Abstract
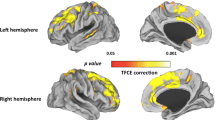
Increased severity of neurological soft signs (NSS) in schizophrenia have been associated with abnormal brain morphology in cerebello-thalamo-cortical structures, but it is unclear whether similar structures underlie NSS prior to the onset of psychosis. The present study investigated the relationship between severity of NSS and grey matter volume (GMV) in individuals at ultra-high risk for psychosis (UHR) stratified for later conversion to psychosis. Structural T1-weighted MRI scans were obtained from 56 antipsychotic-naïve UHR individuals and 35 healthy controls (HC). The UHR individuals had follow-up data (mean follow-up: 5.2 years) to ascertain clinical outcome. Using whole-brain voxel-based morphometry, the relationship between NSS and GMV at baseline was assessed in UHR, HC, as well as individuals who later transitioned (UHR-P, n = 25) and did not transition (UHR-NP, n = 31) to psychosis. NSS total and subscale scores except motor coordination were significantly higher in UHR compared to HC. Higher signs were also found in UHR-P, but not UHR-NP. Total NSS was not associated with GMV in the whole sample or in each group. However, in UHR-P individuals, greater deficits in sensory integration was associated with lower GMV in the left cerebellum, right insula, and right middle frontal gyrus. In conclusion, NSS are present in UHR individuals, particularly those who later transitioned to a psychotic disorder. While these signs show little overall variation with GMV, the association of sensory integration deficits with lower GMV in UHR-P suggests that certain brain areas may be implicated in the development of specific neurological abnormalities in the psychosis prodrome.



Similar content being viewed by others
Data availability
The data of this study are available upon request from the corresponding author.
Code availability
The analysis code of this study are available upon request from the corresponding author.
References
Hirjak D, Meyer-Lindenberg A, Fritze S, Sambataro F, Kubera KM, Wolf RC (2018) Motor dysfunction as research domain across bipolar, obsessive-compulsive and neurodevelopmental disorders. Neurosci Biobehav Rev 95:315–335. https://doi.org/10.1016/j.neubiorev.2018.09.009
Peralta V, Cuesta MJ (2017) Motor abnormalities: from neurodevelopmental to neurodegenerative through “functional” (neuro)psychiatric disorders. Schizophr Bull 43(5):956–971. https://doi.org/10.1093/schbul/sbx089
Hirjak D, Meyer-Lindenberg A, Sambataro F, Wolf RC (2021) Sensorimotor neuroscience in mental disorders: progress, perspectives and challenges. Schizophr Bull. https://doi.org/10.1093/schbul/sbab053
Garvey MA, Cuthbert BN (2017) Developing a motor systems domain for the NIMH RDoC program. Schizophr Bull 43(5):935–936. https://doi.org/10.1093/schbul/sbx095
Mittal VA, Bernard JA, Northoff G (2017) What can different motor circuits tell us about psychosis? An RDoC perspective. Schizophr Bull 43(5):949–955. https://doi.org/10.1093/schbul/sbx087
Buchanan RW, Heinrichs DW (1989) The Neurological Evaluation Scale (NES): a structured instrument for the assessment of neurological signs in schizophrenia. Psychiatry Res 27:335–350
Bombin I, Arango C, Buchanan RW (2005) Significance and meaning of neurological signs in schizophrenia: two decades later. Schizophr Bull 31:962–977. https://doi.org/10.1093/schbul/sbi028
Chan RCK, Gottesman II (2008) Neurological soft signs as candidate endophenotypes for schizophrenia: a shooting star or a Northern star? Neurosci Biobehav Rev 32:957–971. https://doi.org/10.1016/j.neubiorev.2008.01.005
Chan RCK, Cui H-R, Chu M-Y, Zhang T-H, Wang Y, Wang Y, Li Z, Lui SSY, Wang J-J, Cheung EFC (2018) Neurological soft signs precede the onset of schizophrenia: a study of individuals with schizotypy, ultra-high-risk individuals, and first-onset schizophrenia. Eur Arch Psychiatry Clin Neurosci 268(1):49–56. https://doi.org/10.1007/s00406-017-0828-4
