Abstract
Background
Hip fractures are regarded as a worldwide epidemic and a major public health concern. Changing risk factors, local differences and temporal trends contribute to the particular epidemiology of hip fractures. This overview gives a comprehensive insight into the epidemiology of hip fractures and reviews where German data have contributed to the literature.
Methods
The review of the epidemiology of hip fractures in Germany is based on a systematic literature search in PubMed. Information about the global epidemiology of hip fractures was provided by a selective literature review focusing on specific aspects of the epidemiology of hip fractures.
Results
Hip fracture rates vary more than 100-fold between different countries. In most high-income countries, a rise in age-standardized hip fracture rates was observed until the 1980s and 1990s and a decrease thereafter. Such a decrease has not been observed for Germany so far. Many factors, diseases and drugs have been found to be associated with hip fractures and there is some evidence that fracture risk in later life is already programmed during fetal life and early childhood. Of the hip fracture burden 50% occur in people with disability and in need of care. In nursing homes approximately 4 fractures can be expected in 100 women per year. In people with intellectual or developmental disabilities comparable risks of hip fracture occur 10–40 years earlier than in the general population. Incidence of disability, institutionalization and death are frequent consequences of hip fractures.
Conclusion
The epidemiology of hip fractures is characterized by a high burden of disease, local differences, temporal trends, well-defined high-risk populations and many established risk factors.
Zusammenfassung
Hintergrund
Hüftfrakturen werden weltweit als eines der großen Gesundheitsprobleme angesehen. Diese Übersicht vermittelt einen umfassenden Einblick in die Hüftfrakturepidemiologie und zeigt, wo deutsche Daten neue Erkenntnisse hinzugefügt haben.
Methode
Das Review zur deutschen Hüftfrakturepidemiologie basiert auf einer systematischen Literatursuche in PubMed. Informationen zu spezifischen Teilaspekten der globalen Hüftfrakturepidemiologie beruhen auf einer selektiven Literatursuche.
Ergebnisse
Hüftfrakturraten unterscheiden sich um mehr als das 100-fache zwischen verschiedenen Ländern. In den meisten westlichen Industriestaaten wurde ein Anstieg der altersstandardisierten Raten bis in die 80er- und 90er-Jahre und ein Rückgang in den Folgejahren beobachtet. In Deutschland wurde bisher kein Rückgang der Hüftfrakturrate beobachtet. Hüftfrakturen treten in 50 % der Fälle bei Personen mit Pflegebedürftigkeit auf. In Pflegeheimen muss jährlich mit 4 Hüftfrakturen pro 100 Bewohnern gerechnet werden. Bei Personen mit geistiger Behinderung treten Hüftfrakturen 10 bis 40 Jahre früher auf als in der Allgemeinbevölkerung. Pflegebedürftigkeit, Institutionalisierung und Tod sind häufige Folgen von Hüftfrakturen.
Schlussfolgerung
Die Hüftfrakturepidemiologie ist durch eine hohe Krankheitslast, geographische Unterschiede, zeitliche Veränderungen, Hochrisikopopulationen und eine Reihe etablierter Risikofaktoren charakterisiert.
Similar content being viewed by others
Introduction
The life expectancy of the world population is increasing and more and more people are reaching high ages. This results in a shift of the health burden towards diseases appearing predominantly in higher ages. Hip fractures occur in old and very old people and the absolute number of fractures is therefore strongly affected by the observed demographic change. In the meantime, hip fractures are regarded as a worldwide epidemic and a major public health concern in many countries [1]. Globally, during the year 2000, there were an estimated 1.6 million hip fractures [2] accounting for about 20% of all fractures in people aged 50 years and older. Since nearly all people with a hip fracture are hospitalized for surgical treatment, most of the fractures are captured by routine data. This is an excellent basis for epidemiological analyses and resulted in a large body of literature. There are considerable geographic differences in the incidence of hip fractures which cannot be explained by different age structures of the studied populations. In addition, heterogenous secular trends in the incidence of hip fractures have been observed during the last decades. These local differences and temporal trends contribute to the particular epidemiology of hip fractures.
