Abstract
Introduction
Accurate measurement of combined component anteversion (CA) is important in evaluating the radiographic outcomes following total hip arthroplasty (THA). The aim of the present study was to evaluate the accuracy and reliability of a novel radiographic method in estimating CA in THA.
Materials and methods
The radiographs and computer tomography of patients who underwent a primary THA were retrospectively reviewed, to measure the radiographic CA (CAr), defined as the angle between a line connecting the center of the femoral head to the most anterior rim of the acetabular cup and a line connecting the center of the femoral head to the base of the femoral head to allow a comparison with the CA measured on the CT (CACT). Subsequently, a computational simulation was performed to evaluate the effect of cup anteversion, inclination, stem anteversion, and leg rotation on the CAr and develop a formula that would correct the CAr according to the acetabular cup inclination based on the best-fit equation.
Results
In the retrospective analysis of 154 THA, the average CAr_cor, and CACT were 53 ± 11° and 54 ± 11° (p > 0.05), respectively. A strong correlation was found between CAr and CACT (r = 0.96, p < 0.001), with an average bias of − 0.5° between CAr_cor and CACT. In the computational simulation, the CAr was strongly affected by the cup anteversion, inclination, stem anteversion, and leg rotation. The formula to convert the CAr to CA_cor was: CA-cor = 1.3*Car − (17* In (Cup Inclination) − 31.
Conclusion
The combined anteversion measurement of THA components on the lateral hip radiograph is accurate and reliable, implying that it could be routinely used postoperatively but also in patients with persistent complaints following a THA.
Level of evidence
Cross-sectional study, Level III.
Similar content being viewed by others
Introduction
Accurate measurement of component orientation is important in evaluating the radiographic outcomes following total hip arthroplasty (THA), as component malposition might be associated with early implant failure, impingement, dislocation, and early implant failure [5, 11, 16, 18, 20, 22, 24]. The concept of combined anteversion (CA), introduced by Ranawat [21] as the sum of acetabular and femoral component anteversion, is gaining popularity as its importance in preventing THA dislocation has been widely demonstrated [7, 10, 17, 30]. Several methods have been proposed for accurate measurement of acetabular cup anteversion on plain radiographs [1, 6, 8, 12, 14, 26]; however, no method exists to assess femoral stem anteversion and consequently CA. Although computed tomography (CT) is considered the gold standard in evaluating CA, plain radiographs are commonly used postoperatively, as CT scans are expensive and expose patients to a considerable amount of radiation [2, 3, 7].
The Ranawat sign [15] was introduced by Lucas and Scott as an intraoperative maneuver to assess CA. Hereby, the operated leg is placed in zero degrees of extension and 45° of internal rotation. If the base of the femoral head is parallel to the acetabular cup, a combined anteversion of 45° could be assumed. Based on the Ranawat sign and the intraoperative observation that the proportion of the anterior femoral head, which was not covered by the acetabular cup, could give an estimation of the CA (Fig. 1), a simple method was developed to assess the CA on cross-table lateral hip radiographs. The aim of the present study was: (1) to verify the novel method with a computational simulation and (2) to evaluate its accuracy and reliability in estimating CA in THA.
Materials and methods
Retrospective study design, inclusion, and exclusion criteria
The present study was approved by the state ethical committee (BASEC Nr.: 2022-01344) and was entirely conducted at the authors' institution. The medical records and radiographs of patients who underwent a rotational profile CT scan (including the pelvis and knee) at our institution either as part of a randomized control trial comparing a three-dimensional CT-based preoperative to the standard two-dimensional planning (NCT05120063) or because of hip instability (consecutive patients from 01/2012 until 12/2021), were retrospectively reviewed. The inclusion criteria were adult patients, who underwent a primary THA, and had a CT scan and cross-table lateral hip radiograph, 3 months postoperatively. The exclusion criteria were revision THA, gross hip deformity making complex hip reconstruction necessary, such as greater trochanter advancement, acetabular augmentation, femoral osteotomy, and use of a revision stem, as those patients might have increased risk for THA dislocation, which could have affected the subgroup analysis.
