Abstract
Purpose
To determine the frequency and distribution of Adverse Events (AE) in obstetrics departments at Spanish hospitals.
Methods
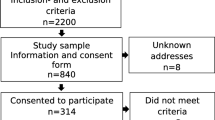
We present a retrospective cohort study including 816 women admitted to the obstetrics departments at 41 hospitals that took part in the National Adverse Effects Study in Spain (ENEAS) and an extension of this study in all hospitals located in two Autonomous Regions. To identify AE, nurses from each participating hospital examined all medical records, and completed a validated screening guide. A team of external reviewers evaluated the medical records of all women who met at least one of the criteria in the screening guide to verify all AE. The main outcome measure was the incidence of AE during hospitalization.
Results
The cumulative incidence of patients with obstetric care-related AE was 3.6 % (95 % CI 2.3–4.8). The most frequent AE were those related with surgical interventions or procedures (59.4 %). None of the AE detected were considered severe. 36.7 % of the AE lengthened the woman’s hospital stay, and 13.3 % led to hospital admission. Additional procedures were needed after 71.9 % of the AE, and additional treatment was needed after 59.4 %. 56.3 % of the AE were considered preventable.
Conclusions
Obstetric care is characterized by generally younger ages among patients, their low frequency of comorbidities and high expectations for successful outcomes of care. However, some factors can increase obstetric risk and favor the appearance of preventable incidents and AE. Systems are needed to detect preventable AE, and measures are needed to reduce risks or attenuate their consequences.
Similar content being viewed by others
References
Kohn L, Corrigan JM, Donaldson MS (eds) (1999) To err is human; building a safer health system. National Academy Press, Washington
Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG et al (1991) Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. New Engl J Med 324:70–76
Wilson RM, Runciman WB, Gibberd RW, Harrisson BT, Newby L, Hamilton JD et al (1995) The quality in Australian health care study. Med J Aust 163:458–471
Michel P, Minodier C, Lathelize M, Moty-Monnereau C, Domecq S, Chaleix M et al (2010) Les événements indésirables graves associés aux soins observés dans les établissements de santé Résultats des enquêtes nationales menées en 2009 et 2004. Dossiers Solidarité et Santé 17:1–18
Aranaz JM, Aibar C, Vitaller J, Ruiz P, Limón R, Terol E, ENEAS work group (2008) Incidence of adverse events related to health care in Spain: results of the Spanish National Study of Adverse Events. J Epidemiol Commun Health 62:1022–1029
Soop M, Fryksmark U, Koster M, Haglund B (2009) The incidence of adverse events in Swedish hospitals: a retrospective medical record review study. Int J Qual Health Care 21:285–291
Wilson RM, Michel P, Olsen S, Gibberd RW El-Assady R, Rasslan O et al (2012) Patient safety in developing countries: retrospective estimation of scale and nature of harm to patients in hospital. BMJ 344: e832. doi:10.1136/bmj.e832. Available at: http://www.bmj.com/content/344/bmj.e832. Accessed 7 Jan 2014
Gambone JC, Reiter RC (2008) Elements of a successful quality improvement and patient safety program in obstetrics and gynecology. Obstet Gynecol Clin North Am 35:129–145
Foster AJ, Fung I, Caughey S, Oppenheimer L, Beach C, Shojania KG, Van Walraven C (2006) Adverse events detected by clinical surveillance on an obstetric service. Obstet Gynecol 108:1073–1083
Aibar C, Júdez D (2005) Estudio autonómico de efectos adversos. ENEAS Aragon. Informe técnico no 1. Servicio Aragonés de Salud, Zaragoza
Moris J (2008) Estudio de los efectos adversos en la atención hospitalaria en el Principado de Asturias. Consejería de Salud y Servicios Sanitarios. Gobierno del Principado de Asturias, Oviedo
Aranaz JM y el Grupo de Estudio del Proyecto IDEA (2004) Proyecto IDEA: Identificación de efectos adversos. Rev Calidad Asistencial 19: 14–8. Available at: http://proyectoidea.com/index2.htm. Accessed 7 Jan 2014
World Health Organization (2009) More than words. Conceptual framework for the international classification for patient safety. Technical report. WHO. Available at: http://www.who.int/patientsafety/implementation/taxonomy/icps_technical_report_en.pdf. Accessed 7 Jan 2014
Tormo MJ, Dal-Ré R, Pérez-Albarracín G (1998) Ética e Investigación. In: Principios, aplicaciones y casos prácticos sobre la revisión de los aspectos éticos de la investigación epidemiológica. Barcelona: Sociedad Española de Epidemiología
Foster AJ, Worthington JR, Hawken S, Bourke M, Rubens F, Shojania K, Walraven C (2011) Using prospective clinical surveillance to identify adverse events in hospital. BMJ Qual Saf 20:756–763
Florea A, Caughey S, Westland J, Berckmans M, Kennelly C, Beach C et al (2010) The Ottawa Hospital quality incident notification system for capturing adverse events in obstetrics. J Obstet Gynaecol Can 32:657–662
Aranaz-Andres JM, Aibar-Remón C, Limón-Ramírez R, Amarilla A, Restrepo FR, Urroz O et al (2011) Prevalence of adverse events in the hospitals of five Latin American countries: results of the Iberoamerican study of adverse events (IBEAS). BMJ Qual Saf 20:1043–1051
King’s Fund (2008) Safe births: everybody’s business. An independent inquiry into the safety of maternity services in England. In: Walker I, Grise E (eds) King’s Fund, London
Joint Commission (2004) Preventing infant death and injury during delivery. Sentinel Event Alert Issue 30. Available at: http://www.jointcommission.org/assets/1/18/SEA_30.PDF. Accessed 7 Jan 2014
Aibar L, Rabanaque MJ, Mozas J, Puertas A, Aranaz JM, Aibar C (2014) Improving patient safety by detecting obstetric care-related adverse events: application of a new screening guide. Arch Gynecol Obstet 289:945–952
Millar J, Mattke S and the Members of the OECD Patient Safety Panel (2004) Selecting indicators for patient safety at the health systems level in OECD countries. OECD health technical papers no. 18. Paris
Institute for Healthcare Improvement (2006) Perinatal trigger tool. Available at: http://www.ihi.org/knowledge/Pages/Tools/PerinatalTriggerTool.aspx. Accessed 7 Jan 2014
Nielsen M, Mann S (2008) Team function in obstetrics to reduce errors and improve outcomes. Obstet Gynecol Clin N Am 35:81–95
Acknowledgments
This work was supported by the Ministry of Health of Spain.
Conflict of interest
The authors declare no conflicts of interest in connection with this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aibar, L., Rabanaque, M.J., Aibar, C. et al. Patient safety and adverse events related with obstetric care. Arch Gynecol Obstet 291, 825–830 (2015). https://doi.org/10.1007/s00404-014-3474-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3474-3