Abstract
Post-acute sequelae of COVID-19 can present as multi-organ pathology, with neuropsychiatric symptoms being the most common symptom complex, characterizing long COVID as a syndrome with a significant disease burden for affected individuals. Several typical symptoms of long COVID, such as fatigue, depressive symptoms and cognitive impairment, are also key features of other psychiatric disorders such as myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and major depressive disorder (MDD). However, clinically successful treatment strategies are still lacking and are often inspired by treatment options for diseases with similar clinical presentations, such as ME/CFS. Acetylcarnitine, the shortest metabolite of a class of fatty acid metabolites called acylcarnitines and one of the most abundant blood metabolites in humans can be used as a dietary/nutritional supplement with proven clinical efficacy in the treatment of MDD, ME/CFS and other neuropsychiatric disorders. Basic research in recent decades has established acylcarnitines in general, and acetylcarnitine in particular, as important regulators and indicators of mitochondrial function and other physiological processes such as neuroinflammation and energy production pathways. In this review, we will compare the clinical basis of neuropsychiatric long COVID with other fatigue-associated diseases. We will also review common molecular disease mechanisms associated with altered acetylcarnitine metabolism and the potential of acetylcarnitine to interfere with these as a therapeutic agent. Finally, we will review the current evidence for acetylcarnitine as a supplement in the treatment of fatigue-associated diseases and propose future research strategies to investigate the potential of acetylcarnitine as a treatment option for long COVID.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19) is associated with neuropsychiatric symptoms both during the acute SARS-CoV-2 infection as well as within weeks to months after recovery from the acute disease episode, termed post-acute sequelae of SARS-CoV-2 infection (PASC) [23]. PASC that persist for more than 4 weeks after the acute infection are termed “long COVID” [12, 26, 31], with varying incidences between 10 and 70% of infected COVID-19 patients developing long COVID symptoms, depending on the study population examined, e.g., non-hospitalized, hospitalized or vaccinated patients, etc. [31]. Long COVID is a multi-system disease affecting heart, lungs, gastrointestinal tract, kidneys, spleen and the liver, as reviewed in detail elsewhere [6, 26, 31]. However, neuropsychiatric symptoms developing on the basis of direct brain tissue pathology or underlying vascular dysfunction are considered to be a major and the most common feature of long COVID [4, 7, 31, 37, 65, 88, 113], with potentially devastating consequences for affected individuals. In particular, fatigue with post-exertional malaise, cognitive impairment characterized by deficits in executive functions, concentration and memory and depressed mood [88] are the main features of neuropsychiatric long COVID syndrome [31], with fatigue being the most common and debilitating [99].
It is interesting to note that other post-acute infection syndromes (PAIS) and some neuropsychiatric diseases such as myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), depression (especially the atypical/immunometabolic subtype (IMD) [86]) and others also have fatigue as a leading clinical symptom, which may serve as a model for investigating the mechanisms of fatigue and drawing conclusions regarding therapeutic options in long COVID. Indeed, most treatment options for long COVID, which focus on modulating neuroinflammation, vascular defects and energy metabolism alterations due to mitochondrial dysfunction, have been inspired by treatment approaches for PAIS and ME/CFS [31].
Acetylcarnitine belongs to a class of fatty acid metabolites called acylcarnitines, which are produced by the conjugation of fatty acids with l-carnitine, a physiological process essential for the transport of fatty acids into mitochondria for β-oxidation and ATP production [3, 29]. Interestingly, evidence from metabolomic studies has shown associations between abnormal acylcarnitine and acetylcarnitine levels in several of the aforementioned fatigue-associated neuropsychiatric diseases, as reviewed elsewhere [29]. Short-chain acylcarnitines, i.e., acylcarnitines with two to five carbon atoms, are the most abundant acylcarnitines in human plasma, with acetylcarnitine being the major acylcarnitine [29]. Consequently, acetylcarnitine supplementation has been shown to improve fatigue, depressive symptoms and cognitive dysfunction for example, by modulating mitochondrial metabolism and neuroinflammation in the aforementioned diseases [29]. Furthermore, acetylcarnitine supplementation has recently been proposed for the treatment of neuropsychiatric long COVID symptoms [115].
The aims of this review are (1) to provide an overview of the clinical and biological overlap between neuropsychiatric long COVID and other fatigue-associated neuropsychiatric disorders, (2) to examine the shared molecular mechanisms of fatigue and depressive symptoms involving acetylcarnitine metabolism, and finally (3) to review the current evidence on acetylcarnitine supplementation studies as a treatment for fatigue-associated syndromes and pharmacological aspects of acetylcarnitine supplementation to provide a conceptual foundation for acetylcarnitine supplementation in neuropsychiatric long COVID syndrome.