Patient characteristics, surgical technique, and implants
A total of 154 THA in 148 patients (males: 53, females: 95) with an average age of 59 ± 11 (range: 24 to 91) years were included. The majority of the patients (THA = 108/154, 70%) underwent a rotational CT as part of a randomized control trial, whereas 46/154 (30%) received a CT scan due to an early hip dislocation (< 3 months postoperative). All cases were performed with a standardized minimally invasive direct anterior approach in a supine position using the AMIS® Mobile Leg Positioner [Medacta International SA, Castel San Pietro, Switzerland] under spinal or general anesthesia. An imaging intensifier was used intraoperatively to assess the acetabular cup anteversion in all cases. The implants used in the current study included a cementless press-fit acetabular cup (April [Symbios, Yverdon-Les-Bains, Switzerland] (n = 108) or Versafit [Medacta International SA, Castel San Pietro, Switzerland] (n = 46) and a cementless straight femoral stem (Harmony® [Symbios, Yverdon-Les-Bains, Switzerland] (n = 62) or Quadra-H [Medacta International SA, Castel San Pietro, Switzerland] (n = 46) and a three-dimensional anatomical stem (SPS® Evolution (n = 46) [Symbios, Yverdon-Les-Bains, Switzerland].
Radiographic measurements
A standardized cross-table lateral hip radiograph was performed 3 months postoperatively. This was taken in a supine position, with the foot rotated internally at 15° and the contralateral hip flexed to 90° to prevent interference in the radiographic projection. The cassette was held perpendicular to the examination table and the direction of the beam was parallel to the examination table and 45° cephalad to the long axis of the body.
For the measurement of the radiographic CA (CAr) in the cross-table lateral radiograph, the best-fit circle was applied to the femoral head. CAr was defined as the angle between the line connecting the center of the femoral head to the most anterior rim of the acetabular cup and the line connecting the center of the femoral head to the base of the femoral head, defined as the point where the head loses its sphericity (Fig. 2).
Cross-table lateral radiograph of a left hip demonstrating the method used to measure the radiographic combined anteversion of the components (CAr). A best-fit circle was applied to the femoral head. CAr was defined as the angle between the line connecting the center of the femoral head (best-fitted circle) to the most anterior rim of the acetabular cup and the line connecting the center of the femoral head to the base of the femoral head, defined as the point where the head loses its sphericity
CT measurements
CT scans of the pelvis and the distal femur were obtained with a 64-slice CT scanner (SOMATOM Definition AS, Siemens Healthineers) using a standardized protocol. CT images were acquired with automated tube voltage selection (CARE kV, reference 120 kV) and tube current modulation (CARE Dose4D, reference 147mAs), a collimation width of 0.6 mm, a rotation time of 0.5 s, and a pitch of 0.8.
The CACT was measured on the axial CT image of the pelvis as the sum of the acetabular cup and femoral stem anteversion. Acetabular cup anteversion was defined as the line connecting the most anterior and posterior point of the acetabular cup at the level of the hip rotational center and a reference line drawn perpendicular to a line between the most posterior pelvic margins (Fig. 3A) [23]. Femoral stem anteversion was defined as the angle between a line connecting the center of the femoral head to the center of the base of the femoral stem's neck and the line connecting the posterior aspect of the medial and lateral femoral condyles (Fig. 3B) [29].