This overview gives a comprehensive insight in the complete spectrum of global hip fracture epidemiology. Furthermore, the overview points out which epidemiological data from Germany are available, how they differ from other studies and in which fields they add new aspects to the literature of hip fracture epidemiology.
Methods
For the review of hip fracture epidemiology derived from German data a systematic literature search in PubMed was performed (for search strategy see Electronic supplementary material). The literature search identified 145 manuscripts and 8 further manuscripts were found by manually searching the reference lists. After evaluation of title, abstract or full text, 131 publications did not meet the inclusion and exclusion criteria. Despite one inclusion criterion, which was a publication date in 2000 or later, we added 5 articles published before 2000 due to their relevance. The German studies are presented in Supplementary Table 1.
To provide an overview of the international hip fracture epidemiology, an additional selective literature review was performed to identify publications with specific aspects of hip fracture epidemiology.
Results
Age and sex
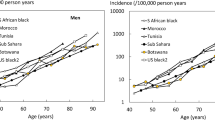
The incidence of hip fractures increases exponentially with age. A decrease in bone mass and an increase in falls result in the strong association between age and the risk of hip fractures [3]. In Western countries approximately three out of four hip fractures occur in women. This huge difference in the absolute number of fractures is partly explained by the higher life expectancy of women. The age-standardized difference between women and men is lower with a relation of about 2:1 in most countries of the world [3, 4]. In Germany, the age-standardized relationship between women and men is somewhat lower (1.72:1) and even nearly identical if residents of German nursing homes are compared (ratio 1.26:1; data derived from Rapp et al.; [5]). Male residents have clearly higher fall rates than female residents [6], which may contribute to their similar risk of hip fractures in long-term care.
Geographic differences
Hip fracture rates differ considerably between different countries and regions of the world. The rates vary more than 200-fold in women and more than 140-fold in men [7]. The countries with the highest incidence are northern Europe (Norway, Sweden, Iceland, Ireland) followed by Central Europe (Denmark, Belgium, Germany, Switzerland, Austria) and eastern Europe (Czech Republic, Slovakia, Hungary) and the Middle East (Oman, Iran). Other high-risk countries are Argentina and Taiwan [8]. The reasons for the huge geographic differences in hip fracture incidence are not well understood. Secular trends in hip fracture incidence which are described below in more detail and migration studies suggest environmental rather than genetic reasons [8]. Various country indicators, such as socioeconomic status, development and urbanization are positively correlated with hip fracture risk [7]; however, there is no clear evidence about an association between socioeconomic factors and fracture risk within countries [9]. Urban areas have 20–60% higher incidences of hip fractures than rural areas [10]. Hard surfaces due to soil sealing, lower physical activity and lower serum levels of vitamin D due to less sun exposure may contribute to the higher risks in urban areas and in countries with higher socioeconomic prosperity. Germany is a high-risk country for hip fractures with an incidence of approximately 130 fractures/100,000 citizens per year (standardized to the German population; [11]). Considerable differences in hip fracture incidence have been reported for the different federal states [12]. They do not follow an apparent pattern and the underlying reasons remain unclear. In addition, no consistent pattern was observed between area level socioeconomic conditions and hip fracture risk [13].
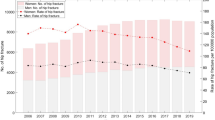
Secular trends
Age-specific hip fracture rates have changed considerably over time in most analyzed countries [14]. The majority of available studies are based on data from Western countries. For most of the regions there was a steep rise in age-standardized rates until the 1980s and 1990s and a decrease thereafter. The trends have been more pronounced in women than in men [15]. For populous regions like South America or many parts of Asia continuously rising hip fracture rates are reported. These trends are highly relevant since they strongly influence the national hip fracture burden. A decrease in age-specific hip fracture rates could counteract the predicted increase due to demographic changes in high income countries [16].