Main part
Similarities in clinical presentation of long COVID and post-acute infection syndromes as well as major depressive disorder with atypical features
Already in 2020 the first long COVID patients approached medical professionals from different disciplines [68]. At that time, physicians were often reluctant to diagnose this multifaceted clinical syndrome as long COVID because routine diagnostics of blood samples or imaging in survivors of mild acute COVID-19 rarely yielded any pathological results [120]. However, the diagnosis and treatment of patients with long COVID to date has made it very clear that the majority of patients experience a multi-system syndrome characterized by fatigue with post-exertional malaise, cognitive deficits, depressed mood, stress-related head and joint pain, insomnia and vegetative dysfunction [99]. So far, there is an alarming number of long COVID patients who do not recover after several months and even a subgroup with worsening symptoms over time [36, 126]. However, long COVID is only one of several post-acute infection syndromes (PAIS) that have been reported, not only after previous coronavirus epidemics (e.g., SARS-CoV-1 and MERS-CoV) but also after other systemic viral, bacterial and parasitic infections, as reviewed in [23]. According to their review, the clinical characteristics of other PAIS appear almost indistinguishable from long COVID as described above, including exertion intolerance, fatigue, neurocognitive and sensory impairment, sleep disturbances, joint and muscle pain, and non-specific symptoms that are often present but of variable severity.
Many of these PAIS patients, as well as PASC patients, even meet the criteria for ME/CFS after months of incomplete recovery, as has been impressively demonstrated in large registry studies after infections with H1N1/09 influenza A virus and varicella zoster virus [78, 139]. The significant clinical overlap between ME/CFS and PASC has very recently been reviewed here [82], with the hypothesis that both entities may be caused by a chronic state of multisystemic disequilibrium, including endocrinological, immunological, and/or metabolic changes.
ME/CFS is a frequent syndrome affecting 0.9% of the population [71]. It is diagnosed according to the Canadian consensus criteria, at least 6 months after onset when the following symptoms are present: fatigue, post-exertional malaise with a recovery period of at least 24 h, sleep dysfunction, pain, at least two neurological/neurocognitive symptoms and at least two symptoms involving the autonomic, neuroendocrine or immune system [19]. The underlying pathophysiology is mostly unresolved, with immunological factors often, but not exclusively, occurring after an initial infection with a distinct or gradual onset. Other putative origins investigated in large, population-based datasets include chronic autoimmune syndromes such as inflammatory bowel disease and psoriasis [136, 137], and even after thermal injury, especially in extensive injuries and on sun-exposed body parts [138].
To understand the biological overlap and therefore possible therapeutic targets for PAIS such as PASC, it is also interesting to note similar clinical features in a typical major depressive disorder, (MDD) also known as immunometabolic depression [86]. This syndrome is characterized by clinical symptoms of sickness behavior such as leaden paralysis of the limbs, hypersomnia, and hyperphagia/weight gain, while mood reactivity is unimpaired, i.e., mood brightens in response to positive events (according to DSM-5 criteria for MDD with atypical features), while still suffering from lack of concentration and higher levels of exhaustibility as in melancholic MDD [99]. Van Hoof et al. even reviewed clinical observations of behavioral, affective and cognitive features already 20 years ago and hypothesized that atypical depression is a secondary symptom in chronic fatigue syndrome [140].
Considering the clinical overlap of these multisystemic clinical syndromes, we will now proceed to summarize aspects of common biomarkers and pathological mechanisms underlying these shared symptoms.
