Abstract
Introduction
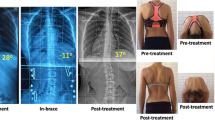
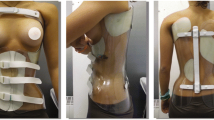
Scoliosis in patients with neuromuscular disease is a common issue and leads to secondary impairment. It is thus important to help such patients to regain and retain best possible stability to improve their quality of life. One option is the double-shelled brace (DSB). The aim of this study was to provide information on the degree of correction when using a DSB on patients with neuromuscular scoliosis.
Methods
We included patients with neuromuscular scoliosis treated with double-shelled braces in this retrospective study. Radiographs of the full spine were taken with and without the DSB, the Cobb angles were measured and compared. The correction was expressed in percent of the lumbar and thoracic Cobb angles. In addition, compounding factors such as age, sex, type of the curves, and movement disorder were included.
Results
We analyzed data from 84 patients with scoliosis with different neuromuscular disorders. The mean age was 12.3 years (± 5.9). In the lumbar spine we detected an improvement of 27.5% (SD ± 32.9), in the thoracic spine 25.3% (SD ± 38.0).
Interpretation
Short-term corrections with a double-shelled brace in neuromuscular scoliosis present an average improvement of one fourth of the lumbar and thoracic Cobb angles and, independent of age, sex, movement disorder, shape or type of the curve. Only spasticity has an influence on the lumbar scoliosis outcome.



Similar content being viewed by others
Abbreviations
- DSB:
-
Double-shelled brace
- CP:
-
Cerebral palsy
- NMS:
-
Neuromuscular scoliosis
- MMC:
-
Myelomeningocele
- SMA:
-
Spinal muscle atrophy
- GMFCS:
-
Gross Motor Function Classification System
- AP:
-
Anterior–posterior
References
Murphy R, Mooney J (2019) Currents concept in neuromuscular scoliosis. Pediatr Orthop 2:220–227
Berven S, Bradford DS (2002) Neuromuscular scoliosis: causes of deformity and principles for evaluation and management. Semin Neurol 22(2):167–178
McCarthy RE (1999) Management of neuromuscular scoliosis. Orthop Clin North Am 30(3):435–449
Miller F (2007) Spinal deformity secondary to impaired neurologic control. J Bone Jt Surg Am 89(Suppl 1):143–147
Saito N, Ebara S, Ohotsuka K, Kumeta H, Takaoka K (1998) Natural history of scoliosis in spastic cerebral palsy. Lancet 351(9117):1687–1692
Vialle R, Thévenin-Lemoine C, Mary P (2013) Neuromuscular scoliosis. Orthop Traumatol Surg Res 99(1 Suppl):S124–S139
Madigan RR, Wallace SL (1981) Scoliosis in the institutionalized cerebral palsy population. Spine (Phila Pa 1976) 6(6):583–590
Miller A, Temple T, Miller F (1996) Impact of orthoses on the rate of scoliosis progression in children with cerebral palsy. J Pediatr Orthop 16(3):332–335
Rutz E, Brunner R (2013) Management of spinal deformity in cerebral palsy: conservative treatment. J Child Orthop 7(5):415–418
Soo B, Howard JJ, Boyd RN, Reid SM, Lanigan A, Wolfe R et al (2006) Hip displacement in cerebral palsy. J Bone Jt Surg Am 88(1):121–129
Larnert P, Risto O, Hägglund G, Wagner P (2014) Hip displacement in relation to age and gross motor function in children with cerebral palsy. J Child Orthop 8(2):129–134
Yoshida K, Kajiura I, Suzuki T, Kawabata H (2018) Natural history of scoliosis in cerebral palsy and risk factors for progression of scoliosis. J Orthop Sci 23(4):649–652
Oikonomidis S, Meyer C, Scheyerer MJ, Grevenstein D, Eysel P, Bredow J (2019) Lumbar spinal fusion of low-grade degenerative spondylolisthesis (Meyerding grade I and II): do reduction and correction of the radiological sagittal parameters correlate with better clinical outcome? Arch Orthop Trauma Surg 140:1155–1162
Karampalis C, Tsirikos AI (2014) The surgical treatment of lordoscoliosis and hyperlordosis in patients with quadriplegic cerebral palsy. Bone Jt J 96-B(6):800–806
Kotwicki T, Jozwiak M (2008) Conservative management of neuromuscular scoliosis: personal experience and review of literature. Disabil Rehabil 30(10):792–798