The reasons for the increase and decrease of hip fracture rates within short time periods are speculative. The rapid increase in hip fracture risk is paralleled with the process of urbanization which may act through lower physical activity, more hard surfaces, less sun exposure or other life style factors [14]. An increasing survival of frail people who have low bone quality and a high risk of falls may also contribute to the trend. Factors proposed for the declining trend are the ‘compression of morbidity’ with higher physical activity and lower fall rates, increasing rates of obesity and the introduction of anti-resorptive drugs. The hip fracture risk today may be also influenced by conditions during pregnancy and childhood. Similar to the Barker hypothesis which suggests an association between intrauterine undernourishment and coronary heart disease [17], there is some evidence that fracture risk in later life is already programmed during fetal life and early childhood [18]. Low weight and size at birth and poor childhood growth have been observed to be related to low peak bone mass and high fracture risk later in life [19]. Therefore, a cohort effect may additionally contribute to recent changes of hip fracture risk reflecting changing conditions in nourishment and life style from many years ago.
In the former Eastern Germany an increase in the age-standardized hip fracture rate of 3% per year was observed from 1974 to 1989 [20]. Data for the former Western Germany are not available for this time period. After reunification age-standardized hip fracture rates were approximately 10% and 20% lower in both women and men of the former Eastern Germany, respectively [21]. Between 1995 and 2010 there was no significant trend in the total German population; however, different trends were observed in different subgroups with decreasing rates in women of former Western Germany and increasing rates in men of former Western and Eastern Germany [22]. The converging incidence rates in the former Eastern and Western Germany may be explained by the converging life styles in both parts of Germany [21].
Change of risk over short time periods
The individual fracture risk can change within short time periods. It is well known that hip fracture risk is increased immediately after a preceding fracture [23, 24]. In two German studies it was observed that the initial time period after admission to a nursing home is a high-risk situation for hip and other fragility fractures [25, 26]. The fracture risk was highest during the first weeks after admission and declined thereafter (Fig. 1). Potential causes of the observed pattern may be the new environment which is a challenge to many of the new and often cognitively impaired residents. Another German study found that patients hospitalized due to any reason had an increased risk for hip fractures during the first weeks after discharge from hospital to their homes [27]. A morbidity-related weakness with a deterioration of gait and balance, and a persisting (sub-acute) delirium may be further reasons for a transient increased risk of falls and fractures.
Incidence rate of fractures as a function of time since admission to a nursing home for all fractures combined and femoral fractures. (Data from Rapp et al. [26])
Seasonal patterns
Several studies reported higher incidence rates of hip fractures during winter months [28]. This seasonal pattern was also observed in countries without snow and ice [29]. Low outside temperature, precipitation and wind are associated with increased fracture rates [28].
Risk factors
Many factors, diseases and drugs have been found to be associated with hip fractures. More than 90% of hip fractures are caused by a fall [30] and two thirds of patients with a hip fracture have osteoporosis [31]. Therefore, established risk factors usually work by influencing fall risk and bone quality or both. Age and female sex are strongly associated with fracture risk [3]. The association with a parental history of hip fractures shows that a hereditary component contributes to the hip fracture risk [32]. Further established factors are prior fractures [33], falls, low muscle strength, underweight and smoking [1]. Some diseases are strongly associated with fracture risk. Examples are Cushing’s disease, hyperthyroidism and diabetes mellitus type 1 [34,35,36]. Other diseases have been also found to be associated with fractures, such as depression or epilepsy [37, 38]. Drugs, such as glucocorticoids and aromatase inhibitors may also influence bone mass and bone quality or increase fall risk like benzodiazepines [39], anti-depressants or anti-psychotics [40]. For more comprehensive lists of risk factors we refer to the literature [41].
Three German studies [42,43,44] support earlier findings [45,46,47] of an increased risk of hip fractures in people with Parkinson’s disease, after stroke, or in patients with dementia.