Shared pathomechanisms of neuropsychiatric syndromes with fatigue as a leading symptom (PASC, PAIS, ME/CFS, IMD)
Alterations of brain structure and connectivity
PASC is currently being investigated by neuroimaging experts all over the world. To date, structural imaging studies have reported inconsistent results, probably depending on the age of the participants, the severity of acute COVID-19 and the symptom burden at the time of scanning. The most consistent results so far are grey matter alterations in the basal ganglia, areas of the limbic system such as the anterior cingulate cortex, hippocampus, insula, etc., and prefrontal areas like the orbitofrontal cortex, sometimes even more pronounced in association with self-reported fatigue or neurocognitive impairment [12, 35, 49]. A recent longitudinal imaging study showed a reduction of thalamus and basal ganglia volumes as well as aberrant diffusion markers in post-COVID patients, which correlated with fatigue scores [50]. Regarding functional connectivity, several exploratory studies have confirmed a pattern of increased and/or decreased connectivity in frontotemporal networks associated with subjective cognitive impairment and olfactory dysfunction [98, 148, 152]. As demonstrated by [18F]FDG-PET/CT ([18F]Fluorodeoxyglucose positron emission tomography/computed tomography), patients suffering from long COVID also showed brain glucose hypometabolism in the right parahippocampal gyrus and thalamus, while specific hypometabolic area(s) characterized patients with persistent anosmia/ageusia, fatigue, and vascular uptake [119]. The brainstem, which has been implicated to be affected in PASC, explaining the broad spectrum of symptoms, particularly pain and autonomic symptoms [156], has been found to show glucose hypometabolism in patients (among other regions) [47, 53, 89]. Although technically challenging, this should be further investigated, especially in light of the neuroimaging findings in ME/CFS, described in the following paragraphs.
While there is no evidence of common structural or functional brain alterations in PAIS, probably due to its heterogeneous origin and lack of conceptualization, ME/CFS has been extensively studied with MRI (magnetic resonance imaging), as recently reviewed by Nelson et al. [94]. Although the findings are not always consistent, changes in the brainstem have been very common, especially structural changes, mainly a decrease in grey or white matter volume in patients, often pronounced in relation to the symptom burden of fatigue, pain and autonomic symptoms. One diffusion-tensor imaging study even showed decreased diffusivity in the brainstem and basal ganglia area in ME/CFS patients [129]. In addition, altered functional connectivity has also been reported in the brainstem, basal ganglia and related areas such as the limbic system [123]. Neuroinflammation, vascular dysfunction, and cellular dysfunction regarding astrocytes and neurons have been discussed as underlying mechanisms contributing to these structural and functional alterations [94]. Furthermore, ME/CFS patients showed glucose hypometabolism in the brainstem as well as in the right mediofrontal cortex, similar to findings in long COVID patients [130].
Neuroinflammation
Neuroinflammation is increasingly recognized as a key factor interacting with neurobiological correlates of the neuropsychiatric long COVID syndrome, such as brain serotonin depletion [111], hypothalamic–pituitary–adrenal (HPA) axis dysregulation [57], and impaired hippocampal neurogenesis and plasticity [13, 61].
The central nervous system (CNS) relies on a complex and intricate network of molecular and cellular interactions to maintain proper function and homeostasis. The initial SARS-CoV-2 viral infection triggers an immune response that may persist in some individuals even after the virus has been cleared, leading to ongoing hyper-inflammation. There is increasing evidence that neuroinflammation is an important component of ME/CFS [34] and probably also of long COVID [127]. Commonly suggested biomedical hypotheses to explain PAIS (such as in long COVID/PASC, ME/CFS) are chronic stimulation of the immune system by a persistent infection or persistent unviable pathogen structures; immune activation with targeting self-antigens, either due to infection-triggered impairment of regulatory T-cell function, molecular mimicry, dysregulation of the microbiota–gut–brain axis, as well as permanent organ damage [104]. The immune response to SARS-CoV-2 in the respiratory tract has been shown to induce neuroinflammation, which subsequently leads to an acute inflammatory response and immune cell trafficking in the brain, and induces reactive states of resident microglia and other immune cells in the brain and brain borders [44, 51, 154]. These processes may exist in combination and at different intensities in different patient subgroups. However, neuroinflammation and the consequent dysregulation of neural homeostasis and plasticity is likely to be a more common mechanistic principle, occurring even after mild COVID-19 disease [141]. Of note, neuroinflammation has furthermore been implicated in the pathophysiology of depression [87], whereas increased inflammatory markers, such as C-reactive protein (CRP) or interleukin-2 (IL-2), have been specifically described to be more associated with the atypical subtype of depression [69].
Perturbations in mitochondrial dynamics can affect many cellular and molecular pathways, particularly during inflammation [15] (for reviews, see [33, 116]). Inflammation stimulates the production of reactive oxygen species (ROS), which can further damage mitochondria and impair their function [103]. In addition, inflammation can alter the expression of genes involved in mitochondrial function, leading to changes in energy metabolism. Associations between mitochondrial genetic variation, activation of the immune system, and its effects on neurogenesis and neurotransmission have led some authors to suggest that mitochondrial dysfunction initiates a chain of molecular events leading to key symptoms of neuropsychiatric long COVID, such as depressive mood and cognitive impairment [39, 100, 135].
