Abstract
Objective
The aim of this study was to compare the outcome of nonagenarians (≥ 90 years) with that of younger (< 90 years) patients undergoing transcatheter aortic valve implantation (TAVI) in current practice.
Methods
Data are collected from the German Aortic Valve Registry (GARY), which was designed to evaluate current practice in the invasive treatment of patients with aortic valve diseases in Germany. Data were analyzed regarding procedural outcome, 30-day, and 1-year outcomes of nonagenarians in comparison to that of younger patients.
Results
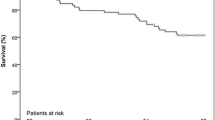
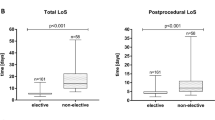
Between 2011 and 2015, 2436/33,051 (7.3%) nonagenarians underwent TAVI and were included in GARY. Nonagenarians were significantly more often male (45.2% vs. 40.0%, p < 0.001), frail (38.7% vs. 34.7%, p < 0.001), and had higher EuroSCORE scores than younger patient group (23.2% vs. 17.0%). Nonagenarians were significantly less often treated via transapical access (16.3% vs. 22.3%, p < 0.001). Procedure was performed significantly less often in general anesthesia (58.2% vs. 60.7%, p = 0.02) in nonagenarians, while necessity of pacemaker implantation was significantly higher in nonagenarians (27.2% vs. 24.8%, p > 0.001). The incidence of other typical postprocedural complications such as severe bleeding events and vascular complications were comparable between groups. However, 30-day (5.2% vs. 3.9%) and 1-year (22.7% vs. 17.7%) mortality rates were significantly higher among nonagenarians and age ≥ 90 years could be identified as an isolated risk factor for mortality.
Conclusion
TAVI is a highly standardized procedure that can be performed safely with high procedural success even in very old patients. Although mortality is significantly higher in these patients—most probably due to the intrinsic higher risk profile of the very old patients—the results are still acceptable. To optimize outcome, especially elderly patients seem to profit from a procedure under local anesthesia or conscious sedation, to minimize the rate of postoperative delirium and the length of stay and to facilitate early mobilization.

Similar content being viewed by others
References
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M (2006) Burden of valvular heart diseases: a population-based study. Lancet 368:1005–1011
Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, Thourani VH, Tuzcu EM, Miller DC, Herrmann HC, Doshi D, Cohen DJ, Pichard AD, Kapadia S, Dewey T, Babaliaros V, Szeto WY, Williams MR, Kereiakes D, Zajarias A, Greason KL, Whisenant BK, Hodson RW, Moses JW, Trento A, Brown DL, Fearon WF, Pibarot P, Hahn RT, Jaber WA, Anderson WN, Alu MC, Webb JG (2016) PARTNER 2 investigators. Transcatheter or surgical aortic-valve replacement in intermediate-risk Patients. N Engl J Med. 374:1609–1620
Gaede L, Blumenstein J, Liebetrau C, Dörr O, Kim W-K, Nef H, Husser O, Elsässer A, Hamm CW, Möllmann H (2018) Outcome after transvascular transcatheter aortic valve implantation in 2016. Eur Heart J. 39:667–675
Möllmann H, Bestehorn K, Bestehorn M, Papoutsis K, Fleck E, Ertl G, Kuck K-H, Hamm C (2016) In-hospital outcome of transcatheter vs. surgical aortic valve replacement in patients with aortic valve stenosis: complete dataset of patients treated in 2013 Germany. Clin Res Cardiol 105:553–559
Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, Kapadia SR, Malaisrie SC, Cohen DJ, Pibarot P, Leipsic J, Hahn RT, Blanke P, Williams MR, McCabe JM, Brown DL, Babaliaros V, Goldman S, Szeto WY, Genereux P, Pershad A, Pocock SJ, Alu MC, Webb JG, Smith CR (2019) PARTNER 3 investigators. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 380:1695–1705
Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O’Hair D, Bajwa T, Heiser JC, Merhi W, Kleiman NS, Askew J, Sorajja P, Rovin J, Chetcuti SJ, Adams DH, Teirstein PS, Zorn GL 3rd, Forrest JK, Tchétché D, Resar J, Walton A, Piazza N, Ramlawi B, Robinson N, Petrossian G, Gleason TG, Oh JK, Boulware MJ, Qiao H, Mugglin AS, Reardon MJ (2019) Evolut low risk trial investigators. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. 380:1706–1715
Arsalan M, Szerlip M, Vemulapalli S, Holper EM, Arnold SV, Li Z, DiMaio MJ, Rumsfeld JS, Brown DL, Mack MJ (2016) Should transcatheter aortic valve replacement be performed in nonagenarians?: insights from the STS/ACC TVT registry. J Am Coll Cardiol. 67:1387–1395
Mack MC, Szerlip M, Herbert M, Akram S, Kim R, Prince B, Harrington KB, Mack M, Holper E (2014) Outcome of treatment of nonagenarians with severe aortic stenosis. J Am Coll Cardiol. 63:A1935
Noble S, Frangos E, Samaras N, Ellenberger C, Frangos C, Cikirikcioglu M, Bendjelid K, Frei A, Myers P, Licker M, Roffi M (2013) Transcatheter aortic valve implantation in nonagenarians: effective and safe. Eur J Intern Med. 24:750–755
Yamamoto M, Meguro K, Mouillet G, Bergoend E, Monin J-L, Lim P, Dubois-Rande J-L, Teiger E (2012) Comparison of effectiveness and safety of transcatheter aortic valve implantation in patients aged ≥90 years versus %3c90 years. Am J Cardiol. 110:1156–1163
Lange R, Beckmann A, Neumann T, Krane M, Deutsch M-A, Landwehr S, Kötting J, Welz A, Zahn R, Cremer J, Figulla HR, Schuler G, Holzhey DM, Funkat A-K, Heusch G, Sack S, Pasic M, Meinertz T, Walther T, Kuck K-H, Beyersdorf F, Böhm M, Möllmann H, Hamm CW, Mohr FW (2016) GARY executive board. Quality of life after transcatheter aortic valve replacement: prospective data from GARY (German Aortic Valve Registry). JACC Cardiovasc Interv. 9:2541–2554
Green P, Woglom AE, Genereux P, Daneault B, Paradis J-M, Schnell S, Hawkey M, Maurer MS, Kirtane AJ, Kodali S, Moses JW, Leon MB, Smith CR, Williams M (2012) The impact of frailty status on survival after transcatheter aortic valve replacement in older adults with severe aortic stenosis: a single-center experience. JACC Cardiovasc Interv. 5:974–981
Stortecky S, Schoenenberger AW, Moser A, Kalesan B, Jüni P, Carrel T, Bischoff S, Schoenenberger C-M, Stuck AE, Windecker S, Wenaweser P (2012) Evaluation of multidimensional geriatric assessment as a predictor of mortality and cardiovascular events after transcatheter aortic valve implantation. JACC Cardiovasc Interv. 5:489–496
Beckmann A, Hamm C, Figulla HR, Cremer J, Kuck KH, Lange R, Zahn R, Sack S, Schuler GC, Walther T, Beyersdorf F, Böhm M, Heusch G, Funkat AK, Meinertz T, Neumann T, Papoutsis K, Schneider S, Welz A, Mohr FW (2012) GARY executive board. The German Aortic Valve Registry (GARY): a nationwide registry for patients undergoing invasive therapy for severe aortic valve stenosis. Thorac Cardiovasc Surg. 60:319–325
Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH, Brott TG, Cohen DJ, Cutlip DE, van Es G-A, Hahn RT, Kirtane AJ, Krucoff MW, Kodali S, Mack MJ, Mehran R, Rodés-Cabau J, Vranckx P, Webb JG, Windecker S, Serruys PW, Leon MB (2012) Valve academic research consortium (VARC)-2. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document (VARC-2). Eur J Cardiothorac Surg. 42:S45–60