High-risk populations
Fracture risk is particularly high in people with disabilities. German data show that 50% of the hip fracture burden occurs in people with disabilities and need for care living at home or in an institution. In younger age groups (65–80 years) the risk of hip fracture is up to 10 times higher in people with care needs than in people without care needs ([5]; Fig. 2).
Femoral fracture rates in women stratified by setting (community-dwelling people without care needs, community-dwelling people with care needs and residents of nursing homes) and age. (Data from Rapp et al. [5])
Long-term care institutions are the setting with the highest fracture risk. One of the most valid datasets about the incidence of hip fractures occurring in long-term care institutions derives from a German dataset with nearly 70,000 residents [25]. Approximately 4 and 3 hip fractures can be expected in women and men per 100 resident places per year, respectively [5, 25]; however, within this very frail population the degree of disability and fracture risk is inversely associated [25]. Former studies have shown that people with intellectual or developmental disabilities (DD) often have a low bone mass density and an increased fall risk [48]. Some of the discussed reasons are gait problems, seizures, medication or endocrine disorders [48, 49]. Data from Germany demonstrated that comparable risks of hip fracture occur about 10–15 years earlier in females and even 20–40 years earlier in males with DD than in the general population [50].
Consequences of hip fractures
Mortality
Hip fractures occur predominantly in frail older people who have a high baseline mortality risk. Many studies have demonstrated that hip fractures additionally increase the risk of death. Excess mortality is consistently higher in men than in women [51]. It is highest in the days and weeks following the fracture and remains elevated for months [51, 52]. It is estimated that 20–30% of deaths are causally related to the fracture event [53]. In residents of German nursing homes excess mortality during the first 6 months is even higher with 57.8% in men and 32.9% in women [25].
Disability
Hip fractures have a high impact on older people’s abilities, function and quality of life. Only 40–60% of hip fracture patients recover their prefracture level of mobility [54]. Between 20% and 60% of patients who were independent in self-care activities, such as washing and dressing before the fracture require assistance to do these tasks after 1 year [55]. Most patients who recover their prefracture function and walking ability do so within the first 6 months after discharge from hospital [54, 56]. The degree of recovery is even lower in institutionalized patients.
Institutionalization
Hip fractures may compromise an independent life and make it often impossible to live at home any longer. In high income countries, 10–20% of hip fracture patients are institutionalized following a hip fracture [54]. A German study demonstrated institutionalization rates of 15% in women and 11.8% in men within 6 months after hospital discharge [57]. The risk of institutionalization increases from 3.6% in women aged 65–69 years to 34.8% in women aged 95 years and older. In men the risk of institutionalization after hip fracture is even comparable in size with that after stroke (Fig. 3).
Rates of institutionalization within 6 months after discharge from hospital in men with femoral fracture, stroke, myocardial infarction, pneumonia and other reasons for hospitalization in different age categories. (Data from Rapp et al. [57])
Secondary fractures
A prior hip fracture increases the risk of a subsequent fragility fracture by the factor 2– 2.5 [58, 59]. The increase of the relative risk is similar in men and women. The risk for a second hip fracture is particularly pronounced during the first months after the first fracture [60].
Prevention of hip fractures
The etiology of hip fractures is complex and the underlying factors are only partly amenable to prevention. Lifelong moderate to vigorous physical activity seems to reduce the risk of hip fractures by about 40% [61]. Osteoporosis can be treated by specific medication which reduces the risk of hip fractures by about 40% [62]; however, a considerable percentage of people with a new hip fracture do not meet the criteria of treatment prior to the fracture [31]. Single fall prevention studies were not sufficiently powered for the analysis of fracture incidence but a meta-analysis of fall prevention exercise interventions found a reduction of osteoporotic fractures by 61% [63]; however, a model calculation which used German baseline conditions showed that unrealistically high medical treatment rates or fall prevention participation rates are needed to achieve substantial effects on the burden of hip fractures at present and in the future [31]. Therefore, coordinated interventions are needed which address different measures and strategies of fracture prevention on a population level [64].
