Abstract
Introduction
The high rigidity of metal implants may be a cause of failure after fixation of proximal humerus fractures. Carbon fiber-reinforced polyetheretherketone (PEEK) plates with a modulus similar to human cortical bone may help to overcome this problem. The present study assesses the biomechanical behavior of a PEEK plate compared with a titanium locking plate.
Materials and methods
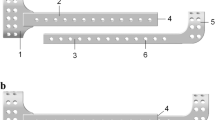
Unstable two- and three-part fractures were simulated in 12 pairs of cadaveric humeri and were fixed with either a PEEK or a titanium locking plate using a pairwise comparison. With an optical motion capture system, the stiffness, failure load, plate bending, and the relative motion at the bone–implant interface and at the fracture site were evaluated.
Results
The mean load to failure for two- and three-part fracture fixations was, respectively, 191 N (range 102–356 N) and 142 N (range 102–169 N) in the PEEK plate group compared with 286 N (range 191–395 N) and 258 N (range 155–366 N) in the titanium locking plate group. The PEEK plate showed significantly more bending in both the two- and three-part fractures (p < 0.05), an increased relative motion at the bone–implant interface and lower stiffness values (p < 0.05).
Conclusion
In this biomechanical study on unstable proximal humerus fractures, fixation with a PEEK plate showed lower fixation strength and increased motion at the bone–implant interface compared with a titanium locking plate.








Similar content being viewed by others
References
Bell JE, Leung BC, Spratt KF, Koval KJ, Weinstein JD, Goodman DC, Tosteson AN (2011) Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Jt Surg Am 93(2):121–131. doi:10.2106/JBJS.I.01505
Warriner AH, Patkar NM, Curtis JR, Delzell E, Gary L, Kilgore M, Saag K (2011) Which fractures are most attributable to osteoporosis? J Clin Epidemiol 64(1):46–53. doi:10.1016/j.jclinepi.2010.07.007
Palvanen M, Kannus P, Niemi S, Parkkari J (2006) Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res 442:87–92
Gupta AK, Harris JD, Erickson BJ, Abrams GD, Bruce B, McCormick F, Nicholson GP, Romeo AA (2014) Surgical management of complex proximal humerus fractures—a systematic review of 92 studies including 4500 patients. J Orthop Trauma. doi:10.1097/BOT.0000000000000229
Schliemann B, Siemoneit J, Theisen C, Kösters C, Weimann A, Raschke MJ (2012) Complex fractures of the proximal humerus in the elderly—outcome and complications after locking plate fixation. Musculoskelet Surg 96(Suppl 1):S3–S11. doi:10.1007/s12306-012-0181-8
Sproul RC, Iyengar JJ, Devcic Z, Feeley BT (2011) A systematic review of locking plate fixation of proximal humerus fractures. Injury 42(4):408–413. doi:10.1016/j.injury.2010.11.058
Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P (2009) Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elbow Surg 18(6):837–844. doi:10.1016/j.jse.2009.06.004
Maldonado ZM, Seebeck J, Heller MO, Brandt D, Hepp P, Lill H, Duda GN (2003) Straining of the intact and fractured proximal humerus under physiological-like loading. J Biomech 36(12):1865–1873
Gardner MJ, Nork SE, Huber P, Krieg JC (2010) Less rigid stable fracture fixation in osteoporotic bone using locked plates with near cortical slots. Injury 41(6):652–656. doi:10.1016/j.injury.2010.02.022
Epari DR, Kassi JP, Schell H, Duda GN (2007) Timely fracture-healing requires optimization of axial fixation stability. J Bone Jt Surg Am 89(7):1575–1585. doi:10.2106/JBJS.F.00247
Brunner A, Resch H, Babst R, Kathrein S, Fierlbeck J, Niederberger A, Schmolz W (2012) The Humerusblock NG: a new concept for stabilization of proximal humeral fractures and its biomechanical evaluation. Arch Orthop Trauma Surg 132(7):985–992. doi:10.1007/s00402-012-1503-x