Chan RCK, Xu T, Heinrichs RW, Yu Y, Gong Q (2010) Neurological soft signs in non-psychotic first-degree relatives of patients with schizophrenia: a systematic review and meta-analysis. Neurosci Biobehav Rev 34(6):889–896
Sanders RD, Joo YH, Almasy L, Wood J, Keshavan MS, Pogue-Geile MF, Gur RC, Gur RE, Nimgaonkar VL (2006) Are neurologic examination abnormalities heritable? A preliminary study. Schizophr Res 86(1–3):172–180. https://doi.org/10.1016/j.schres.2006.06.012
Chan RCK, Xie W, Geng FL, Wang Y, Lui SSY, Wang CY, Yu X, Cheung EFC, Rosenthal R (2016) Clinical utility and lifespan profiling of neurological soft signs in schizophrenia spectrum disorders. Schizophr Bull 42(3):560–570. https://doi.org/10.1093/schbul/sbv196
Tamagni C, Studerus E, Gschwandtner U, Aston J, Borgwardt S, Riecher-Rössler A (2013) Are neurological soft signs pre-existing markers in individuals with an at-risk mental state for psychosis? Psychiatry Res 210(2):427–431. https://doi.org/10.1016/j.psychres.2013.06.016
Callaway DA, Perkins DO, Woods SW, Liu L, Addington J (2014) Movement abnormalities predict transitioning to psychosis in individuals at clinical high risk for psychosis. Schizophr Res 159(2–3):263–266. https://doi.org/10.1016/j.schres.2014.09.031
Mittal VA, Walker EF, Bearden CE, Walder D, Trottman H, Daley M, Simone A, Cannon TD (2010) Markers of basal ganglia dysfunction and conversion to psychosis: neurocognitive deficits and dyskinesias in the prodromal period. Biol Psychiatry 68(1):93–99. https://doi.org/10.1016/j.biopsych.2010.01.021
Schiffman J (2017) Motor issues in the clinical high risk phase of psychosis. Schizophr Bull 43(5):937–938. https://doi.org/10.1093/schbul/sbx086
Weinberger DR (1987) Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry 44(7):660–669. https://doi.org/10.1001/archpsyc.1987.01800190080012
Weinberger DR (2017) Future of days past: neurodevelopment and schizophrenia. Schizophr Bull 43(6):1164–1168. https://doi.org/10.1093/schbul/sbx118
Rapoport JL, Giedd JN, Gogtay N (2012) Neurodevelopmental model of schizophrenia: update 2012. Mol Psychiatry 17(12):1228–1238. https://doi.org/10.1038/mp.2012.23
Bang M, Park H-J, Pae C, Park K, Lee E, Lee S-K, An SK (2018) Aberrant cerebro-cerebellar functional connectivity and minimal self-disturbance in individuals at ultra-high risk for psychosis and with first-episode schizophrenia. Schizophr Res 202:138–140. https://doi.org/10.1016/j.schres.2018.06.031
Andreasen NC, Paradiso S, O’Leary DS (1998) Cognitive dysmetria as an integrative theory of schizophrenia: a dysfunction in cortical-cerebellar circuitry? Schizophr Bull 24:203–218. https://doi.org/10.1093/oxfordjournals.schbul.a033321
Thomann PA, Wustenberg T, Dos Santos V, Bachmann S, Essig M, Schroder J (2009) Neurological soft signs and brain morphology in first-episode schizophrenia. Psychol Med 39:371–379
Dazzan P, Morgan KD, Orr KG, Huchinson G, Chitnis X, Suckling J, Fearon P, Salvo J, McGuire PK, Mallett RM, Jones PB, Leff J, Murray RM (2004) The structural brain correlates of neurological soft signs in AESOP first-episode psychoses study. Brain 127:143–153
Kong L, Bachmann S, Thomann PA, Essig M, Schröder J (2012) Neurological soft signs and gray matter changes: a longitudinal analysis in first-episode schizophrenia. Schizophr Res 134(1):27–32. https://doi.org/10.1016/j.schres.2011.09.015
Kong L, Herold CJ, Cheung EFC, Chan RCK, Schröder J (2020) Neurological soft signs and brain network abnormalities in schizophrenia. Schizophr Bull 46(3):562–571. https://doi.org/10.1093/schbul/sbz118
