Abstract
Background
Dealing with work-related stress is highly prevalent for employees in Gynecology Medicine. Junior physicians, in particular, have to face high working demands and challenges while starting their medical career after graduation. Job resources (i.e., social support) and personal resources (coping skills) might reduce job strain. The evidence for supportive and effective mental health interventions for clinicians is limited. Offering psychosocial skill training for entrants in Gynecology Medicine is expected to be highly beneficial. Following this, the present pilot study focused on strengthening physicians’ psychosocial skills and analyzed the effects of innovative training for junior gynecologists working in German hospitals.
Methods
Coping skills training for junior gynecologists was offered as group training for 12 weekly sessions over a time period of 3 months. Physicians were randomized to either an intervention group (IG) receiving the training (n = 38) or a control group (CG; n = 40). Training content involved developing and learning coping skills as well as solution-focused and cognitive behavioral counselling for junior gynecologists. Study outcomes were (1) perceived occupational stress, (2) emotional exhaustion, (3) resilience coping behavior, (4) emotion regulation skills and (5) job satisfaction. Surveys were distributed at baseline (T0), after the training (T1), after 3 (T2) and 6 months (T3).
Results
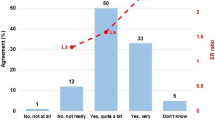
Junior gynecologists (IG) reported a significant decrease in perceived job stress and emotional exhaustion from baseline to all follow-ups, whereas the control group did not show any comparable results. A clear positive value of the mental health promotion program was also noticeable with regard to job satisfaction and increased coping skills (i.e., emotion regulation). Overall satisfaction with the skill training was high: gynecologists reported high scores for training design, content, received outcome and overall satisfaction with the training.
Conclusions
In this pilot study, participating in a psychosocial skills training course adapted for gynecology clinicians was associated with reductions in perceived job stress, exhaustion and improvements in coping skills and satisfaction. Modified psychosocial skills training may be a time-efficient tool to support gynecologists in their performance and well-being, which may have positive implications for patient care.

Similar content being viewed by others
Abbreviations
- ANCOVA:
-
Analysis of covariance
- b :
-
Beta weight
- BRCS:
-
Brief Resilient Coping Scale
- CI:
-
Confidence interval
- COPSOQ:
-
Copenhagen Psychosocial Questionnaire
- d :
-
Effect size
- ERSQ:
-
Emotion Regulation Skills Questionnaire
- N:
-
Numbers
- M:
-
Mean
- MBI:
-
Maslach Burnout Inventory
- MD:
-
Median
- PSQ:
-
Perceived Stress Questionnaire
- SD:
-
Standard deviation
References
Emmons SL, Nichols M, Schulkin J, James KE, Cain JM (2006) The influence of physician gender on practice satisfaction among obstetrician gynecologists. Am J Obstet Gynecol 194:1728–1738
Bauer J, Groneberg DA, Brueggmann D (2016) Gender-based workplace assessment in gynecology and obstetrics in Germany: results from the iCEPT Study. Arch Gynecol Obstet 294:317–326
Esteves SC, Hamada A, Kondray V, Pitchika A, Agarwal A (2012) What every gynecologist should know about male infertility: an update. Arch Gynecol Obstet 286:217–229
Graham J, Ramirez A (2002) Improving the working lives of cancer clinicians. Eur J Cancer Care 11:188–192
Rasmussen V, Turnell A, Butow P, Juraskova I, Kirsten L, Wiener L, Patenaude A, Hoekstra-Weebers J, Grassi L (2016) Burnout among psychosocial oncologists: an application and extension of the effort-reward imbalance model. Psychooncology 25:194–202
Keeton K, Fenner DE, Johnson TRB, Hayward RA (2007) Predictors of physician career satisfaction, work-life balance, and burnout. Obstet Gynecol 109:949–955
Becker JL, Milad MP, Klock SC (2006) Burnout, depression, and career satisfaction: cross-sectional study of obstetrics and gynecology residents. Am J Obstet Gynecol 195:1444–1449
Shanafelt TD, Boone S, Tan L (2012) Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 172:1377–1385
Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM (1996) Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet 347:724–728
Brooks SK, Chalder T, Gerada C (2011) Doctors vulnerable to psychological distress and addictions: treatment from the Practitioner Health Programme. J Ment Health 20:157–164
Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, Edwards S, Wiedermann BL, Landrigan CP (2008) Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ Clin Res Ed 336:488–491
West CP, Shanafelt TD (2007) Physician well-being and professionalism. Minn Med 90:44–46
Ruitenburg MM, Frings-Dresen MHW, Sluiter JK (2012) The prevalence of common mental disorders among hospital physicians and their association with self-reported work ability: a cross-sectional study. BMC Health Serv Res 12:292
Shanafelt TD (2009) Enhancing meaning in work: a prescription for preventing physician burnout and promoting patient-centered care. JAMA 302:1338–1340
Williams ES, Manwell LB, Konrad TR, Linzer M (2007) The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manag Rev 32:203–212
Hancke K, Igl W, Toth B (2014) Work—life balance of German gynecologists: a web-based survey on satisfaction with work and private life. Arch Gynecol Obstet 289:123–129
Carver CS, Scheier MF, Weintraub JK (1989) Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol 56:267–283
Macedo T, Wilheim L, Gonçalves R, Coutinho ES, Vilete L, Figueira I, Ventura P (2014) Building resilience for future adversity: a systematic review of interventions in non-clinical samples of adults. BMC Psychiatry 14:227–241
Ramaswamy R, Williams A, Clark EM, Kelley AS (2014) Communication skills curriculum for foreign medical graduates in an internal medicine residency program. J Am Geriatr Soc 62:2153–2158
Puskar KR, Sereika S, Tusaie-Mumford K (2003) Effect of the teaching kids to cope (TKC) program on outcomes of depression and coping among rural adolescents. J Child Adolesc Psychiatr Nurs 16:71–80
Tan L, Wang MJ, Modini M, Joyce S, Mykletun A, Christensen H, Harvey SB (2014) Preventing the development of depression at work: a systematic review and meta-analysis of universal interventions in the workplace. BMC Med 12:74
Krasner MS, Epstein RM, Beckman H (2009) Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physician. JAMA 302:1284–1293
Czabała C, Charzyńska K, Mroziak B (2011) Psychosocial interventions in workplace mental health promotion: an overview. Health Promot Int 26(Suppl 1):i70–i84. doi:10.1093/heapro/dar1050
Lagerveld SE, Blonk RW, Brenninkmeijer V, Wijngaards-de Meij L, Schaufeli WB (2012) Work-focused treatment of common mental disorders and return to work: a comparative outcome study. J Occup Health Psychol 17:220–234
Lazarus R, Folkman S (1984) Stress, appraisal, and coping. Springer Publishing Co, New York
Malouff JM, Thorsteinsson EB, Schutte NS (2007) The efficacy of problem solving therapy in reducing mental and physical health problems: a meta-analysis. Clin Psychol Rev 27:46–57
D’Zurilla T, Nezu A, Dobson KS (2010) Problem-solving therapy. Handbook of cognitive-behavioral therapies. Guilford Press, New York
Levenstein S, Prantera C, Varvo V, Scribano ML, Berto E, Luzi C (1993) Development of the Perceived Stress Questionnaire: a new tool for psychosomatic research. J Psychsom Res 37:19–32
Kristensen T, Hannerz H, Høgh A, Borg V (2005) The Copenhagen Psychosocial Questionnaire (COPSOQ). A tool for the assessment and improvement of the psychosocial work environment. Scand J Work Environ Health 31:438–449
Nuebling M, Hasselhorn HM (2010) The Copenhagen Psychosocial Questionnaire in Germany: from the validation of the instrument to the formation of a job-specific database of psychosocial factors at work. Scand J Public Health 38:120–124
Schaufeli W, Leiter M, Maslach C, Jackson S (1996) Maslach Burnout Inventory—General Survey (MBI-GS). In: Maslach C, Jackson SE, Leiter MP (eds) Maslach Burnout Inventory Manual. Consulting Psychologists Press, Palo Alto
Berking M, Znoj H (2008) Development and validation of a self-report instrument for the assessment of emotion-specific regulation skills (ERSQ-27). Z Psychiatrie Psychol Psychother 56:141–153
Sinclair VG, Wallston KA (2004) The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment 11:94–101
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. Stat Soc Ser 57
Cohen J, Hillsdale NJ (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates, New York
Buchberger B, Heymann R, Huppertz H, Friepörtner K, Pomorin N, Wasem J (2011) The effectiveness of interventions in workplace health promotion as to maintain the working capacity of health care personal. GMS Health Technol Assess 1
Zimber A, Gregersen S, Kuhnert S, Nienhaus A (2010) Workplace health promotion through human resources development part I: development and evaluation of qualification programme for prevention of psychic stresses. Gesundheitswesen 72:209–215
