Abstract
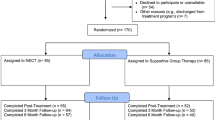
There is a need for interventions supporting patients with mental health conditions in coping with stigma and discrimination. A psycho-educational group therapy module to promote stigma coping and empowerment (STEM) was developed and tested for efficacy in patients with schizophrenia or depression. 30 clinical centers participated in a cluster-randomized clinical trial, representing a broad spectrum of mental health care settings: in-patient (acute treatment, rehabilitation), out-patient, and day-hospitals. As randomized, patients in the intervention group clusters/centers received an illness-specific eight sessions standard psychoeducational group therapy plus three specific sessions on stigma coping and empowerment (‘STEM’). In the control group clusters the same standard psychoeducational group therapy was extended to 11 sessions followed by one booster session in both conditions. In total, N = 462 patients were included in the analysis (N = 117 with schizophrenia spectrum disorders, ICD-10 F2x; N = 345 with depression, ICD-10 F31.3–F31.5, F32–F34, and F43.2). Clinical and stigma-related measures were assessed before and directly after treatment, as well as after 6 weeks, 6 months, and 12 months (M12). Primary outcome was improvement in quality of life (QoL) assessed with the WHO-QOL-BREF between pre-assessment and M12 analyzed by mixed models and adjusted for pre-treatment differences. Overall, QoL and secondary outcome measures (symptoms, functioning, compliance, internalized stigma, self-esteem, empowerment) improved significantly, but there was no significant difference between intervention and control group. The short STEM module has proven its practicability as an add-on in different settings in routine mental health care. The overall increase in empowerment in both, schizophrenia and depression, indicates patients’ treatment benefit. However, factors contributing to improvement need to be explored.
The study has been registered in the following trial registers. ClinicalTrials.gov: https://register.clinicaltrials.gov/ Registration number: NCT01655368. DRKS: https://www.drks.de/drks_web/ Registration number: DRKS00004217.

Similar content being viewed by others
References
Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M, INDIGO Study Group (2009) Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet 373(9661):408–415
Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rüsch N (2012) Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr Serv 63:963–973
Gaebel W, Rössler W, Sartorius N (eds) (2017) The stigma of mental illness–end of the story? Springer, Heidelberg
Gaebel W, Zäske H, Baumann AE, Klosterkötter J, Maier W, Decker P, Möller HJ (2008) Evaluation of the German WPA “Program against stigma and discrimination because of schizophrenia—Open the doors”: results from representative telephone surveys before and after 3 years of antistigma interventions. Schizophr Res 98:184–193
Henderson RC, Corker E, Hamilton S, Williams P, Pinfold V, Rose D, Webber M, Evans-Lacko S, Thornicroft G (2014) Viewpoint survey of mental health service users’ experiences of discrimination in England 2008−2012. Soc Psychiatry Psychiatr Epidemiol 49:1599–1608
Gronholm PC, Henderson C, Deb T, Thornicroft G (2017) Interventions to reduce discrimination and stigma: the state of the art. Soc Psychiatry Psychiatr Epidemiol 52:249–258
Schomerus G, Schwahn C, Holzinger A, Corrigan PW, Grabe HJ, Carta MG, Angermeyer MC (2012) Evolution of public attitudes about mental illness: a systematic review and meta-analysis. Acta Psychiatr Scand 125:440–452
Gaebel W, Riesbeck M, Siegert A, Zäske H, Zielasek J (2017) Improving treatment, prevention, and rehabilitation. In: Gaebel W, Roessler W, Sartorius N (eds) The stigma of mental illness-end of the story?. Springer International Publishing, Switzerland, pp 537–549
Brohan E, Slade M, Clement S, Thornicroft G (2010) Experiences of mental illness stigma, prejudice and discrimination: a review of measures. BMC Health Serv Res. https://doi.org/10.1186/1472-6963-10-80
Wahl OF (1989) Mental health consumers’ experience of stigma. Schizophr Bull 25:467–478
Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP (1989) A modified labeling theory approach to mental disorders: an empirical assessment. Amer Sociol Rev 54:400–423
Corrigan PW, Larson JE, Rüsch N (2009) Self-stigma and the “why try” effect: impact on life goals and evidence-based practices. World Psychiatry 8:75–81
Major B, O’Brien LT (2005) The social psychology of stigma. Annu Rev Psychol 56:393–421