Mittal VA, Dean DJ, Bernard JA, Orr JM, Pelletier-Baldelli A, Carol EE, Gupta T, Turner J, Leopold DR, Robustelli BL (2014) Neurological soft signs predict abnormal cerebellar-thalamic tract development and negative symptoms in adolescents at high risk for psychosis: a longitudinal perspective. Schizophr Bull 40(6):1204–1215. https://doi.org/10.1093/schbul/sbt199
Kong L, Cui H, Zhang T, Wang Y, Huang J, Zhu Y, Tang Y, Herold CJ, Schröder J, Cheung EFC, Chan RCK, Wang J (2019) Neurological soft signs and grey matter abnormalities in individuals with ultra-high risk for psychosis. PsyCh J 8:250–262. https://doi.org/10.1002/pchj.258
Yung AR, McGorry PD, McFarlane CA, Jackson HJ, Patton GC, Rakkar A (1996) Monitoring and care of young people at incipient risk of psychosis. Schizophr Bull 22(2):283–303. https://doi.org/10.1093/schbul/22.2.283
McGorry PD, Goodwin RJ, Stuart GW (1988) The development, use, and reliability of the brief psychiatric rating scale (nursing modification)—an assessment procedure for the nursing team in clinical and research settings. Compr Psychiatry 29(6):575–587. https://doi.org/10.1016/0010-440X(88)90078-8
Yung AR, Pan Yuen H, Mcgorry PD, Phillips LJ, Kelly D, Dell’olio M, Francey SM, Cosgrave EM, Killackey E (2005) Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Aust N Z J Psychiatry 39(11–12):964–971. https://doi.org/10.1080/j.1440-1614.2005.01714.x
American Psychiatric Association (1986) Global assessment of functioning (GAF). Diagnostic and statistical manual of mental disorders-III-R. American Psychiatric Association, Washington DC
Yung AR, Phillips LJ, Yuen HP, Francey SM, McFarlane CA, Hallgren M, McGorry PD (2003) Psychosis prediction: 12-month follow-up of a high-risk (“prodromal”) group. Schizophr Res 60(1):21–32
Nelson B, Yuen HP, Wood SJ, Lin A, Spiliotacopoulos D, Bruxner A, Broussard C, Simmons M, Foley DL, Brewer WJ (2013) Long-term follow-up of a group at ultra high risk (“prodromal”) for psychosis: the PACE 400 study. JAMA Psychiat 70(8):793–802. https://doi.org/10.1001/jamapsychiatry.2013.1270
First MB, Spitzer RL, Gibbon M, Williams JBW (1997) User’s guide for the Structured clinical interview for DSM-IV axis I disorders SCID-I: clinician version. American Psychiatric Publication, Washington
Gaser C, Dahnke R (2016) CAT-a computational anatomy toolbox for the analysis of structural MRI data. HBM 2016:336–348
Ashburner J, Friston KJ (2000) Voxel-based morphometry—the methods. Neuroimage 11(6):805–821. https://doi.org/10.1006/nimg.2000.0582
Winkler AM, Ridgway GR, Webster MA, Smith SM, Nichols TE (2014) Permutation inference for the general linear model. Neuroimage 92:381–397. https://doi.org/10.1016/j.neuroimage.2014.01.060
Schroder J, Niethammer R, Geider FJ, Reitz C, Binkert M, Jauss M, Sauer H (1992) Neurological soft signs in schizophrenia. Schizophr Res 6:25–30
Ruhrmann S, Schultze-Lutter F, Klosterkötter J (2010) Probably at-risk, but certainly ill–advocating the introduction of a psychosis spectrum disorder in DSM-V. Schizophr Res 120(1–3):23–37. https://doi.org/10.1016/j.schres.2010.03.015
Lin A, Wood SJ, Nelson B, Beavan A, McGorry P, Yung AR (2015) Outcomes of nontransitioned cases in a sample at ultra-high risk for psychosis. Am J Psychiatry 172(3):249–258. https://doi.org/10.1176/appi.ajp.2014.13030418
Cropley VL, Lin A, Nelson B, Reniers RLEP, Yung AR, Bartholomeusz CF, Klauser P, Velakoulis D, McGorry P, Wood SJ, Pantelis C (2016) Baseline grey matter volume of non-transitioned “ultra high risk” for psychosis individuals with and without attenuated psychotic symptoms at long-term follow-up. Schizophr Res 173(3):152–158. https://doi.org/10.1016/j.schres.2015.05.014
Addington J, Piskulic D, Liu L, Lockwood J, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Bearden CE, Mathalon DH, Woods SW (2017) Comorbid diagnoses for youth at clinical high risk of psychosis. Schizophr Res 190:90–95. https://doi.org/10.1016/j.schres.2017.03.043