Beckmann A, Meyer R, Lewandowski J, Frie M, Markewitz A, Harringer W (2018) German heart surgery report 2017: the annual updated registry of the german society for thoracic and cardiovascular surgery. Thorac Cardiovasc Surg. 66:608–621
Abramowitz Y, Chakravarty T, Jilaihawi H, Kashif M, Zadikany R, Lee C, Matar G, Cheng W, Makkar RR (2015) Comparison of outcomes of transcatheter aortic valve implantation in patients ≥90 years versus %3c90 years. Am J Cardiol. 116:1110–1115
Havakuk O, Finkelstein A, Steinvil A, Halkin A, Arbel Y, Abramowitz Y, Ben Assa E, Konigstein M, Keren G, Banai S (2014) Comparison of outcomes in patients ≤85 versus %3e85 years of age undergoing transcatheter aortic-valve implantation. Am J Cardiol. 113:138–141
Yamamoto M, Mouillet G, Meguro K, Gilard M, Laskar M, Eltchaninoff H, Fajadet J, Iung B, Donzeau-Gouge P, Leprince P, Leuguerrier A, Prat A, Lievre M, Chevreul K, Dubois-Rande J-L, Teiger E (2014) FRANCE-2 registry investigators. Clinical results of transcatheter aortic valve implantation in octogenarians and nonagenarians: insights from the FRANCE-2 registry. Ann Thorac Surg. 97:29–36
Steinvil A, Leshem-Rubinow E, Halkin A, Abramowitz Y, Ben-Assa E, Shacham Y, Bar-Dayan A, Keren G, Banai S, Finkelstein A (2015) Vascular complications after transcatheter aortic valve implantation and their association with mortality reevaluated by the valve academic research consortium definitions. Am J Cardiol. 115:100–106
Barbash IM, Barbanti M, Webb J, Molina-Martin De Nicolas J, Abramowitz Y, Latib A, Nguyen C, Deuschl F, Segev A, Sideris K, Buccheri S, Simonato M, Rosa FD, Tamburino C, Jilaihawi H, Miyazaki T, Himbert D, Schofer N, Guetta V, Bleiziffer S, Tchetche D, Immè S, Makkar RR, Vahanian A, Treede H, Lange R, Colombo A, Dvir D (2015) Comparison of vascular closure devices for access site closure after transfemoral aortic valve implantation. Eur Heart J 36:3370–3379
Thourani VH, Kodali S, Makkar RR, Herrmann HC, Williams M, Babaliaros V, Smalling R, Lim S, Malaisrie SC, Kapadia S, Szeto WY, Greason KL, Kereiakes D, Ailawadi G, Whisenant BK, Devireddy C, Leipsic J, Hahn RT, Pibarot P, Weissman NJ, Jaber WA, Cohen DJ, Suri R, Tuzcu EM, Svensson LG, Webb JG, Moses JW, Mack MJ, Miller DC, Smith CR, Alu MC, Parvataneni R, D’Agostino RB Jr, Leon MB (2016) Transcatheter aortic valve replacement versus surgical valve replacement in intermediate-risk patients: a propensity score analysis. Lancet 387:2218–2225
Gaede L, Kim W-K, Liebetrau C, Dörr O, Sperzel J, Blumenstein J, Berkowitsch A, Walther T, Hamm C, Elsässer A, Nef H, Möllmann H (2018) Pacemaker implantation after TAVI: predictors of AV block persistence. Clin Res Cardiol. 107:60–69
Barbanti M, Gulino S, Costa G, Tamburino C (2017) Pathophysiology, incidence and predictors of conduction disturbances during Transcatheter Aortic Valve Implantation. Expert Rev Med Devices. 14:135–147
Urena M, Webb JG, Tamburino C, Muñoz-García AJ, Cheema A, Dager AE, Serra V, Amat-Santos IJ, Barbanti M, Immè S, Briales JHA, Benitez LM, Al Lawati H, Cucalon AM, García Del Blanco B, López J, Dumont E, Delarochellière R, Ribeiro HB, Nombela-Franco L, Philippon F, Rodés-Cabau J (2014) Permanent pacemaker implantation after transcatheter aortic valve implantation: impact on late clinical outcomes and left ventricular function. Circulation 129:1233–1243
Fujita B, Schmidt T, Bleiziffer S, Bauer T, Beckmann A, Bekeredjian R, Möllmann H, Walther T, Landwehr S, Hamm C, Beyersdorf F, Katus HA, Harringer W, Ensminger S, Frerker C (2019) Impact of new pacemaker implantation following surgical and transcatheter aortic valve replacement on 1-year outcome. Eur J Cardiothorac Surg. 57(1):151–159