Ilic M, Reinecke J, Bohner G, Hans-Onno R, Beblo T, Driessen M, Frommberger U, Corrigan PW (2011) Protecting self-esteem from stigma: a test of different strategies for coping with the stigma of mental illness. Int J Soc Psychiatry 58:246–257
Livingston JD, Boyd JE (2010) Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med 71:2150–2161
Gronholm PC, Thornicroft G, Laurens KR, Evans-Lacko S (2017) Mental health-related stigma and pathways to care for people at risk of psychotic disorders or experiencing first-episode psychosis: a systematic review. Psychol Med 47:1867–1879
Angermeyer M, Schomerus G (2012) A stigma perspective on recovery. World Psychiatry 11:163–164
Mittal D, Sullivan G, Chekuri L, Allee E, Corrigan PW (2012) Empirical studies of self-stigma reduction strategies: a critical review of the literature. Psychiatr Serv 63:974–981
Sibitz I, Provaznikova K, Lipp M, Lakeman R, Amering M (2013) The impact of recovery-oriented day clinic treatment on internalized stigma: preliminary report. Psychiatry Res 209:326–332
Roe D, Hasson-Ohayon I, Mashiach-Eizenberg M, Derhy O, Lysaker PH, Yanos PT (2014) Narrative enhancement and cognitive therapy (NECT) effectiveness: a quasi-experimental study. J Clin Psychol 70:303–312
Gerlinger G, Hauser M, De Hert M, Lacluyse K, Wampers M, Correll CU (2013) Personal stigma in schizophrenia spectrum disorders: a systematic review of prevalence rates, correlates, impact and interventions. World Psychiatry 12:155–164
Griffiths KM, Carron-Arthur B, Parsons A, Reid R (2014) Effectiveness of programs for reducing the stigma associated with mental disorders. A meta-analysis of randomized controlled trials. World Psychiatry 13:161–175
Mehta N, Clement S, Marcus E, Stona AC, Bezborodovs N, Evans-Lacko S, Palacios J, Docherty M, Barley E, Rose D, Koschorke M, Shidhaye R, Henderson C, Thornicroft G (2015) Evidence for effective interventions to reduce mental health-related stigma and discrimination in the medium and long term: systematic review. Br J Psychiatry 207:377–384
Büchter RB, Messer M (2017) Interventions for reducing self-stigma in people with mental illnesses: a systematic review of randomized controlled trials. Ger Med Sci. https://doi.org/10.3205/000248
Campbell MK, Piaggio G, Elbourne DR, Altman DG, CONSORT Group (2012) Consort 2010 statement: extension to cluster randomised trials. BMJ 345:e5661
Bäuml J, Pitschel-Walz G, Berger H, Gunia H (2009) Manual psychoeducation for schizophrenia [arbeitsbuch psychoedukation bei schizophrenie (APES)], 2nd edn. Schattauer, Stuttgart
Pitschel-Walz G, Bäuml J, Kissling W (2003) Psychoeducation for depression: manual for groups with patients and relatives [psychoedukation bei depressionen: manual zur leitung von patienten- und angehörigengruppen], 1st edn. Urban und Fischer, München
Hesse K, Klingberg S, Zäske H, Conrad B, Heise F, Gaebel W, Wölwer W, Richter J, Wernet T (2018) Coping with sigmatization and promoting empowerment (STEM) manual and worksheets for download [Stigmatisierung überwinden und empowerment fördern (STEM). Manual und Arbeitsblätter zum download]. http://psychose-psychotherapie.de/index.php/therapiemanuale. Accessed 9 Sept 2019
Yanos PT, Lucksted A, Drapalski AL, Roe D, Lysaker P (2015) Interventions targeting mental health self-stigma: a review and comparison. Psychiatr Rehabil J 38:171–178
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62
Kay SR, Opler LA, Fiszbein A (1986) The positive and negative syndrome scale (PANSS) rating manual. Soc Behav Sci Doc 17:28–29
Guy W, Bethesda MD (1976) Clinical Global Impressions (CGI) Scale. In: Guy W (ed) ECDEU assessment manual for psychopharmacology, revised. US Dept. Health, Education, and Welfare, Washington, pp 218–222
Frances A, Pincus HA, First MB (1994) The Global Assessment of Functioning Scale (GAF). Diagnostic and Statistical Manual of Mental Disorder–IV. American Psychiatric Association, Washington, p 32
Kemp R, David A (1996) Psychological predictors of insight and compliance in psychotic patients. Br J Psychiatry 169:444–450
Skevington SM, Lotfy M, O’Connell KA, WHOQOL Group (2004) The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res 13:299–310
Ritsher JB, Otilingam PG, Grajales M (2003) Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res 121:31–49
Rogers ES, Chamberlin J, Ellison ML, Crean T (1997) A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatr Serv 48:1042–1047
Wright ER, Gronfein WP, Owens TJ (2000) Deinstitutionalization, social rejection, and the self-esteem of former mental patients. J Health Soc Behav 41:68–90