Terjesen T, Lange JE, Steen H (2000) Treatment of scoliosis with spinal bracing in quadriplegic cerebral palsy. Dev Med Child Neurol 42(7):448–454
Tsirikos AI, Chang WN, Dabney KW, Miller F, Glutting J (2003) Life expectancy in pediatric patients with cerebral palsy and neuromuscular scoliosis who underwent spinal fusion. Dev Med Child Neurol 45(10):677–682
Obid P, Yiu K, Cheung K, Kwan K, Ruf M, Cheung JPY (2020) Magnetically controlled growing rods in early onset scoliosis: radiological results, outcome, and complications in a series of 22 patients. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03518-z
Bohtz C, Meyer-Heim A, Min K (2011) Changes in health-related quality of life after spinal fusion and scoliosis correction in patients with cerebral palsy. J Pediatr Orthop 31(6):668–673
Canavese F, Marengo L, Corradin M, Mansour M, Samba A, Andreacchio A et al (2018) Deep postoperative spine infection treated by negative pressure therapy in patients with progressive spinal deformities. Arch Orthop Trauma Surg 138(4):463–469
Bosshard A, Nadarajalingam M, Keller S, Brunner R, Camathias C, Rutz E (2019) Double-shelled brace to correct spinal deformity in non-ambulatory patients with cerebral palsy—a STROBE-compliant study. J Pediatr Perinatol Child Health 3:152–162
Cobb J (1948) Outline for the study of scoliosis. American Acad Orthop Surg Instr Course Lect 5:261–275
Marklund T (1978) Scoliosis angle. Conceptual basis and proposed definition. Acta Radiol Diagn (Stockh) 19(1A):78–88
McMaster WC, Clayton K (1980) Spinal bracing in the institutionalized person with scoliosis. Spine (Phila Pa 1976) 5(5):459–462
Olafsson Y, Saraste H, Al-Dabbagh Z (1999) Brace treatment in neuromuscular spine deformity. J Pediatr Orthop 19(3):376–379
Thometz JG, Simon SR (1988) Progression of scoliosis after skeletal maturity in institutionalized adults who have cerebral palsy. J Bone Jt Surg Am 70(9):1290–1296
Hollenbeck MDSM (2019) The pros and cons of operating early versus late in the progression of cerebral palsy scoliosis. Spine Deform 7:489–493
Forst J, Forst KD, Hengstler K (1997) Besonderheiten in der Behandlung von Skoliosen bei Muskelsystemerkrankungen. Z Orthop Unfall 135(2):95–105
Piggott H (1980) The natural history of scoliosis in myelodysplasia. J Bone Jt Surg Br 62-B(1):54–58
Samuelsson L, Eklöf O (1988) Scoliosis in myelomeningocele. Acta Orthop Scand 59(2):122–127
Müller EB, Nordwall A (1994) Brace treatment of scoliosis in children with myelomeningocele. Spine 19(2):151–155
Thomson JD, Banta JV (2001) Scoliosis in cerebral palsy: an overview and recent results. J Pediatr Orthop B 10(1):6–9
Acknowledgements
Many thanks to the participants and their parents. Special thanks to my loving husband for moral support and to my father and grand-father, which both made it possible for me to pursue a medical career.
Author information
Authors and Affiliations
Contributions
Design (NV, ER, RB), Data acquisition (NV, MK), Analysis and interpretation of data (CC, ER, NV, RB), Drafting and critical revision of the manuscript (NV, MK, RB, CC, ER).
Corresponding author
Ethics declarations
Conflict of interest
Each author declares that they have no conflict of interest.
Ethical approval
This study, approved by the local ethical committee (EKNZ, ID 2017-01076), was conducted according to the current version of the World Medical Association Declaration of Helsinki.
Consent
There was no patient consent given. The further use of the radiographs that were already made is ethically sound. A signed consent would be difficult to acquire due to the high number of subjects. Although it is a single center study the patients are coming from all over Switzerland. This is also a reason why it would be difficult to get a signed consent. However, the data was of course made anonymous and untraceable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vogel-Tgetgel, N.D., Kläusler, M., Brunner, R. et al. Short-term outcome of double-shelled braces in neuromuscular scoliosis. Arch Orthop Trauma Surg 142, 115–122 (2022). https://doi.org/10.1007/s00402-020-03600-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03600-6