Of note, there are at least five other mechanisms besides secondary neuroinflammation by which COVID can affect the CNS (direct viral invasion of neural tissue, autoimmunity, reactivation of herpesviruses, neurovascular dysfunction, the sequelae of hypoxic, and other metabolic disturbances), which may occur exclusively or in combination in some individuals with varying frequency and timing (for review, see [88]).
Preclinical studies suggest that acetylcarnitine attenuates oxidative stress and neuroinflammation [2, 112]. Mechanisms that could potentially link acetylcarnitine to inflammatory pathways and synaptic activity include changes in monoaminergic and glutamatergic transmission. Such changes are commonly observed in neuropsychiatric disorders (for a review of these changes, see [153]). In brief, indoleamine 2,3-dioxygenase (IDO) activity is increased during inflammation, leading to increased conversion of tryptophan to kynurenine, reducing substrate availability for serotonin synthesis. Kynurenine is predominantly metabolized to the N-methyl-d-aspartate (NMDA) receptor agonist quinolinic acid (QUIN) in the inflammatory state, contributing to the accumulation of glutamate in the extracellular space, leading to changes in network connectivity associated with depression, fatigue and cognitive impairment. Acetylcarnitine, on the other hand, affects the epigenetic regulation of metabotropic glutamate type 2 receptors (mGluR2), negatively modulating neurotransmitter release and producing rapid and long-lasting antidepressant effects (demonstrated by forced swim tests, sucrose preference tests) in Flinders Sensitive Line rats and in mice exposed to chronic unpredictable stress, which model genetic and environmentally induced depression, respectively [92]. Using nuclear magnetic resonance (NMR) spectroscopy, Smeland and colleagues also demonstrated increased levels of norepinephrine and serotonin in the cortex of healthy mice, after 25 days of treatment with acetylcarnitine at a daily dose of approximately 0.5 g/kg body weight [117]. In addition, a non-enzymatic product of the prostaglandin D2 synthase gene (PGD2S), whose expression is upregulated by acetylcarnitine treatment with 100 mg/kg body weight [134], has been shown to have anti-inflammatory properties that may help protect the brain from ischemia–reperfusion injury [72].
Taken together, these findings suggest that acetylcarnitine supplementation may attenuate the inflammatory damage that contributes to neuropsychiatric long COVID syndrome.
Systemic metabolic alterations and their relationship to neuropsychiatric symptomatology
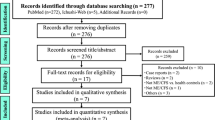
PAIS, including long COVID, as well as CFS and IMD, share the characteristic of systemic metabolic disturbances, which may be a sign of underlying multi-organ inflammation and exhaustion [31], and consequently may contribute to neuropsychiatric symptomatology, as many metabolites can cross the blood–brain barrier (BBB) [30, 58] (e.g., short chain fatty acids (SCFAs) derived from the gut microbiota such as acetate [40], amino acids such as tryptophan [52] and also carnitine/acetylcarnitine can cross the BBB via transporters [59]). A large number of studies have investigated peripheral metabolomic changes in the aforementioned conditions, with considerable overlap between PAIS, CFS, and immunometabolic depression: As reviewed by Komaroff et al., the systemic metabolomic changes in ME/CFS patients are characterized by (1) an impairment in the production of ATP from all energy substrates, (2) a general “hypometabolic state” and (3) an imbalance between pro- and antioxidant metabolites favouring pro-oxidant processes [43, 62]. This metabolic dysregulation is defined by systemically reduced levels of metabolites such as amino acids and fatty acids, leading to reduced TCA cycle activity and oxidative phosphorylation, which may ultimately be a major contributor to neuropsychiatric symptoms associated with reduced energy, such as fatigue and other cognitive impairments [43, 62]. Interestingly, such signs of mitochondrial dysfunction have also been described in MDD and long COVID: de Boer et al. found that during exercise, patients with long COVID showed decreased rates of fatty acid oxidation [32], consistent with other reports [48] that describe a general metabolic profile of impaired mitochondrial fatty acid and lipid catabolism in general, as well as a decrease in several amino