Fadahunsi OO, Olowoyeye A, Ukaigwe A, Li Z, Vora AN, Vemulapalli S, Elgin E, Donato A (2016) Incidence, predictors, and outcomes of permanent pacemaker implantation following transcatheter aortic valve replacement: analysis from the US Society of thoracic surgeons/american college of cardiology TVT registry. JACC Cardiovasc Interv. 9:2189–2199
Kapadia SR, Huded CP, Kodali SK, Svensson LG, Tuzcu EM, Baron SJ, Cohen DJ, Miller DC, Thourani VH, Herrmann HC, Mack MJ, Szerlip M, Makkar RR, Webb JG, Smith CR, Rajeswaran J, Blackstone EH, Leon MB (2018) PARTNER trial investigators. Stroke after surgical versus transfemoral transcatheter aortic valve replacement in the PARTNER trial. J Am Coll Cardiol. 72:2415–2426
Soundhar A, Udesh R, Mehta A, Schindler J, Jeevanantham V, Gleason T, Thirumala PD (2017) Delirium following transcatheter aortic valve replacement: national inpatient sample analysis. J Cardiothorac Vasc Anesth. 31:1977–1984
Husser O, Fujita B, Hengstenberg C, Frerker C, Beckmann A, Möllmann H, Walther T, Bekeredjian R, Böhm M, Pellegrini C, Bleiziffer S, Lange R, Mohr F, Hamm C, Bauer T, Ensminger S (2018) Conscious sedation versus general anesthesia in transcatheter aortic valve replacement: the German Aortic Valve Registry. JACC Cardiovasc Interv. 11:567–578
Ehret C, Rossaint R, Foldenauer AC, Stoppe C, Stevanovic A, Dohms K, Hein M, Schälte G (2017) Is local anaesthesia a favourable approach for transcatheter aortic valve implantation? A systematic review and meta-analysis comparing local and general anaesthesia. BMJ Open. 7:e016321
Dehédin B, Guinot PG, Ibrahim H, Allou N (2011) Anesthesia and perioperative management of patients who undergo transfemoral transcatheter aortic valve implantation: an observational study of general versus local/regional anesthesia in 125 consecutive patients. J Cardiothorac Vasc Anesth. 25:1036–1043
Maas EHA, Pieters BMA, Van de Velde M, Rex S (2016) General or local anesthesia for TAVI? A systematic review of the literature and meta-analysis. CPD. 22:1868–1878
Pressler A, Förschner L, Hummel J, Haller B, Christle JW, Halle M (2018) Long-term effect of exercise training in patients after transcatheter aortic valve implantation: Follow-up of the SPORT:TAVI randomised pilot study. Eur J Prev Cardiol. 25:794–801
Pressler A, Christle JW, Lechner B, Grabs V, Haller B, Hettich I, Jochheim D, Mehilli J, Lange R, Bleiziffer S, Halle M (2016) Exercise training improves exercise capacity and quality of life after transcatheter aortic valve implantation: A randomized pilot trial. Am Heart J. 182:44–53
Pulignano G, Gulizia MM, Baldasseroni S, Bedogni F, Cioffi G, Indolfi C, Romeo F, Murrone A, Musumeci F, Parolari A, Patanè L, Pino PG, Mongiardo A, Spaccarotella C, Di Bartolomeo R, Musumeci G (2017) ANMCO/SIC/SICI-GISE/SICCH executive summary of consensus document on risk stratification in elderly patients with aortic stenosis before surgery or transcatheter aortic valve replacement. Eur Heart J Suppl. 19:D354–D369
Funding
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Blumenstein, J., Möllmann, H., Bleiziffer, S. et al. Transcatheter aortic valve implantation in nonagenarians: insights from the German Aortic Valve Registry (GARY). Clin Res Cardiol 109, 1099–1106 (2020). https://doi.org/10.1007/s00392-020-01601-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-020-01601-4