Abstract
Purpose
Benign lesions of the proximal femur region, such as simple bone cysts, aneurysmal bone cysts, and fibrous dysplasia, are common in children. Benign lesions may cause pathologic fractures, limb length inequities, and growth disturbances. Differential diagnoses, e.g., malignant bone tumors and osteomyelitis, are sometimes difficult to rule out.
Objective
We aimed to evaluate outcomes in children with benign lesions of the proximal femur treated with curettage, bone grafting, and plate fixation.
Methods
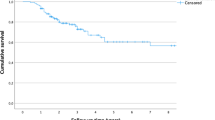
In this retrospective study, we included 30 children (median age 10.5 years; range 1.1–17.8 years) suffering from bone cysts and tumor-like lesions of the proximal femur region treated between 2002 and 2018. We analyzed plain X-ray images and CT scans in all children and obtained MRI scans in a selected group of children (63.3%). We examined histopathologic biopsy results for all bone lesions before initiating treatment. Surgical management comprised tumor curettage with adjuvant high-speed drilling and allogenic bone grafting supplemented by bone graft substitutes before plate fixation. Median follow-up interval was 87 months (range 24–156 months). We evaluated the healing of lesions according to Capanna’s classification and rated functional outcomes according to Merle d’Aubigné and Postel score.
Results
Overall, 25 of 30 (83.3%) patients were admitted to hospital because of a pathologic fracture. We diagnosed simple bone cysts in 15 (50.0%) patients, aneurysmal bone cysts in 7 (23.5%) patients, and fibrous dysplasia in 8 (26.5%) patients. Bone consolidation was achieved in 22 of 30 (73.3%) patients after a mean of 5 months (range 3–7 months). The main complication was recurrence of the lesion in 4 of 30 (13.3%) patients. With respect to the Merle d’Aubigné and Postel scores, 17 of 30 (56.7%) patients obtained an excellent result (18 points), while 12 (40.0%) patients had a good result (15–17 points) and only 1 (3.3%) patient had a fair result (14 points).
Conclusion
Surgical treatment of bone cysts and tumor-like lesions of the proximal femur by local resection or destruction of the lesion, followed by filling the defect with bone graft material and internal stabilization represents a safe and effective treatment option in children.
Level of evidence
Therapeutic, retrospective comparative study—Level III






Similar content being viewed by others
Abbreviations
- ABC:
-
Aneurysmal bone cyst
- BCI:
-
Bone cyst index
- CT:
-
Computer tomography
- FD:
-
Fibrous dysplasia
- MRI:
-
Magnetic resonance imaging
- SBC:
-
Simple bone cyst
References
van den Berg H, Kroon HM, Slaar A, Hogendoorn P (2008) Incidence of biopsy-proven bone tumors in children: a report based on the Dutch pathology registration “PALGA.” J Pediatr Orthop 28(1):29–35. https://doi.org/10.1097/BPO.0b013e3181558cb5
De Mattos CBR, Binitie O, Dormans JP (2012) Pathological fractures in children. Bone Joint Res 10:272–280
Jackson WF, Theologis TN, Gibbons CL, Mathews S, Kambouroglou G (2007) Early management of pathological fractures in children. Injury 38:194–200
Ortiz EJ, Isler MH, Navia JE, Canosa R (2005) Pathologic fractures in children. Clin Orthop Relat Res 432:116–126
Snyder BD, Hauser-Kara DA, Hipp JA et al (2006) Predicting fracture through benign skeletal lesions with quantitative computed tomography. J Bone Joint Surg [Am] 88:55–70
Pireau N, De Gheldere A, Mainard-Simard L, Lascombes P, Docquier PL (2011) Fracture risk in unicameral bone cyst: is magnetic resonance imaging a better predictor than plain radiography? Acta Orthop Belg 77:230–238
Wilkins RM (2000) Unicameral bone cysts. J Am Acad Orthop Surg 8:217–224
Lokiec F, Wientroub S (1998) Simple bone cyst: etiology, classification, pathology, and treatment modalities. J Pediatr Orthop B 7(4):262–273