Hardt J (2008) The symptom checklist-27-plus (SCL-27-plus): a modern conceptualization of a traditional screening instrument. GMS Psychosoc Med
Roick C, Kilian R, Matschinger H, Bernert S, Mory C, Angermeyer MC (2001) German adaptation of the client sociodemographic and service receipt inventory—an instrument for the cost of mental health care. Psychiatr Prax 28(Suppl 2):90
Priebe S (2012) Where is the progress? Psychiatr Prax 39:55–56
Amaresha AC, Kalmady SV, Joseph B, Agarwal SM, Narayanaswamy JC, Venkatasubramanian G, Muralidhar D, Subbakrishna DK (2018) Short term effects of brief need based psychoeducation on knowledge, self-stigma, and burden among siblings of persons with schizophrenia: a prospective controlled trial. Asian J Psychiatr 32:59–66
Jobe TH, Harrow M (2005) Long-term outcome of patients with schizophrenia: a review. Can J Psychiatry 50:892–900
Henderson C (2017) Disorder-specific Differences. In: Gaebel W, Roessler W, Sartorius N (eds) The stigma of mental illness-end of the story?. Springer International Publishing, Switzerland, pp 83–109
Zäske H, Degner D, Jockers-Scherübl M, Klingberg S, Klosterkötter J, Maier W, Möller HJ, Sauer H, Schmitt A, Gaebel W (2016) Experiences of stigma and discrimination in patients with first-episode schizophrenia. Nervenarzt 87:82–87
Kaiser CR, Miller CT (2001) Stop complaining! The social costs of making attributions to discrimination. Pers Soc Psychol Bull 27:254–263
Isaksson A, Corker E, Cotney J, Hamilton S, Pinfold V, Rose D, Rüsch N, Henderson C, Thornicroft G, Evans-Lacko S (2018) Coping with stigma and discrimination: evidence from mental health service users in England. Epidemiol Psychiatr Sci. 27:577–588
Acknowledgements
The study has been funded by a research grant of the Federal Ministry of Education and Research (BMBF; research Grant 01GX1011).
We want to thank all study participants and all collaborators of the STEM work group who contributed to this study.
STEM work group (all facilities are located in Germany): Gaebel W, Cleveland, H, Conradt B, Feiertag N, Heise F, Janssen B, Riesbeck M, Sauter S, Siegert A, Zäske H; Department of Psychiatry and Psychotherapy, Medical Faculty, Heinrich Heine University, LVR-Klinikum, Düsseldorf. Klingberg S, Hesse K, Richter J, Nentwich B; Department of Psychiatry and Psychotherapy, University of Tübingen. Ohmann C, Grebe J, See B, Verde P; Coordination Center for Clinical Trials, Medical Faculty, Heinrich Heine University, Düsseldorf. Icks, A; Institute for Health Services Research and Health Economics, Centre for Health and Society, Heinrich Heine University, Düsseldorf. Schneider F, Backes V; Department of Psychiatry, Psychotherapy and Psychosomatics, Medical Faculty, RWTH Aachen, Aachen. Wolff-Menzler C, Guse B; Department of Psychiatry, University Medical Center Göttingen, Göttingen. Bock T, Frey J; Department of Psychiatry and Psychotherapy of the University Medical Center Hamburg-Eppendorf. Jockers-Scherübl MC, Krüger T; Charité, Universitätsmedizin Berlin, Berlin, Germany Hennigsdorf: Oberhavel Kliniken GmbH, Klinik Hennigsdorf. Jessen F, Bechdolf A, v. Pützfeld V, Zarafonitis S. Department of Psychiatry and Psychotherapy, University of Cologne, Cologne. Kircher T, Konrad C. Department of Psychiatry and Psychotherapy, University of Marburg, Marburg. Falkai P, Schaub A. Department of Psychiatry and Psychotherapy, Ludwig Maximilian University, Munich. Rudolph M; Mittelrhein-Klinik for Psychosmatics and Rehabilitation, Bad Salzig. Köllner, V; Department of Psychosomatic Medicine, Mediclin Bliestal Clinic, Blieskastel. Schmidt-Ott G, Stock Gissendanner S; Department of Psychosomatics, Berolina Clinic Löhne. Linden, M, Lieberei B; Department of Behavioral Medicine, Rehabilitation Center Seehof, Berlin. Stuhlinger M; Psychiatric-psychotherapeutic Rehabilitation Center grund.stein, Tübingen. Sommerfeld S, Schumacher A, Krenge S; AHG Klinik, Waren. Gereke S, Mönter N, Navarro-Urena A; Psychiatric Practices, Berlin. Frosch G, Kuhlbusch FJ; Psychiatric Practices, Düsseldorf.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
J. Gallinat has received research funding from the German Federal Ministry of Education and Research, German Science Foundation, and speaker fees from Lundbeck, Janssen-Cilag, Lilly and Otsuka. All other authors state that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Gaebel, W., Zäske, H., Hesse, K. et al. Promoting stigma coping and empowerment in patients with schizophrenia and depression: results of a cluster-RCT. Eur Arch Psychiatry Clin Neurosci 270, 501–511 (2020). https://doi.org/10.1007/s00406-019-01064-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-019-01064-3