Burton NW, Pakenham KI, Brown WJ (2008) Feasibility and effectiveness of psychosocial resilience training: a pilot study of the READY program. Psychol Health Med 15:266–277
Leppin AL, Gionfriddo MR, Sood A, Montori VM, Erwin PJ, Zeballos-Palacios C, Bora PR, Dulohery MM, Brito JP, Boehmer KR, Tilburt JC (2014) The efficacy of resilience training programs: a systematic review protocol. Syst Rev. doi:10.1186/2046-4053-3-20
Goldhagen BE, Kingsolver K, Stinnett SS, Rosdahl JA (2015) Stress and burnout in residents: impact of mindfulness-based resilience training. Adv Med Educ Pract 25:525–532
McCue JD, Sachs CL (1991) A stress management workshop improves residents’ coping skills. Arch Intern Med 151:2273–2277
Ospina-Kammerer V, Figley CR (2003) An evaluation of the respiratory one method (ROM) in reducing emotional exhaustion among family physician residents. Int J Emerg Ment Health 5:29–32
Shapiro SL, Astin JA, Bishop SR (2005) Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int J Stress Manag 12:164–176
Holton MK, Barry AE, Chaney JD (2015) Employee stress management: An examination of adaptive and maladaptive coping strategies on employee health. Work
Schneider S, Kingsolver K, Rosdahl J (2014) Physician coaching to enhance well-being: a qualitative analysis of a pilot intervention. Explore 10:372–379
Goodman MJ, Schorling JB (2012) A mindfulness course decreases burnout and improves well-being among healthcare providers. Int J Psychiatry Med 43:119–128
Pflugeisen BM, Drummond D, Ebersole D, Mundell K, Chen D (2016) Brief video-module administered mindfulness program for physicians: a pilot study. Explore 12:50–54
Huang SL, Li RH, Huang FY, Tang FC (2015) The potential for mindfulness-based intervention in workplace mental health promotion: results of a randomized controlled trial. PLoS One 10
West CP, Dyrbye LN, Rabatin JT, Call TG, Davidson JH, Multari A, Romanski SA, Hellyer JMH, Sloan JA, Shanafelt TF (2014) Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med 174:527–533
Sood A, Prasad K, Schroeder D, Varkey P (2011) Stress management and resilience training among Department of Medicine faculty: a pilot randomized clinical trial. J Gen Intern Med 26:858–861
Ayres J, Malouff JM (2007) Problem-solving training to help workers increase positive affect, job satisfaction, and life satisfaction. Eur J Work Organ Psychol 16:279–294
Kirkpatrick DL, Kirkpatrick DJ (2006) Evaluating training programs: the four levels. Berrett-Koehler Publishers, Oakland
McKensey A, Sullivan L (2016) Balint groups—helping trainee psychiatrists make even better use of themselves. Australas Psychiatry 24:84–87
Parker SD, Leggett A (2014) Reflecting on our practice: an evaluation of Balint groups for medical students in psychiatry. Australas Psychiatry 22:190–194
Van Roy K, Vanheule S, Inslegers R (2015) Research on Balint groups: a literature review. Patient Educ Couns 98:685–694
Lee E, Kealy D (2014) Revisiting Balint’s innovation: enhancing capacity in collaborative mental health care. J Interprof Care 28:466–470
Aust B, Ducki A (2004) Comprehensive Health promotion interventions at the workplace: experiences with health circles in Germany. J Occup Health Psychol 9:258–270
Köhler T, Janssen C, Platz SC, Reese JP, Lay J, Steinhausen S, Gloede T, Kowalski C, Schulz-Nieswandt F, Pfaff H (2010) Communication, social capital and workplace health management as determinants of the innovative climate in German banks. Int J Public Health 55:561–570
Warnecke E, Quinn S, Ogden K, Towle N, Nelson MR (2011) A randomised controlled trial of the effects of mindfulness practice on medical student stress levels. Med Educ 45:381–388
Shanafelt TD, Balch CM, Bechamps GJ (2009) Burnout and career satisfaction among American surgeons. Ann Surg 250:463–471
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare, they have no conflict of interest.
Ethical considerations
Ethical approval was granted by the Institutional Review Board of the Free University Berlin. The study is in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964.
Informed consent
Informed consent was obtained from all participating physicians included in this study.
Rights and permissions
About this article
Cite this article
Mache, S., Baresi, L., Bernburg, M. et al. Being prepared to work in Gynecology Medicine: evaluation of an intervention to promote junior gynecologists professionalism, mental health and job satisfaction. Arch Gynecol Obstet 295, 153–162 (2017). https://doi.org/10.1007/s00404-016-4223-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4223-6