Abstract
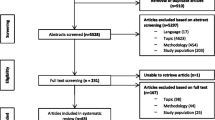
Deficits in quality, a lack of professional process management and, most importantly, neglect of outcome quality are criticized in long-term care. A cluster randomized, controlled trial was conducted to assess whether the Resident Assessment Instrument (RAI) can help to improve or stabilize functional abilities (ADL, IADL) and cognitive skills (MMST), improve quality of life (EQ-5D), and reduce institutionalization, thereby, increasing outcome quality. A total of 69 home care services throughout Germany were included and randomized. The treatment group (n=36) received training in RAI and was supported by the research team during the study (13 months). Comparison of mean differences between the treatment and control groups (n=33) showed no significant effect. Although the multilevel regression results show that clients in the treatment group fared better in terms of ADLs and IADLs (smaller decline) and were less likely to move to nursing homes and be hospitalized, none of these effects is significant. The lack of significance might result from the small number of clients included in the study. Moreover, RAI was not fully implemented and even partial implementation required more time than expected.
Zusammenfassung
In der Pflege werden Qualitätsdefizite, mangelnde Prozesssteuerung und vor allem die Vernachlässigung der Ergebnisqualität bemängelt. In einer clusterrandomisierten kontrollierten Studie wurde untersucht, inwieweit das Resident Assessment Instrument (RAI) eine Verbesserung oder Stabilisierung der funktionalen (ADL, IADL) und kognitiven Fähigkeiten (MMST) der Pflegebedürftigen sowie der Lebensqualität (EQ-5D) bzw. eine Verminderung der Hospitalisierung oder Institutionalisierung bewirken und damit die Ergebnisqualität verbessern kann. Dazu wurden 69 Pflegedienste rekrutiert und randomisiert. Die Interventionsgruppe (n=36) wurde im RAI geschult, über 13 Monate begleitet und unterstützt. Im Vergleich der Mittelwertdifferenzen ergibt sich bei keiner Zielgröße ein signifikanter Unterschied zur Kontrollgruppe (n=33). Zwar zeigen die Klienten der Interventionsgruppe in Multilevel-Regressionen bezüglich der ADL und IADL bessere Entwicklungen (geringere Verschlechterungen), weisen eine geringere Heimeinweisungsquote und weniger Krankenhausaufenthalte auf, allerdings ist keiner dieser Unterschiede signifikant. Die fehlenden Signifikanzen können zum Teil darauf zurückgeführt werden, dass die geplante Stichprobengröße nicht realisiert werden konnte. Zudem gelang die RAI-Umsetzung nicht vollständig bzw. dauerte länger als erwartet.

Similar content being viewed by others
Notes
The ICC shows the variance between the clusters compared to the total variance [26].
Reference
Roth G (2001) Qualitätsmängel der Dienstleistung ambulante Altenpflege. Nationale und internationale Forschungsergebnisse [Quality deficits in geriatric home care. National and international results], Stuttgart
Roth G (2002) Qualität in Pflegeheimen. Expertise im Auftrag des Bundesministeriums für Familie, Senioren, Frauen und Jugend [Quality in nursing homes. Expertise on behalf of the Federal Ministery of Family, Senior Citizens, Women and Youth], Dortmund
Garms-Homolová V, Roth G (2004) Vorkommen, Ursachen und Vermeidung von Pflegemängeln. Forschungsbericht im Auftrag der Enquetekommission “Situation und Zukunft der Pflege in Nordrhein- Westfalen” des Landtag von Nordrhein Westfalen. Forschungsbericht [Appearance, reason and avoidance of deficits in care. Research report on behalf of the committee of enquiry “Situation and future of care in North Rhine-Westphalia” of the state parliament of North Rhine-Westphalia], Berlin, Göttingen
Donabedian A (1966) Evaluation the quality of medical care. Milbank Mem Fund Q 44:166–203
Kane RL (1998) Assuring quality in nursing home care. J Am Geriatr Soc 46:232–237
Görres S, Reif K, Biedermann H et al (2008) Optimierung des Pflegeprozesses durch neue Steuerungsinstrumente. Der Pflegeforschungsverbund Nord [Optimizing the nursing process by new management instruments. The Northern Germany Nursing Research Network]. Z Gerontol Geriatr 39:159–164
Morris JN, Hawes C, Fries BE et al (1990) Designing the national Resident Assessment Instrument for nursing homes. Gerontologist 30:293–307
Hawes C, Morris JN, Phillips CD et al (1997) Development of the nursing home Resident Assessment Instrument in the USA. Age Ageing 26:19–25
Hawes C, Mor V, Phillips CD et al (1997) The OBRA-87 nursing home regulations and implementation of the Resident Assessment Instrument: effect on process quality. J Am Geriatr Soc 45:977–985
Hirdes J, Fries BE, Morris JN et al (2004) Home Care Quality Indicators (HCQIs) based on the MDS-HC. Gerontologist 44:665–679