Axial computed tomography (CT) image demonstrating the method used to measure the A acetabular anteversion as the line connecting the most anterior and posterior point of the acetabular cup and a reference line drawn perpendicular to a line between the most posterior pelvic margins and B femoral anteversion defined as the angle between a line connecting the center of the femoral head to the center of the base of the femoral stem neck and the line connecting the posterior aspect of the medial and lateral femoral condyles
Computer simulation
As a first step, CT-based three-dimensional models of the entire lower extremity of a patient who underwent a primary THA at our institution were reconstructed. The acetabular cup was implanted at 30° of anteversion and 40° of inclination, whereas the femoral stem at 15° of anteversion. The acetabular cup version was subsequently increased (from 10 to 60°) without changing the inclination and the femoral stem anteversion, with the foot kept in 15° of internal rotation. The view was then set to 45°, to simulate the cross-table lateral hip radiography, and the angle between the femoral head center to the anterior acetabular rim and the base of the femoral head was measured (Fig. 4A–E). Next, the femoral version was increased (from − 15° to 45°) without changing the acetabular version (30°) and inclination (40°) with the foot kept at 15° of internal rotation (Fig. 5A–E). Then the acetabular cup inclination was increased (from 15° to 75°) without changing the acetabular (30°) and femoral (15°) versions with the foot kept at 15° of internal rotation. Finally, the leg was externally rotated from (− 30° to 45°) to investigate without changing the acetabular version (30°), inclination (40°), and femoral stem version (15°) to investigate the effect of leg rotation on the measurement of the radiologic combined anteversion. According to the computer simulation data, the equation of best fit was used to develop a formula that would correct the CAr according to the acetabular inclination (CA_cor). The CAr was then corrected for acetabular cup inclination (CAr_cor) measured on an anteroposterior pelvic radiograph to allow for direct comparison with the CA measured on the CT scan (CACT).
CT-based three-dimensional models of a patient with THA. The acetabular cup anteversion was increased (from 15°, 30°, 45°, 60°) (A–D) while the cup inclination (40°) femoral stem anteversion (15°) remained constant. Increasing the acetabular cup anteversion (E) increased the proportion of the femoral head, which remained uncovered from the acetabular cup
CT-based three-dimensional models of a patient with THA. The femoral stem anteversion was increased (from − 15°, 0°, 15°, 30°, 45°) while the acetabular cup anteversion and inclination remained constant (cup anteversion 30°, cup inclination 40°). Increasing the femoral stem anteversion (from A–E) increased the portion of the femoral head, which remained uncovered from the acetabular cup. The polar axis (line passing through the center of the stem neck and the center of the prosthetic head) as defined by Pour et al. [25] (red arrow) also moved anteriorly with increased femoral stem anteversion (from A–E)
Assessment of accuracy and inter-/intra-observer reliability
The accuracy of the CAr_cor was defined as the proximity to the CACT. The CAr_cor was measured by three orthopedic residents (FC, EW, and CZ) and one hip fellow (DD) blinded to the CACT. The average CAr_cor of the four above-mentioned measurements was compared to the CACT. For the intra-observer reliability, one examiner (DD) reassessed the CAr_cor after a 4-week interval to avoid recall bias without comparison to the previous measurements. The inter-observer reliability of the CAr_cor was assessed by comparing the results of the four examiners. The intra-observer and inter-observer reliabilities of the measurements were evaluated using an average-measure intra-class correlation coefficient (ICC) with a two-way random-effects model for absolute agreement. Plain radiographs were presented to each examiner in random order by a research assistant who did not participate in the reliability and accuracy sessions.
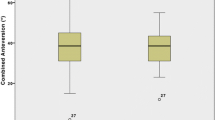
Subgroup analysis of patients with and without THA dislocation
The CACT of patients with and without THA dislocation was compared to detect any differences. The percentage of the THA components with a CACT within the “safe zone” of 25–50°, as defined by Dorr [7], was also evaluated.
Statistical analysis
Descriptive statistics used averages, standard deviation, range, and percentages to present the data. All parameters were tested with the Kolmogorov–Smirnov test for normality. When the criteria for normality were met, a two-tailed t test was used. Otherwise, the Wilcoxon signed-rank test was applied. The Bland–Altman plots were used to compare the agreement between the average CAr_cor and CACT [4]. Pearson correlation coefficient was applied to investigate the relationship between CAr_cor and CACT but also the effect of cup anteversion, inclination, leg rotation, and femoral stem anteversion of the CAr. The level of significance was set to p ≤ 0.05. All the statistical analyses were performed using SPSS version 23 software (SPSS Inc., Chicago, Illinois).