acids that can fuel mitochondrial TCA cycle activity. These findings have also been described for MDD, e.g., in a large meta-analysis by Bot and Milaneschi et al., which found an association between depression risk and different lipid classes [14] and in several other studies, as reviewed in detail by Guerreiro Costa et al. [74]. In addition to these general metabolic changes linking impaired energy production to fatigue as a common symptom between long COVID, ME/CFS and MDD, common differences in specific metabolites may also be of importance. Tryptophan (Trp) metabolism, and consequently Trp-derived metabolite pathways such as the kynurenine and serotonin pathways, have long been known to be central to the pathophysiology of MDD—lower blood concentrations of Trp have been described in several studies of MDD patients, and alterations in tryptophan and kynurenine levels have also been associated with symptomatology and treatment [24, 74]. In addition, the ratio of neuroprotective to neurotoxic kynurenine metabolites differs between healthy controls and ME/CFS patients [46], accompanied and probably often preceded by a general decrease in tryptophan [25, 74]. The direct relationship between tryptophan levels and depressive symptoms and fatigue has been demonstrated by Trp depletion experiments, as reviewed elsewhere [76], and is also of interest in the context of long-term COVID, as recent studies have shown a significant decrease in plasma Trp levels in PASC patients [48], and alterations in kynurenine pathway metabolites have been associated with cognitive impairment in long COVID patients [27], as well as with anxiety and depressive symptoms in COVID-19 survivors 6 months post-infection [66]. In addition to the aforementioned remodelling of the metabolome in fatigue-associated diseases, including long COVID, acylcarnitines have emerged as important modulators of CNS function [29]: In both mice and humans, different classes of acylcarnitines have been found to be altered in either mouse models of depression or humans with MDD, with associations to symptom severity and also treatment response, as reviewed by Liu et al. [73]. In particular, short-chain acylcarnitines, such as acetylcarnitine, which are thought to rather support neuronal function [29], were decreased in the plasma of MDD patients, and more harmful medium- and long-chain acylcarnitines were increased in several studies [73]. Interestingly, similar patterns have also been observed in ME/CFS [91] and long Covid patients [48]. Guntur et al. found that in a small cohort of PASC patients, increases in medium- and long-chain acylcarnitines were among the most pronounced changes in a plasma metabolomic experiment between healthy controls and patients with PASC [48]. However, short-chain acylcarnitines were not altered in this study, which may be explained by the relatively small patient cohort (29 PASC patients, 30 healthy controls) [48]. In contrast to this result, another recent study by Kovarik et al. found a significant decrease in C3-carnitine in patients with long COVID, although the cohort sizes in this study were also relatively small (13 healthy controls and 13 patients with long COVID) [63]. Therefore, we obtained the data from the—to our knowledge—largest plasma metabolomics study conducted to date in long COVID patients by Su et al. [124] (Table S2 from Su et al., sheet “S2.2 Metabolomics”, age-, sex- and BMI-adjusted z-score-transformed plasma metabolite concentrations) and re-analysed the plasma metabolomics data for acetylcarnitine to investigate differences in acetylcarnitine levels between healthy controls and patients with PASC (≥ 1 PASC symptom according to the clinical information available from Table S1, sheet “S1.3 PASC data” of Su et al.). Indeed, we observed a decrease in plasma acetylcarnitine levels in PASC patients (Fig. 1), which is consistent with previously reported decreases in acetylcarnitine in other fatigue-associated conditions and supports our hypothesis that acetylcarnitine supplementation may be beneficial in the treatment of long COVID-associated neuropsychiatric symptoms. Taken together, metabolomic studies of long COVID, ME/CFS, and MDD show considerable similarities in the overall metabolic profiles associated with a disruption of energy production and an imbalance of potentially neuroprotective and detrimental metabolites, i.e., a deficiency of neuroprotective metabolites such as acetylcarnitine.