Pantelis C, Yücel M, Wood SJ, Velakoulis D, Sun D, Berger G, Stuart GW, Yung A, Phillips L, McGorry PD (2005) Structural brain imaging evidence for multiple pathological processes at different stages of brain development in schizophrenia. Schizophr Bull 31(3):672–696. https://doi.org/10.1093/schbul/sbi034
Mechelli A, Riecher-Rössler A, Meisenzahl EM, Tognin S, Wood SJ, Borgwardt SJ, Koutsouleris N, Yung AR, Stone JM, Phillips LJ (2011) Neuroanatomical abnormalities that predate the onset of psychosis: a multicenter study. Arch Gen Psychiatry 68(5):489–495. https://doi.org/10.1001/archgenpsychiatry.2011.42
Fusar-Poli P, Radua J, McGuire P, Borgwardt S (2012) Neuroanatomical maps of psychosis onset: voxel-wise meta-analysis of antipsychotic-naive VBM studies. Schizophr Bull 38(6):1297–1307. https://doi.org/10.1093/schbul/sbr134
Pantelis C, Velakoulis D, McGorry PD, Wood SJ, Suckling J, Phillips LJ, Yung AR, Bullmore ET, Brewer W, Soulsby B (2003) Neuroanatomical abnormalities before and after onset of psychosis: a cross-sectional and longitudinal MRI comparison. Lancet 361:281–288
Bartholomeusz CF, Cropley VL, Wannan C, Di Biase M, McGorry PD, Pantelis C (2017) Structural neuroimaging across early-stage psychosis: Aberrations in neurobiological trajectories and implications for the staging model. Aust N Z J Psychiatry 51(5):455–476. https://doi.org/10.1177/0004867416670522
Takahashi T, Wood SJ, Yung AR, Walterfang M, Phillips LJ, Soulsby B, Kawasaki Y, McGorry PD, Suzuki M, Velakoulis D (2010) Superior temporal gyrus volume in antipsychotic-naive people at risk of psychosis. Br J Psychiatry 196(3):206–211. https://doi.org/10.1192/bjp.bp.109.069732
Wood SJ, Kennedy D, Phillips LJ, Seal ML, Yücel M, Nelson B, Yung AR, Jackson G, McGorry PD, Velakoulis D (2010) Hippocampal pathology in individuals at ultra-high risk for psychosis: a multi-modal magnetic resonance study. Neuroimage 52(1):62–68. https://doi.org/10.1016/j.neuroimage.2010.04.012
Zhao Q, Li Z, Huang J, Yan C, Dazzan P, Pantelis C, Cheung EFC, Lui SSY, Chan RCK (2014) Neurological soft signs are not “soft” in brain structure and functional networks: evidence from ALE meta-analysis. Schizophr Bull 40(3):626–641. https://doi.org/10.1093/schbul/sbt063
Hirjak D, Kubera KM, Wolf RC, Thomann AK, Hell SK, Seidl U, Thomann PA (2015) Local brain gyrification as a marker of neurological soft signs in schizophrenia. Behav Brain Res 292:19–25. https://doi.org/10.1016/j.bbr.2015.05.048
Bachmann S, Schröder J (2018) Neurological soft signs in schizophrenia: an update on the state-versus trait-perspective. Front Psych 8:272. https://doi.org/10.3389/fpsyt.2017.00272
Bottmer C, Bachmann S, Pantel J, Essig M, Amann M, Schad LR, Magnotta V, Schröder J (2005) Reduced cerebellar volume and neurological soft signs in first-episode schizophrenia. Psychiatry Res Neuroimaging 140(3):239–250
Keshavan MS, Sanders RD, Sweeney JA, Diwadkar VA, Goldstein G, Pettegrew JW, Schooler NR (2003) Diagnostic specificity and neuroanatomical validity of neurological abnormalities in first-episode psychoses. Am J Psychiatry 160(7):1298–1304. https://doi.org/10.1176/appi.ajp.160.7.1298
Mouchet-Mages S, Canceil O, Willard D, Krebs M-O, Cachia A, Martinot J-L, Rodrigo S, Oppenheim C, Meder J-F (2007) Sensory dysfunction is correlated to cerebellar volume reduction in early schizophrenia. Schizophr Res 91(1–3):266–269. https://doi.org/10.1016/j.schres.2006.11.031
Herold CJ, Essig M, Schröder J (2020) Neurological soft signs (NSS) and brain morphology in patients with chronic schizophrenia and healthy controls. PLoS ONE 15(4):e0231669. https://doi.org/10.1371/journal.pone.0231669