Results
Radiographic and CT measurements
The average CAr_cor was 53 ± 11 (range: 20 to 77)°, whereas the average cup inclination was 39 ± 5 (range: 24 to 55)°. The average acetabular and femoral anteversion, measured on CT, was 34 ± 7 (range: 17 to 59)° and 22 ± 10 (range: -6 to 50)°, respectively, whereas the average CACT was 54 ± 11 (range: 21 to 78)°. Patients with THA dislocation demonstrated a significantly higher average CACT (62 ± 9)° compared to patients without a THA dislocation (52 ± 10°) (p < 0.001). The majority of THAs with and without early dislocation demonstrated a combined anteversion outside the CA” safe zone” (96% and 57%, respectively).
Computer simulation
The CAr was positively correlated to the femoral stem (r = 0.99, p < 0.001) and acetabular cup anteversion (r = 0.99, p < 0.001). The CAr was also positively correlated with cup inclination ((r = 0.99, p < 0.001). meaning, that the higher the cup inclination, the higher the CAr for the same CACT (Fig. 6). The formula to convert the CAr to CAr_cor was: CAr_cor = 1.3* Car − (17* In (Cup Inclination) − 31) (Table 1). The leg rotation was also positively correlated to CAr (r = 0.99, p < 0.001), meaning the more externally rotated leg, the more CAr would be measured on the lateral cross-table hip radiograph.
Accuracy and inter-/intra-observer reliability
Accuracy: The Bland–Altman plot demonstrated an average bias of − 0.5° (95% limits of agreement: − 6.7 to 5.6)° between CAr_cor and CACT (Fig. 7). Pearson’s correlation demonstrated a strong correlation between CAr and CACT (r = 0.96, p < 0.001).
Bland–Altman plot for agreement between CAr_cor and CACT. *Blue line: bias of CAr_cor compared to CACT. Green line: 95% confidence interval of the bias. Red dotted lines: 95% limit of agreement between CAr_cor and CACT. Bias close to zero and narrow limits indicate that the method studied (CAr_cor) could replace the gold standard (CACT)
Reliability: The intra-observer and inter-observer reliability were in excellent agreement between CAr and CACT (0.94 and 0.93), respectively.
Discussion
Adverse clinical outcomes related to implant malposition have stimulated an increasing interest in optimal component orientation in primary THA. Accurate measurement of component anteversion is important in evaluating the radiographic outcomes of THA but also patients with persistent complaints following THA. Although several methods have been proposed for accurate measurement of acetabular cup anteversion on plain radiographs, no data are available on combined component anteversion. The aim of the present study was to evaluate the accuracy and reliability of a novel radiographic method on the lateral hip radiograph in estimating CA in THA. The study demonstrated a high accuracy of the CAr_cor with an average bias of − 0.5° compared to the CACT, with excellent inter- and intra-observer reliability, suggesting that the CAr_cor could be routinely used postoperatively to estimate the CA of the THA components.
The CAr_cor essentially represents the proportion of the anterior femoral head, which is not covered by the acetabular cup (Fig. 1). By increasing the acetabular anteversion, it is expected that a larger proportion of the anterior head will be uncovered. A similar effect is anticipated by increasing the femoral stem anteversion. This is confirmed by the computer simulation performed in the present study (Figs. 4 and 5), which demonstrated a positive linear correlation with both femoral stem, and acetabular cup anteversion, meaning that by increasing acetabular or femoral anteversion, the proportion of the femoral head, which remains uncovered from the acetabular cup will also increase. Pour et al. [19] in a simulation study demonstrated that by increasing both acetabular cup and femoral stem anteversion, the polar axis (line passing through the center of the stem neck and the center of the prosthetic head) moved anteriorly, which is in accordance with our observation (Fig. 5).