Metabolomic data from Su et al. [124] were retrieved from the provided Supplementary Data Set S2 (sheet “S2.2 Metabolomics”), as well as clinical data on PASC (post-acute sequelae of SARS-CoV-2 infection) symptoms (Table S1) from the INCOV cohort. Subsequently, z-score transformed metabolite concentrations for acetylcarnitine (C2) were extracted for healthy controls (n = 178) and all INCOV patients with ≥ 1 PASC symptom (n = 68), representing the PASC cohort. Shown are z-score transformed metabolite concentrations at T3, a time point 2–3 months after initial infection. p value represents the exact p value from a two-tailed Mann–Whitney test as the z-score transformed data were not normally distributed, calculated using GraphPad Prism 8.4.3. Violin plots show the median (bold black line) and quartiles (faint black lines)
Mitochondrial dysfunction in post-infectious fatigue
The SARS-CoV-2 virus primarily damages lung cells, thus affecting the respiratory system and causing acute respiratory distress, resulting in low blood and tissue oxygen levels. The pathways associated with hypoxia and dysregulated immune system have been identified as strong drivers of neurological complications of post-acute sequelae of SARS-CoV-2 infection (evidence from the post-mortem brain studies and observational studies) [97]. Global hypoxia affects the electron transport chain, fatty acid beta-oxidation and other metabolic pathways essential for mitochondrial energy production. Reduced ATP production and impaired mitochondrial function were observed not only in the lungs, but also in the heart and other tissues. In addition, COVID-19’s effects on the cardiovascular system reduce the availability of oxygen and nutrients throughout the body, depleting energy stores and causing energy deficency. Inefficient metabolism has been shown to lead to the accumulation of metabolic intermediates that can interfere with mitochondrial function and impair the ability to produce ATP. Several metabolic intermediates, such as long-chain acylcarnitines can cause oxidative stress at high levels and high levels of ROS can then cause damage to cells and tissues, leading to a further decline in performance. Overall, the biochemical mechanisms of COVID-19-induced tissue damage are complex and involve a range of metabolism-disturbing processes, including inflammation, hypoxia, energy deficiency, and accumulation of metabolic intermediates [45]. Accordingly, tissue damage of varying severity results in long recovery times after the acute phase of COVID-19 infection.
COVID-19 has now been classified as an endemic disease, but the consequences of COVID-19 infection manifest as long-term multiorgan dysfunction. Most attention is being paid to critical perturbations of the cardiovascular system, where the underlying mechanisms of post-COVID-19 cardiovascular dysfunction are associated with cardiac mitochondrial dysfunction [21]. Another syndrome is post-COVID-19 sarcopenia, characterized by loss of muscle mass and function [102], leading to exercise intolerance [8, 32]. The hyper-inflammatory response caused by SARS-CoV-2 induces the process of immunosenescence, increases endothelial cell damage, and leads to myofibrillar degradation and muscle wasting (sarcopenia) due to mitochondrial dysfunction and autophagy [102]. Persistent viral infection and inflammation may cause sleep disturbances observed 3 months after COVID-19, which may also be associated with mitochondrial dysfunction [128]. Several studies suggest that inflammation may contribute to depression by affecting the function of neuronal mitochondria in the brain [20]. Improving mitochondrial function has been shown to accelerate the resolution of post-COVID-19 symptoms [42, 125]. Overall, mitochondrial dysfunction may play a role in post-COVID-19 syndrome, and more research is needed to fully understand the underlying mechanisms and develop effective treatments, which is why we will elaborate further on acetylcarnitine metabolism in vivo and as a supplement.
Acetylcarnitine metabolism in the context of post-infectious and/or inflammation-associated neuropsychiatric diseases
Biosynthesis and regulation of acetylcarnitine
In the cell, acetylcarnitine is produced by conjugation of the acetyl group of acetyl-CoA with l-carnitine. The reaction is catalyzed by the carnitine acetyltransferase (CrAT, EC:2.3.1.7), which is present in many cell compartments, including the cytosol, the matrix or mitochondria and peroxisomes, as well as the endoplasmic reticulum and nucleus [5, 83, 106]. Carnitine for this reaction can be biosynthesized or obtained from dietary sources and further transported via the organic cation novel type 2 transporter (OCTN2) [75, 107, 122]. CrAT belongs to the family of carnitine acyltransferases, which ensures the transfer of different chain acyl groups to carnitine (Fig. 2). All acyltransferases carry out the bidirectional transfer of acyl groups between CoA and carnitine. CrAT is mainly capable of synthesizing short-chain acylcarnitines with up to five carbons in the acyl group. A less efficient reaction is possible for longer acyl groups with fatty acid chains of up to ten carbon atoms in length [144]. Peroxisomes metabolize a variety of fatty acids, acting as a chain-shortening β-oxidation system that produces large amounts of acetyl-CoA. As CrAT is present in the peroxisomes, peroxisomal CrAT converts a substantial amount of acetyl-CoA to acetylcarnitine [149]. In the cytosol, the reverse activity of CrAT could generate acetyl-CoA that is provided for a variety of biochemical reactions, such as the biosynthesis of malonyl-CoA, acetylcholine, and fatty acids [5].