Brunner A, Weller K, Thormann S, Jockel JA, Babst R (2010) Closed reduction and minimally invasive percutaneous fixation of proximal humerus fractures using the Humerusblock. J Orthop Trauma 24(7):407–413. doi:10.1097/BOT.0b013e3181c81b1c
Kralinger F, Gschwentner M, Wambacher M, Smekal V, Haid C (2008) Proximal humeral fractures: what is semi-rigid? Biomechanical properties of semi-rigid implants, a biomechanical cadaver based evaluation. Arch Orthop Trauma Surg 128(2):205–210. doi:10.1007/s00402-007-0512-7
Steinberg EL, Rath E, Shlaifer A, Chechik O, Maman E, Salai M (2013) Carbon fiber reinforced PEEK optima—a composite material biomechanical properties and wear/debris characteristics of CF-PEEK composites for orthopedic trauma implants. J Mech Behav Biomed Mater 17:221–228. doi:10.1016/j.jmbbm.2012.09.013
Röderer G, Scola A, Schmolz W, Gebhard F, Windolf M, Hofmann-Fliri L (2013) Biomechanical in vitro assessment of screw augmentation in locked plating of proximal humerus fractures. Injury 44(10):1327–1332. doi:10.1016/j.injury.2013.05.008
Unger S, Erhart S, Kralinger F, Blauth M, Schmoelz W (2012) The effect of in situ augmentation on implant anchorage in proximal humeral head fractures. Injury 43(10):1759–1763. doi:10.1016/j.injury.2012.07.003
Lill H, Hepp P, Korner J, Kassi JP, Verheyden AP, Josten C, Duda GN (2003) Proximal humeral fractures: how stiff should an implant be? A comparative mechanical study with new implants in human specimens. Arch Orthop Trauma Surg 123(2–3):74–81. doi:10.1007/s00402-002-0465-9
Bottlang M, Doornink J, Byrd GD, Fitzpatrick DC, Madey SM (2009) A nonlocking end screw can decrease fracture risk caused by locked plating in the osteoporotic diaphysis. J Bone Jt Surg Am 91(3):620–627. doi:10.2106/JBJS.H.00408
Dietrich M, Meier C, Lattmann T, Zingg U, Gruninger P, Platz A (2008) Complex fracture of the proximal humerus in the elderly. Locking plate osteosynthesis vs hemiarthroplasty. Chirurg 79(3):231–240. doi:10.1007/s00104-007-1436-z
Schliemann B, Hartensuer R, Koch T, Theisen C, Raschke MJ, Kösters C, Weimann A (2015) Treatment of proximal humerus fractures with a CFR-PEEK plate: 2-year-results of a prospective study and comparison to fixation with a conventional locking plate. J Shoulder Elbow Surg 24(8):1282–1288. doi:10.1016/j.jse.2014.12.028
Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS (2011) Predicting failure after surgical fixation of proximal humerus fractures. Injury 42(11):1283–1288. doi:10.1016/j.injury.2011.01.017
Owsley KC, Gorczyca JT (2008) Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures [corrected]. J Bone Jt Surg Am 90(2):233–240. doi:10.2106/JBJS.F.01351
Katthagen JC, Schwarze M, Meyer-Kobbe J, Voigt C, Hurschler C, Lill H (2014) Biomechanical effects of calcar screws and bone block augmentation on medial support in locked plating of proximal humeral fractures. Clin Biomech (Bristol, Avon) 29(7):735–741. doi:10.1016/j.clinbiomech.2014.06.008
Zhang L, Zheng J, Wang W, Lin G, Huang Y, Zheng J, Edem Prince GA, Yang G (2011) The clinical benefit of medial support screws in locking plating of proximal humerus fractures: a prospective randomized study. Int Orthop 35(11):1655–1661. doi:10.1007/s00264-011-1227-5
Zhang W, Zeng L, Liu Y, Pan Y, Zhang W, Zhang C, Zeng B, Chen Y (2014) The mechanical benefit of medial support screws in locking plating of proximal humerus fractures. PLoS One 9(8):e103297. doi:10.1371/journal.pone.0103297
Schliemann B, Seifert R, Rosslenbroich SB, Theisen C, Wahnert D, Raschke MJ, Weimann A (2015) Screw augmentation reduces motion at the bone-implant interface: a biomechanical study of locking plate fixation of proximal humeral fractures. J Shoulder Elbow Surg 4(12):1968–1973. doi:10.1016/j.jse.2015.06.028