Fusar-Poli P, Salazar de Pablo G, Correll CU, Meyer-Lindenberg A, Millan MJ, Borgwardt S, Galderisi S, Bechdolf A, Pfennig A, Kessing LV, van Amelsvoort T, Nieman DH, Domschke K, Krebs M-O, Koutsouleris N, McGuire P, Do KQ, Arango C (2020) Prevention of psychosis: advances in detection, prognosis, and intervention. JAMA Psychiat 77(7):755–765. https://doi.org/10.1001/jamapsychiatry.2019.4779
Nelson B, Yuen HP, Lin A, Wood SJ, McGorry PD, Hartmann JA, Yung AR (2016) Further examination of the reducing transition rate in ultra high risk for psychosis samples: the possible role of earlier intervention. Schizophr Res 174(1–3):43–49. https://doi.org/10.1016/j.schres.2016.04.040
Formica MJC, Phillips LJ, Hartmann JA, Yung AR, Wood SJ, Lin A, Amminger GP, McGorry PD, Nelson B (2020) Has improved treatment contributed to the declining rate of transition to psychosis in ultra-high-risk cohorts? Schizophr Res. https://doi.org/10.1016/j.schres.2020.04.028
Yung AR, Yuen HP, Berger G, Francey S, Hung TC, Nelson B, Phillips L, McGorry P (2007) Declining transition rate in ultra high risk (prodromal) services: dilution or reduction of risk? Schizophr Bull 33(3):673–681. https://doi.org/10.1093/schbul/sbm015
Hartmann JA, Yuen HP, McGorry PD, Yung AR, Lin A, Wood SJ, Lavoie S, Nelson B (2016) Declining transition rates to psychotic disorder in “ultra-high risk” clients: investigation of a dilution effect. Schizophr Res 170(1):130–136. https://doi.org/10.1016/j.schres.2015.11.026
Funding
This research was supported by project grants (IDs: 970598 and 981112) and Program Grant (ID: 350241) from the National Health and Medical Research Council (NHMRC), Australia; the Ian Potter Foundation, Melbourne; Woods Family Trust, Melbourne; a Program Grant from the Victorian Health Promotion Foundation, Melbourne. C Pantelis was supported by NHMRC Senior Principal Research Fellowships (628386 and 1105825), and a Brain and Behavior Research Foundation (NARSAD) Distinguished Investigator Award (US; Grant ID: 18722). PD McGorry was supported by a NHMRC Senior Principal Research Fellowship, and a Brain and Behavior Research Foundation (NARSAD) Distinguished Investigator Award (US). AR Yung was supported by a NHMRC Principal Research Fellowship (1136829) and a National Institute of Health Research (NIHR) Senior Fellowship Award. Y Wang was supported by the China Scholarship Council. T Van Rheenen was supported by an NHMRC Early Career Fellowship (1088785). B Nelson was supported by an NHMRC Senior Research Fellowship (1137687). A Lin is supported by an NHMRC Career Development Fellowship (1148793). VL Cropley was supported by a NHMRC Investigator Grant (1177370), a Brain and Behavior Research Foundation (NARSAD) Young Investigator Award (21660), and a University of Melbourne Dame Kate Campbell Fellowship. Raymond Chan was supported by the National Key Research and Development Programme (2016YFC0906402).
Author information
Authors and Affiliations
Contributions
VLC and CP designed the study. DV, BN, PM, AY, AL, WB, JK, SW and CP were responsible for participant recruitment and assessment. YW, EB and VLC performed statistical analysis. All authors reviewed data analysis and data interpretation. YW and EB wrote the first draft, which was critically reviewed by VLC. All authors contributed to the review of and critical input to the manuscript and have approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declares that they have no competing interest.
Ethics approval
The local research and ethics committee in Melbourne, Australia, approved the study.
Consent to participate
Informed consent was provided by all participants.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, Y., Braam, E.E., Wannan, C.M.J. et al. Investigation of structural brain correlates of neurological soft signs in individuals at ultra-high risk for psychosis. Eur Arch Psychiatry Clin Neurosci 271, 1475–1485 (2021). https://doi.org/10.1007/s00406-021-01300-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-021-01300-9