Synthesis and metabolism of acetylcarnitine. This figure is reproduced in part in a modified form under a CC BY-NC Attribution 4.0 International license from Dambrova et al. [29]
In functional mitochondria, the supply of energy substrates is coupled with oxidative phosphorylation, which ensures a complete metabolic pathway for the generation of ATP. Thus, it can be estimated that only a small part of acetylcarnitine leaves the mitochondria and most of the available acetylcarnitine pool is generated in peroxisomes as a result of fatty acid breakdown. Unlike mitochondria, peroxisomes cannot further metabolize acetylcarnitine and therefore peroxisomes are a major source of acyl groups in the form of acetate and acetylcarnitine. In the bloodstream, acetylcarnitine concentrations are different in fed and fasted states, and accordingly acetylcarnitine availability is related to fatty acid load and metabolic rate, which is much higher in the fasted state. Furthermore, given that glucose and lactate metabolism in mitochondria is fairly complete, these energy substrates do not contribute to the available acetylcarnitine pool.
CrAT can perform reactions in both directions, therefore its activity depends on the acetyl-CoA/free CoA ratio and the availability of carnitine. For example, in mitochondria, when the rate of acetyl group production exceeds the capacity of the Krebs cycle, CrAT activity is shifted to the production of acetylcarnitine to prevent depletion of the free CoA pool [151]. Such overproduction is observed during intensive physical exercise in muscle tissue and during ischemia in the heart [121]. The limited availability of free CoA leads to the arrest of the beta-oxidation process and to the accumulation of harmful long-chain acyl–CoA and acylcarnitines in the mitochondria. Therefore, the CrAT mechanism, which ensures a shift towards the production of acetylcarnitine, is considered beneficial.
Shifting CrAT activity towards the production of acetylcarnitine may rescue beta-oxidation by increasing free CoA, but it only partially solves problems of energy deficiency because the acetyl groups do not enter the Krebs cycle for energy production, but rather escape from the mitochondria in the form of acetylcarnitine. The only benefit may be the possibility of pyruvate decarboxylation by the pyruvate dehydrogenase complex (PDC) [96], which produces the equimolar amount of NADH. However, this process may be limited as PDC activity is significantly reduced in the presence of excess acetyl groups. In addition, CrAT activity is shifted towards the production of acetylcarnitine, leading to a depletion of the intramitochondrial free carnitine pool. Carnitine is required for the transport of long-chain acylcarnitines into the mitochondrial matrix, otherwise they accumulate in the mitochondrial intermembrane space and induce detrimental effects on both mitochondrial respiration and pyruvate metabolism. Accordingly, acute carnitine deficiency induced by excessive conversion of free carnitine to acetylcarnitine could lead to detrimental changes in mitochondrial functionality during ischemia and intensive exercise.
Acetylcarnitine levels under physiological and pathological conditions
Several studies have shown that long-term use of acetylcarnitine reduces symptoms of chronic fatigue and improves the general condition in patients with chronic fatigue syndrome (Table 1, [79, 81, 142]). Similarly, acetylcarnitine therapy has been shown to improve the general condition in the post-COVID-19 period (Table 1) [115]. However, studies that have measured acetylcarnitine levels in patients with chronic fatigue syndrome or in the post-COVID-19 period have found no differences in blood acetylcarnitine levels compared with healthy subjects [22, 48, 55, 118]. On the other hand, some studies have shown that acetylcarnitine concentrations are significantly increased in patients with heart failure and in non-surviving patients after sepsis (Table 1) [38, 157].
Acetylcarnitine supplementation: pharmacodynamics, pharmacokinetics, and clinical efficacy in neuropsychiatric diseases
Acetylcarnitine uptake from exogenous sources (e.g., food)
The oral bioavailability of acetylcarnitine, similar to that of carnitine, is relatively low, with some studies reporting absorption rates as low as 5–10% of approximately 2000 mg, which is considered a saturating dose [107, 108]. The relative bioavailability of higher doses has been reported to be even lower [108]. Moreover, acetylcarnitine is rapidly metabolized in the gut by microbiota to trimethylamine, which is further metabolized in the liver to trimethylamine N-oxide, a biomarker of cardiometabolic risk [28]. A considerable amount of research has been dedicated to the various disorders associated with disturbed carnitine and acetylcarnitine homeostasis, but the pharmacokinetics of acetylcarnitine have mostly been studied in healthy subjects and very few studies report carnitine pharmacokinetics in patient groups, most of which are dedicated to studies in hemodialysis patients [108].