References
Marks R (2010) Hip fracture epidemiological trends, outcomes, and risk factors, 1970–2009. Int J Gen Med 3:1–17
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359(9319):1761–1767
Kanis JA, Borgström F, Compston J, Dreinhöfer K, Nolte E, Jonsson L et al (2013) SCOPE: a scorecard for osteoporosis in Europe. Arch Osteoporos 8:144
Rapp K, Becker C, Cameron ID, Klenk J, Kleiner A, Bleibler F et al (2012) Femoral fracture rates in people with and without disability. Age Ageing 41(5):653–658
Rapp K, Becker C, Cameron ID, König H‑H, Büchele G (2012) Epidemiology of falls in residential aged care: analysis of more than 70,000 falls from residents of bavarian nursing homes. J Am Med Dir Assoc 13(2):187.e1
Cauley JA, Chalhoub D, Kassem AM, Fuleihan GE-H (2014) Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol 10(6):338–351
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23(9):2239–2256
Brennan SL, Pasco JA, Urquhart DM, Oldenburg B, Hanna F, Wluka AE (2009) The association between socioeconomic status and osteoporotic fracture in population-based adults: a systematic review. Osteoporos Int 20(9):1487–1497
Brennan SL, Pasco JA, Urquhart DM, Oldenburg B, Hanna FS, Wluka AE (2010) The association between urban or rural locality and hip fracture in community-based adults: a systematic review. J Epidemiol Community Health 64(8):656–665
Icks A, Haastert B, Wildner M, Becker C, Meyer G (2008) Trend of hip fracture incidence in Germany 1995–2004: a population-based study. Osteoporos Int 19(8):1139–1145
Defèr A, Schober H‑C, Möhrke W, Abendroth K, Hofbauer LC, Task Group for Treatment Research at German Society of Osteology, Federal Association of German Osteologists (Bundesverband der Osteologen Deutschland e. V.) et al (2014) Are there still east-to-west differences in the incidence of hip fractures in Germany? Arch Osteoporos 9:195
Icks A, Haastert B, Wildner M, Becker C, Rapp K, Dragano N et al (2009) Hip fractures and area level socioeconomic conditions: a population-based study. BMC Public Health 9:114
Ballane G, Cauley JA, Luckey MM, Fuleihan GE-H (2014) Secular trends in hip fractures worldwide: opposing trends East versus West. J Bone Miner Res 29(8):1745–1755
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM et al (2011) Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22(5):1277–1288
Concin H, Brozek W, Benedetto K‑P, Häfele H, Kopf J, Bärenzung T et al (2016) Hip fracture incidence 2003–2013 and projected cases until 2050 in Austria: a population-based study. Int J Public Health 61(9):1021–1030
Barker DJ (1995) Fetal origins of coronary heart disease. BMJ 311(6998):171–174
Cooper C, Westlake S, Harvey N, Javaid K, Dennison E, Hanson M (2006) Review: developmental origins of osteoporotic fracture. Osteoporos Int 17(3):337–347
Cooper C, Eriksson JG, Forsén T, Osmond C, Tuomilehto J, Barker DJ (2001) Maternal height, childhood growth and risk of hip fracture in later life: a longitudinal study. Osteoporos Int 12(8):623–629
Wildner M, Casper W, Bergmann KE (1999) A secular trend in hip fracture incidence in East Germany. Osteoporos Int 9(2):144–150
Wildner M, Clark DE (2001) Hip fracture incidence in east and west germany: reassessement ten years after unification. Osteoporos Int 12(2):136–139
Icks AIA, Arend WAW, Becker CBC, Rapp KRK, Haastert BHB (2013) Incidence of hip fractures in Germany, 1995–2010. Arch Osteoporos 8(1–2):1–7
Johansson H, Siggeirsdóttir K, Harvey NC, Odén A, Gudnason V, McCloskey E et al (2017) Imminent risk of fracture after fracture. Osteoporos Int 28(3):775–780
Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C et al (2004) Fracture risk following an osteoporotic fracture. Osteoporos Int 15(3):175–179
