001431. doi:10.1002/14651858.CD001431.pub5
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Crispin, A., Klinger, C., Rieger, A. et al. The DGAV risk calculator: development and validation of statistical models for a web-based instrument predicting complications of colorectal cancer surgery. Int J Colorectal Dis 32, 1385–1397 (2017). https://doi.org/10.1007/s00384-017-2869-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-017-2869-6