Cottalorda J, Kohler R, Sales de Gauzy J et al (2004) Epidemiology of aneurysmal bone cyst in children: a multicenter study and literature review. J Pediatr Orthop B 13:389–394
Mankin HJ, Hornicek FJ, Ortiz-Cruz E, Villafuerte J, Gebhardt MC (2005) Aneurysmal bone cyst: a review of 150 patients. J Clin Oncol 23:6756–6762
Sullivan RJ, Meyer JS, Dormans JP, Davidson RS (1999) Diagnosing aneurysmal and unicameral bone cysts with magnetic resonance imaging. Clin Orthop Relat Res 366:186–190. https://doi.org/10.1097/00003086-199909000-00024
Erol B, Topkar MO, Caliskan E, Erbolukbas R (2015) Surgical treatment of active or aggressive aneurysmal bone cysts in children. J Pediatr Orthop B 24(5):461–468. https://doi.org/10.1097/BPB.0000000000000173
DiCaprio MR, Enneking WF (2005) Fibrous dysplasia: pathophysiology, evaluation, and treatment. J Bone Joint Surg [Am] 87:1848–1864
Harris WH, Dudley HR, Barry RJ (1962) The natural history of fibrous dysplasia: an orthopaedic, pathological, and roentgenographic study. J Bone Joint Surg [Am] 44:207–233
Ippolito E, Bray EW, Corsi A et al (2003) Natural history and treatment of fibrous dysplasia of bone: a multicenter clinicopathologic study promoted by the European Pediatric Orthopaedic Society. J Pediatr Orthop B 12:155–177
Guille JT, Kumar SJ, MacEwen GD (1998) Fibrous dysplasia of the proximal part of the femur: long-term results of curettage and bone-grafting and mechanical realignment. J Bone Joint Surg [Am] 80:648–658
Kushare IV, Colo D, Bakhshi H, Dormans JP (2014) Fibrous dysplasia of the proximal femur: surgical management options and outcomes. J Child Orthop 8:505–511
Tong Z, Zhang W, Jiao N, Wang K, Chen B, Yang T (2013) Surgical treatment of fibrous dysplasia in the proximal femur. Exp Ther Med 5:1355–1358
Erol B, Topkar MO, Aydemir AN, Okay E, Caliskan E, Sofulu O (2016) A treatment strategy for proximal femoral benign bone lesions in children and recommended surgical procedures: retrospective analysis of 62 patients. Arch Orthop Trauma Surg 136(8):1051–1061. https://doi.org/10.1007/s00402-016-2486-9
Merle d’Aubigné R, Postel M (1954) Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am 36:451–475
Rutz E, Brunner R (2010) The pediatric LCP hip plate for fixation of proximal femoral osteotomy in cerebral palsy and severe osteoporosis. J Pediatr Orthop 30(7):726–731. https://doi.org/10.1097/BPO.0b013e3181efb86b
Capanna R, Dal Monte A, Gitelis S, Campanacci M (1982) The natural history of unicameral bone cyst after steroid injection. Clin Orthop Relat Res 166:204–211
R Core Team (2018) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available online at https://www.R-project.org/.
Anderson MJ (2001) A new method for non-parametric multivariate analysis of variance. Austral Ecol 26:32–46
WJ Metsemakers M Morgenstern E Senneville et al Fracture-Related Infection (FRI) group (2020) General treatment principles for fracture-related infection: recommendations from an international expert group. Arch Orthop Trauma Surg. 140(8):1013–1027. https://doi.org/10.1007/s00402-019-03287-4 ([Epub 2019 Oct 29])
Dormans JP, Pill SG (2002) Fractures through bone cysts: unicameral bone cysts, aneurysmal bone cysts, fibrous cortical defects, and nonossifying fibromas. Instr Course Lect 51:457–467
Vasconcellos DA, Yandow SM, Grace AM, Moritz BM, Marley LD, Fillman RR (2007) Cyst index: a nonpredictor of simple bone cyst fracture. J Pediatr Orthop 27:307–310
Donaldson S, Wright JG (2011) Recent developments in treatment for simple bone cysts. Curr Opin Pediatr 23:73–77
Dormans JP, Sankar WN, Moroz L, Erol B (2005) Percutaneous intramedullary decompression, curettage, and grafting with medical-grade calcium sulfate pellets for unicameral bone cysts in children: a new minimally invasive technique. J Pediatr Orthop 25:804–811