Rapp K, Becker C, Lamb SE, Icks A, Klenk J (2008) Hip fractures in institutionalized elderly people: incidence rates and excess mortality. J Bone Miner Res 23(11):1825–1831
Rapp K, Lamb SE, Klenk J, Kleiner A, Heinrich S, König H‑H et al (2009) Fractures after nursing home admission: incidence and potential consequences. Osteoporos Int 20(10):1775–1783
Rapp K, Cameron ID, Becker C, Kleiner A, Eckardt M, König H‑H et al (2012) Femoral fracture rates after discharge from hospital to the community. J Bone Miner Res. https://doi.org/10.1002/jbmr.1809
Román Ortiz C, Tenías JM, Estarlich M, Ballester F (2015) Systematic review of the association between climate and hip fractures. Int J Biometeorol 59(10):1511–1522
Turner RM, Hayen A, Dunsmuir WTM, Finch CF (2011) Air temperature and the incidence of fall-related hip fracture hospitalisations in older people. Osteoporos Int 22(4):1183–1189
Youm T, Koval KJ, Kummer FJ, Zuckerman JD (1999) Do all hip fractures result from a fall? Am J Orthop (Belle Mead, NJ) 28(3):190–194
Benzinger P, Becker C, Todd C, Bleibler F, Rothenbacher D, König H‑H et al (2016) The impact of preventive measures on the burden of femoral fractures—a modelling approach to estimating the impact of fall prevention exercises and oral bisphosphonate treatment for the years 2014 and 2025. BMC Geriatr 16:75
Kanis JA, Johansson H, Oden A, Johnell O, De Laet C, Eisman JA et al (2004) A family history of fracture and fracture risk: a meta-analysis. Bone 35(5):1029–1037
Bluhmki T, Peter RS, Rapp K, König H‑H, Becker C, Lindlbauer I et al (2017) Understanding mortality of femoral fractures following low-impact trauma in persons with and without care need. J Am Med Dir Assoc 18(3):221–226
Vestergaard P, Lindholm J, Jørgensen JOL, Hagen C, Hoeck HC, Laurberg P et al (2002) Increased risk of osteoporotic fractures in patients with Cushing’s syndrome. Eur J Endocrinol 146(1):51–56
Vestergaard P, Mosekilde L (2003) Hyperthyroidism, bone mineral, and fracture risk—a meta-analysis. Thyroid 13(6):585–593
Shah VN, Shah CS, Snell-Bergeon JK (2015) Type 1 diabetes and risk of fracture: meta-analysis and review of the literature. Diabet Med 32(9):1134–1142
Wu Q, Liu J, Gallegos-Orozco JF, Hentz JG (2010) Depression, fracture risk, and bone loss: a meta-analysis of cohort studies. Osteoporos Int 21(10):1627–1635
Vestergaard P (2005) Epilepsy, osteoporosis and fracture risk—a meta-analysis. Acta Neurol Scand 112(5):277–286
Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM et al (2009) Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 169(21):1952–1960
Lee S‑H, Hsu W‑T, Lai C‑C, Esmaily-Fard A, Tsai Y‑W, Chiu C‑C et al (2017) Use of antipsychotics increases the risk of fracture: a systematic review and meta-analysis. Osteoporos Int 28(4):1167–1178
Pisani P, Renna MD, Conversano F, Casciaro E, Di Paola M, Quarta E et al (2016) Major osteoporotic fragility fractures: risk factor updates and societal impact. World J Orthop 7(3):171–181
Benzinger P, Rapp K, Maetzler W, König H‑H, Jaensch A, Klenk J et al (2014) Risk for femoral fractures in Parkinson’s disease patients with and without severe functional impairment. PLoS ONE 9(5):e97073
Benzinger P, Rapp K, König HH, Bleibler F, Globas C, Beyersmann J et al (2015) Risk of osteoporotic fractures following stroke in older persons. Osteoporos Int 26(4):1341–1349
Bohlken J, Jacob L, Schaum P, Rapp MA, Kostev K (2017) Hip fracture risk in patients with dementia in German primary care practices. Dementia (London) 16(7):853–864
Critchley RJ, Khan SK, Yarnall AJ, Parker MJ, Deehan DJ (2015) Occurrence, management and outcomes of hip fractures in patients with Parkinson’s disease. Br Med Bull 115(1):135–142