Kathrein S, Kralinger F, Blauth M, Schmoelz W (2013) Biomechanical comparison of an angular stable plate with augmented and non-augmented screws in a newly developed shoulder test bench. Clin Biomech (Bristol, Avon) 28(3):273–277. doi:10.1016/j.clinbiomech.2012.12.013
Roderer G, Gebhard F, Krischak G, Wilke HJ, Claes L (2011) Biomechanical in vitro assessment of fixed angle plating using a new concept of locking for the treatment of osteoporotic proximal humerus fractures. Int Orthop 35(4):535–541. doi:10.1007/s00264-010-1021-9
Euler SA, Hengg C, Wambacher M, Spiegl UJ, Kralinger F (2014) Allogenic bone grafting for augmentation in two-part proximal humeral fracture fixation in a high-risk patient population. Arch Orthop Trauma Surg. doi:10.1007/s00402-014-2128-z
Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG (2007) The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma 21(3):185–191. doi:10.1097/BOT.0b013e3180333094
Neviaser AS, Hettrich CM, Beamer BS, Dines JS, Lorich DG (2011) Endosteal strut augment reduces complications associated with proximal humeral locking plates. Clin Orthop Relat Res 469(12):3300–3306. doi:10.1007/s11999-011-1949-0
Somasundaram K, Huber CP, Babu V, Zadeh H (2013) Proximal humeral fractures: the role of calcium sulphate augmentation and extended deltoid splitting approach in internal fixation using locking plates. Injury 44(4):481–487. doi:10.1016/j.injury.2012.10.030
Tan E, Lie D, Wong MK (2014) Early outcomes of proximal humerus fracture fixation with locking plate and intramedullary fibular strut graft. Orthopedics 37(9):e822–e827. doi:10.3928/01477447-20140825-60
Zhu L, Liu Y, Yang Z, Li H, Wang J, Zhao C, Chen X, Zhang Y (2014) Locking plate fixation combined with iliac crest bone autologous graft for proximal humerus comminuted fracture. Chin Med J 127(9):1672–1676
Westerhoff P, Graichen F, Bender A, Halder A, Beier A, Rohlmann A, Bergmann G (2009) In vivo measurement of shoulder joint loads during activities of daily living. J Biomech 42(12):1840–1849. doi:10.1016/j.jbiomech.2009.05.035
Katthagen JC, Schwarze M, Warnhoff M, Voigt C, Hurschler C, Lill H (2016) Influence of plate material and screw design on stiffness and ultimate load of locked plating in osteoporotic proximal humeral fractures. Injury 47(3):617–624. doi:10.1016/j.injury.2016.01.004
Acknowledgements
This work was supported by the fund “Innovative Medical Research” (IMF, Grant SC 211305 to B.S. and A.W.) of the University of Münster Medical School and by the ASSOCIATION FOR ORTHOPAEDIC RESEARCH (AFOR). B.S. had a research fellowship from the University of Münster Medical School. Depuy Synthes and Lima Corporate provided implants and instruments used in this project. Neither funding source played a role in the study design, collection, analysis, and interpretation of the data and in the preparation and editing process of the manuscript. The manuscript was edited by the American Journal Experts service (http://www.AJE.com).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Twelve pairs’ human cadaveric specimens were used for the study. In life, all the donors provided written consent of their own free will for the use of their bodies for research purposes. Institutional review board approval was obtained prior to the study (IRB No. 2014-421-f-N).
Additional information
B. Schliemann and R. Seifert contributed equally to this study.
Rights and permissions
About this article
Cite this article
Schliemann, B., Seifert, R., Theisen, C. et al. PEEK versus titanium locking plates for proximal humerus fracture fixation: a comparative biomechanical study in two- and three-part fractures. Arch Orthop Trauma Surg 137, 63–71 (2017). https://doi.org/10.1007/s00402-016-2620-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-016-2620-8