The importance of CA in establishing an impingement-free range of motion and preventing THA dislocation has been well-described and the suggested “safe zones” are based on simulation studies [25, 27, 28, 30] or clinical observations [21]. However, the surgical approach might affect the CA, and consequently different “safe zones” might be needed for other surgical approaches. Dorr et al. [7] reported an average CA of 37 ± 7° following a navigated THA through a mini-posterior approach in 47 patients, with 96% of the THAs within the defined “safe zone” of 25 to 50°. Li et al. [13] reported an average CA of 23 ± 13° in 501 patients (545), who underwent a THA through the lateral approach, with only 44% of the THAs being within the “safe zone” of 25 to 50°. Nevertheless, no dislocations have been reported. Jackson et al. [9] demonstrated an average CA of 44 ± 10° in 29 patients who underwent a THA through the direct anterior approach, with 79% of the hips being within the “safe zone”. In the present study, the average CA in 148 patients (154 hips) who underwent a THA through the minimally invasive anterior approach was 54 ± 11°, which is markedly higher than the other approaches reported in the literature. The CA in patients without THA dislocation was 52 ± 10°, with 57% of the THAs having a combined anteversion outside Dorr´s “safe zone”. Patients with THA dislocation demonstrated a significantly higher CA (62 ± 8°) with 96% having a CA outside the Dorr´s “safe zone”. These results might suggest that a surgical approach-specific “safe zone” might be necessary to evaluate the risk of THA dislocation.
The present study should be interpreted in light of its potential limitations. The most obvious drawback was that the lateral hip radiograph in the current study was performed in a standardized protocol, by a well-trained staff of our orthopedic department, but as demonstrated in the present study, leg rotation can strongly influence the measurement of CA on the lateral cross-table hip radiograph. Hence, the CAr_cor should not be used to measure the CA of THA components in lateral radiographs not performed in the above-mentioned standardized matter, as leg rotation might affect the results. Also, the femoral heads used in the present study had a distinct base, which was clearly identified on lateral radiographs (Fig. 2). Therefore, the current method cannot be used with prosthetic heads which do not have an easily identified base. Furthermore, it should be noted, that only a limited number of stem types (straight tapered and anatomical) were analyzed. Although their design might be similar to other implants available, other stems should be evaluated to confirm the findings of the current study.
In conclusion, the result of the present study suggests that the CAr_cor measurement on cross-table lateral hip radiographs is accurate and reliable, implying that it could be routinely used postoperatively to estimate the CA of the THA components. More patients should be recruited in future studies to confirm the validity and accuracy of the CAr on a larger scale and with different THA designs.
Availability of data and materials
The materials described in the manuscript, including all relevant raw data, will be freely available to any researcher wishing to use them for non-commercial purposes, without breaching participant confidentiality.
References
Ackland MK, Bourne WB, Uhthoff HK (1986) Anteversion of the acetabular cup. Measurement of angle after total hip replacement. J Bone Jt Surg Br 68(3):409–413
Arai N, Nakamura S, Matsushita T, Suzuki S (2010) Minimal radiation dose computed tomography for measurement of cup orientation in total hip arthroplasty. J Arthroplasty 25(2):263–267
Arora V, Hannan R, Beaver R, Fletcher T, Harvie P (2017) A cadaver study validating CT assessment of acetabular component orientation: the Perth CT hip protocol. Skeletal Radiol 46(2):177–183
Bland JM, Altman DG (1995) Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet 346(8982):1085–1087
D’Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW Jr (2000) The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Jt Surg Am 82(3):315–321
Derbyshire B, Diggle PJ, Ingham CJ, Macnair R, Wimhurst J, Jones HW (2014) A new technique for radiographic measurement of acetabular cup orientation. J Arthroplasty 29(2):369–372
Dorr LD, Malik A, Dastane M, Wan Z (2009) Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res 467(1):119–127