Luan L, Li R, Wang Z, Hou X, Gu W, Wang X et al (2016) Stroke increases the risk of hip fracture: a systematic review and meta-analysis. Osteoporos Int 27(11):3149–3154
Zhao Y, Shen L, Ji H‑F (2012) Alzheimer’s disease and risk of hip fracture: a meta-analysis study. ScientificWorldJournal 2012:872173
Srikanth R, Cassidy G, Joiner C, Teeluckdharry S (2011) Osteoporosis in people with intellectual disabilities: a review and a brief study of risk factors for osteoporosis in a community sample of people with intellectual disabilities. J Intellect Disabil Res 55(1):53–62
Hsieh K, Rimmer J, Heller T (2012) Prevalence of falls and risk factors in adults with intellectual disability. Am J Intellect Dev Disabil 117(6):442–454
Büchele G, Becker C, Cameron ID, Auer R, Rothenbacher D, König HH et al (2017) Fracture risk in people with developmental disabilities: results of a large claims data analysis. Osteoporos Int 28(1):369–375
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20(10):1633–1650
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B et al (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152(6):380–390
Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK (2003) The components of excess mortality after hip fracture. Bone 32(5):468–473
Dyer SM, Crotty M, Fairhall N, Magaziner J, Beaupre LA et al (2016) A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr 16:158
Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M et al (2000) Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci 55(9):M498–M507
Bertram M, Norman R, Kemp L, Vos T (2011) Review of the long-term disability associated with hip fractures. Inj Prev 17(6):365–370
Rapp K, Rothenbacher D, Magaziner J, Becker C, Benzinger P, König H‑H et al (2015) Risk of nursing home admission after femoral fracture compared with stroke, myocardial infarction, and pneumonia. J Am Med Dir Assoc 16(8):715.e7–715.e12
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15(4):721–739
Colón-Emeric C, Kuchibhatla M, Pieper C, Hawkes W, Fredman L, Magaziner J et al (2003) The contribution of hip fracture to risk of subsequent fractures: data from two longitudinal studies. Osteoporos Int 14(11):879–883
Ryg J, Rejnmark L, Overgaard S, Brixen K, Vestergaard P (2009) Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977–2001. J Bone Miner Res 24(7):1299–1307
Moayyeri A (2008) The association between physical activity and osteoporotic fractures: a review of the evidence and implications for future research. Ann Epidemiol 18(11):827–835
Nguyen ND, Eisman JA, Nguyen TV (2006) Anti-hip fracture efficacy of biophosphonates: a Bayesian analysis of clinical trials. J Bone Miner Res 21(2):340–349
El-Khoury F, Cassou B, Charles M‑A, Dargent-Molina P (2013) The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ 347:f6234–f6234
McClure R, Turner C, Peel N, Spinks A, Eakin E, Hughes K (2005) Population-based interventions for the prevention of fall-related injuries in older people. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd004441.pub2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K. Rapp, G. Büchele, K. Dreinhöfer, B. Bücking, C. Becker and P. Benzinger declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Informationen zu spezifischen Teilaspekten der globalen Hüftfrakturepidemiologie beruhen auf einer selektiven Literatursuche.
Caption Electronic Supplementary Material
Rights and permissions
Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Rapp, K., Büchele, G., Dreinhöfer, K. et al. Epidemiology of hip fractures. Z Gerontol Geriat 52, 10–16 (2019). https://doi.org/10.1007/s00391-018-1382-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00391-018-1382-z