Dong C, Klimek P, Abächerli C, De Rosa V, Krieg AH (2020) Percutaneous cyst aspiration with injection of two different bioresorbable bone cements in treatment of simple bone cyst. J Child Orthop 14(1):76–84. https://doi.org/10.1302/1863-2548.14.190155
Canavese F, Wright JG, Cole WG, Hopyan S (2011) Unicameral bone cysts: comparison of percutaneous curettage, steroid, and autologous bone marrow injections. J Pediatr Orthop 31:50–55
Hou HY, Wu K, Wang CT et al (2011) Treatment of unicameral bone cyst: surgical technique. J Bone Joint Surg [Am] 93:92–99
Mik G, Arkader A, Manteghi A, Dormans JP (2009) Results of a minimally invasive technique for treatment of unicameral bone cysts. Clin Orthop Relat Res 467(11):2949–2954. https://doi.org/10.1007/s11999-009-1008-2
Roposch A, Saraph V, Linhart WE (2004) Treatment of femoral neck and trochanteric simple bone cysts. Arch Orthop Trauma Surg 124(7):437–442. https://doi.org/10.1007/s00402-004-0702-5
Luengo-Alonso G, Mellado-Romero M, Shemesh S, Ramos-Pascua L, Pretell-Mazzini J (2019) Denosumab treatment for giant-cell tumor of bone: a systematic review of the literature. Arch Orthop Trauma Surg 139(10):1339–1349. https://doi.org/10.1007/s00402-019-03167-x ([Epub 2019 Mar 15])
Biesecker JL, Marcove RC, Huvos AG, Miké V (1970) Aneurysmal bone cysts. A clinicopathologic study of 66 cases. Cancer 26(3):615–625. https://doi.org/10.1002/1097-0142(197009)26:3%3c615::aid-cncr2820260319%3e3.0.co;2-i
Gibbs CP Jr, Hefele MC, Peabody TD, Montag AG, Aithal V, Simon MA (1999) Aneurysmal bone cyst of the extremities factors related to local recurrence after curettage with a high-speed burr. J Bone Joint Surg Am. 81(12):1671–1678. https://doi.org/10.2106/00004623-199912000-00003
Dormans JP, Guirguis HB, Johnston DR, Khurana JS (2004) Surgical treatment and recurrence rate of aneurysmal bone cysts in children. Clin Orthop Relat Res 421:205–211
Ward AE; RATeS Study Group (2019) RATeS (Re-Admissions in Trauma and Orthopaedic Surgery): a prospective regional service evaluation of complications and readmissions. Arch Orthop Trauma Surg 139(10):1351–1360. https://doi.org/10.1007/s00402-019-03144-4 ([Epub 2019 Mar 20])
Marcove RC, Sheth DS, Takemoto S, Healey JH (1995) The treatment of aneurysmal bone cyst. Clin Orthop Relat Res 311:157–163
Fritz J, Sonnow L, Morris CD (2019) Adjuvant MRI-guided percutaneous cryoablation treatment for aneurysmal bone cyst. Skeletal Radiol 48(7):1149–1153. https://doi.org/10.1007/s00256-018-3115-1
Matta JM, Mehne DK, Roffi R (1986) Fractures of the acetabulum. Early results of a prospective study. Clin Orthop Relat Res 205:241–250
Øvre S, Sandvik L, Madsen JE, Røise O (2005) Comparison of distribution, agreement and correlation between the original and modified Merle d’Aubigné-Postel Score and the Harris Hip Score after acetabular fracture treatment: moderate agreement, high ceiling effect and excellent correlation in 450 patients. Acta Orthop 76(6):796–802. https://doi.org/10.1080/17453670510045390
Acknowledgement
All authors have read and agreed to the published version of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization WL, JM, RT, ER; formal analysis WL, RT, JD; investigation WL, RT; resources WL, JM, RT; statistical analysis, J.D.; writing—original draft preparation, WL, RT, ER; writing—review and editing JM; visualization WL, RT; supervision, JM, RT, ER.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
This retrospective study was approved by the Ethics Committee of the Silesian Medical University, Katowice, Poland (PCN/0022/KB/99/20 dated June 5th, 2020).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tomaszewski, R., Rutz, E., Mayr, J. et al. Surgical treatment of benign lesions and pathologic fractures of the proximal femur in children. Arch Orthop Trauma Surg 142, 615–624 (2022). https://doi.org/10.1007/s00402-020-03687-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03687-x