Achterberg WP, Campen C van, Margriet A et al (1999) Effects of the Resident Assessment Instrument on the care process and health outcomes in nursing homes. A review of the literature. Scand J Rehabil Med 31:131–137
Morris JN, Fries BE, Steel K et al (1997) Comprehensive clinical assessment in community setting: applicability of the MDS-HC. J Am Geriatr Soc 45:1017–1024
Morris SA, Carpenter GI, Berg K, Jones R (2000) Outcome measures for use with home care clients. Can J Aging 19:87–105
Landi F, Onder G, Russo A et al (2001) A new model of integrated home care for the elderly: impact on hospital use. J Clin Epidemiol 54:968–970
Landi F, Onder G, Tua E et al (2001) Impact of a new assessment system, the MDS-HC, on function and hospitalization of homebound older people: a controlled clinical trial. J Am Geriatr Soc 49:1288–1293
Landi F, Cesari M, Onder G et al (2004) Physical activity and mortality in frail, community-living eldery patients. J Gerontol A Biol Sci Med Sci 59A:833–837
June KJ, Lee JY, Yoon JL (2009) Effects of case mangement using Resident Assessment Instrument – Home Care in home health services for older people. J Korean Acad Nurs 39:366–375
Phillips CD, Morris JN, Hawes C et al (1997) Association of the Resident Assessment Instrument (RAI) with changes in function, cognition, and psychosocial status. J Am Geriatr Soc 45:986–993
Holtkamp CCM, Kerkstra A, Ooms ME et al (2001) Effects of the implementation of the Resident Assessment Instrument on gaps between perceived needs and nursing care supply for nursing home residents in the Netherlands. Int J Nurs Stud 38:619–628
Chi I, Law B, Leung AC et al (2010) Residential Assessment Instrument 2.0 in care planning for residents in nursing homes. Hong Kong Med J 16:29–33
Mor V, Intrator O, Fries BE et al (1997) Changes in hospitalization associated with introducing the Resident Assessment Instrument. J Am Geriatr Soc 45:1002–1010
Dellefield ME (2006) Interdisciplinary care planning and the written care plan in nursing homes: a critical review. Gerontologist 46:128–133
Feuerstein I, Kendlbacher E, Fritz E (2008) Evaluierung der Praktikabilität des RAI-HC 2.0 in der Steiermark [Evaluation of the feasibility of RAI-HC 2.0 in Styria]. Pro Care:11–16
Kuß O, Jahn P, Renz P, Landenberger M (2009) Cluster-randomisierte Studien in der Pflegewissenschaft [Cluster randomized trials in nursing research]. Hallesche Beiträge zu den Gesundheits- und Pflegewissenschaften 8:1–12
Cosby RH, Howard M, Kaczorowski J et al (2002) Randomizing patients by family practice: sample size estimation, intracluster correlation and data analysis. Fam Pract 20:77–82
Hastert B (2008) Cluster-randomisierte Studien. Methodische Besonderheiten [Cluster randomized trials. methodically characteristics]. Universität Bremen, Bremen
Nübling M (2005) Methoden zur Erfassung psychischer Belastungen: Erprobung eines Messinstrumentes (COPSOQ) [Measuring psychological stress and strain at work: evaluation of the COPSOQ Questionnaire in Germany]. Wirtschaftsverl. NW Verl. Für Neue Wiss, Bremerhaven
Morris JN, Fries BE, Morris SA (1999) Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci 54A:M546–M553
Carpenter GI, Hastie Cl, Morris JN et al (2006) Measuring change in Activities of Daily Living in nursing home residents with moderate to severe cognitive impairment. BMC Geriatr 6:7
Folstein MF, Folstein S, McHugh PR (1975) Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Rabin R, Charro F de (2001) EQ-5D: a measure of health status from the EuroQol Group. Ann Med 33:337–343
Greiner W, Claes C, Busschbach JJ et al (2005) Validating the EQ-5D with time trade off for the German population. Eur J Health Econ 6:124–130
Noll H (2000) Konzepte der Wohlfahrtsentwicklung: Lebensqualität und “neue” Wohlfahrtskonzepte [Concepts of the development of social services: quality of life and “new” concepts of social services]. WZB-Discussions papers P00-505. Querschnittsgruppe Arbeit und Ökologie, Berlin
Chi-tat Leung A, Pun Liu C, Lee Tsui L et al (2001) The use of the Minimum Data Set. Home care in a case management project in Hong Kong. Care Manag J 3:8–13
Dellefield ME (2007) Implementation of the Resident Assessment Instrument/Minimum Data Set in the nursing home as organization: implications for quality improvement in RN clinical assessment. Geriatr Nurs 28:377–386
Acknowledgment
We would like to thank all participating home care service providers and people in need for care. The study was financed by the German Ministry of Education and Research (BMBF).
Conflict of interest
The corresponding author states that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stolle, C., Wolter, A., Roth, G. et al. Effects of the Resident Assessment Instrument in home care settings. Z Gerontol Geriat 45, 315–322 (2012). https://doi.org/10.1007/s00391-011-0221-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00391-011-0221-2