Hassan DM, Johnston GH, Dust WN, Watson LG, Cassidy D (1995) Radiographic calculation of anteversion in acetabular prostheses. J Arthroplasty 10(3):369–372
Jackson JB 3rd, Martin JR, Christal A, Masonis JL, Springer BD, Mason JB (2020) The direct anterior approach total hip arthroplasty reliably achieves “safe zones” for combined anteversion. Arthroplasty Today 6(4):651–654
Jolles BM, Zangger P, Leyvraz PF (2002) Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty 17(3):282–288
Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ (1998) Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty 13(5):530–534
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR (1978) Dislocations after total hip-replacement arthroplasties. J Bone Jt Surg 60(2):217–220
Li L, Zhang Y, Lin YY et al (2020) A specific anteversion of cup and combined anteversion for total hip arthroplasty using lateral approach. Orthop Surg 12(6):1663–1673
Liaw CK, Hou SM, Yang RS, Wu TY, Fuh CS (2006) A new tool for measuring cup orientation in total hip arthroplasties from plain radiographs. Clin Orthop Relat Res 451:134–139
Lucas D (1994) The Ranawat sign. A specific maneuver to assess component positioning in total hip arthroplasty. J Orthop Tech 2:59–61
Murphy WS, Yun HH, Hayden B, Kowal JH, Murphy SB (2018) The safe zone range for cup anteversion is narrower than for inclination in THA. Clin Orthop Relat Res 476(2):325–335
Nakashima Y, Hirata M, Akiyama M et al (2014) Combined anteversion technique reduced the dislocation in cementless total hip arthroplasty. Int Orthop 38(1):27–32
Patel AB, Wagle RR, Usrey MM, Thompson MT, Incavo SJ, Noble PC (2010) Guidelines for implant placement to minimize impingement during activities of daily living after total hip arthroplasty. J Arthroplasty 25(8):1275–1281
Pour AE, Schwarzkopf R, Patel KP, Anjaria M, Lazennec JY, Dorr LD (2021) Is combined anteversion equally affected by acetabular cup and femoral stem anteversion? J Arthroplasty 36(7):2393–2401
Pryce GM, Sabu B, Al-Hajjar M et al (2022) Impingement in total hip arthroplasty: a geometric model. Proc Inst Mech Eng H. https://doi.org/10.1177/09544119211069472
Ranawac CS, Maynard MJ (1991) Modern technique of cemented total hip arthroplasty. Tech Orthop 6(3):17–25
Sadhu A, Nam D, Coobs BR, Barrack TN, Nunley RM, Barrack RL (2017) Acetabular component position and the risk of dislocation following primary and revision total hip arthroplasty: a matched cohort analysis. J Arthroplasty 32(3):987–991
Stem ES, O’Connor MI, Kransdorf MJ, Crook J (2006) Computed tomography analysis of acetabular anteversion and abduction. Skeletal Radiol 35(6):385–389
Wan Z, Boutary M, Dorr LD (2008) The influence of acetabular component position on wear in total hip arthroplasty. J Arthroplasty 23(1):51–56
Weber M, Woerner M, Craiovan B et al (2016) Current standard rules of combined anteversion prevent prosthetic impingement but ignore osseous contact in total hip arthroplasty. Int Orthop 40(12):2495–2504
Widmer KH (2004) A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty 19(3):387–390
Widmer KH (2020) The impingement-free, prosthesis-specific, and anatomy-adjusted combined target zone for component positioning in THA depends on design and implantation parameters of both components. Clin Orthop Relat Res 478(8):1904–1918
Widmer KH, Zurfluh B (2004) Compliant positioning of total hip components for optimal range of motion. J Orthop Res 22(4):815–821
Wines AP, McNicol D (2006) Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty 21(5):696–701
Yoshimine F (2006) The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech 39(7):1315–1323
Funding
Open access funding provided by University of Zurich. No funding was received for this work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by DD, CZ, PM and FC. The first draft of the manuscript was written by DD and a major revision was performed by POZ. CZ also performed the stimulation analysis. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have nothing to disclose that would bias the content of the manuscript.
Ethical approval
Kantonale Ethikkommission Zürich, BASEC Nr.: 2022-01344.
Informed consent
All the participants have given informed consent for the present study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dimitriou, D., Zindel, C., Winkler, E. et al. A novel method for evaluating combined component anteversion in total hip arthroplasty on cross-table lateral hip radiographs. Arch Orthop Trauma Surg 143, 5977–5984 (2023). https://doi.org/10.1007/s00402-023-04825-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04825-x