Like other acylcarnitines, acetylcarnitine serves as a transport form for acyl groups, allowing them to cross different membranes with the assistance of various transporters (Fig. 3). OCTN2 (SLC22A5, Organic Cation Transporter Novel 2) is not only known as a main transporter of carnitine but also recognized as an efficient transporter of acetylcarnitine [155]. OCTN2 is localized on various cell membranes and can transport acetylcarnitine into cells as well as ensure acetylcarnitine uptake from the gut and across the blood–brain barrier (BBB) [59]. OCTN2 is differentially expressed in various tissues and plays a major role in regulating carnitine levels within these tissues. OCTN2 is primarily expressed in tissues with high energy demands such as heart, skeletal muscle, liver and kidney. In these tissues, OCTN2 regulates the uptake of carnitine and acetylcarnitine from the blood. OCTN2 is expressed at lower levels in the brain compared to other tissues, therefore the amount of acetylcarnitine transported into the brain would be less active than in other cells [16, 54, 67]. OCTN2 activity can be modulated in response to various physiological and pathological conditions such as exercise, fasting, and metabolic disorders. In addition to OCTN2, organic cation transporter 1 (OCT1, SLC22A1) can also promote the hepatic efflux of acetylcarnitine and contribute to the plasma acetylcarnitine pool [60]. Another transporter, CACT (carnitine-acylcarnitine translocase) is located in the inner mitochondrial membrane and contributes to the exchange of acylcarnitine and longer acylcarnitines for carnitine to ensure acetylcarnitine transfer across the inner mitochondrial membrane [90].
Acetylcarnitine metabolism
From a biochemical perspective, acetylcarnitine is an accessible form of the acetyl group that can be taken up from food and transported unchanged to the mitochondrial matrix for energy production via the tricarboxylic acid (TCA) cycle. Prior to metabolism in the mitochondria, the acetyl group is transferred to coenzyme A (CoA) to form acetyl-CoA, which enters the TCA cycle to generate ATP through oxidative phosphorylation. In comparison to other substrates of energy metabolism, acetylcarnitine can be considered as one of the fastest, as it does not require extensive metabolic changes such as glycolysis of fatty acid beta-oxidation, which are complex processes involving many enzymes. Comparing the oxygen required for the oxidation of different substrates to generate ATP, the oxygen efficiency of glucose is generally considered to be more favourable than that of acetyl-CoA, which is more similar to fatty acids. Thus, under conditions of limited oxygen availability, glucose would be a preferred substrate. Overall, acetylcarnitine can improve mitochondrial energy status if supplied to tissues in sufficient quantities.
When acetylcarnitine is injected directly into the brain, most of the acetyl groups were metabolized, as 60% of the injected acetylcarnitine was recovered as exhaled 14CO2 after 22 h, and the percentage recovered in the brain was 1.9, 1.6, 1.3, and 0.9% at 1, 3, 6, and 22 h, respectively [109]. Some of the acetylcarnitine was incorporated into saturated fatty acids (about 60% of the radioactivity present in the tissues), but it was also found in monounsaturated fatty acids and PUFAs (polyunsaturated fatty acids). The highest level of acetylcarnitine incorporation into brain lipids is observed 1 h after injection and then gradually decreases, suggesting that the metabolic capacity to utilize the acute increase in acetyl groups may be limited and that the excess of acetyl groups is then rapidly incorporated into lipids. In addition, unmetabolized acetyl groups in the brain may be incorporated into various neurotransmitters [114, 150], but it would be an exaggeration to suggest that the availability of acetyl groups has a direct impact on neurotransmitter release at synapses. In the study by Ricciolini and colleagues, labelled [U-14C]glucose was not incorporated into PUFAs, unlike [1-14C]-acetylcarnitine [109], indicating that the formation of acetyl groups from pyruvate in mitochondria ensures complete metabolism. It is proposed that the beneficial effects of acetylcarnitine include the supply of activated acyl groups for the acylation of membrane phospholipids.
Other mechanisms of acetylcarnitine action
Acetylcarnitine has been suggested to protect against oxidative stress through the induction of antioxidant genes and an increase in HO-1 (heme oxygenase 1) expression in vitro and in vivo [17, 18]. However, it is widely accepted that HO-1 is a heat shock protein that is controlled by inflammatory or pro-oxidant states and is induced in various pathologies in response to oxidative stress [1]. In a study in rats, it was demonstrated that aged rats have significantly upregulated protein expression of HO-1 and acetylcarnitine treatment induces further upregulation of HO-1 expression. It has been suggested that the nuclear factor erythroid 2-related factor 2 (Nrf2) pathway is involved in the induction of HO-1 expression by acetylcarnitine [18]. The Nrf2 pathway is typically induced in response to oxidative stress, inflammation, and other cellular stressors [77]. When activated, the Nrf2 pathway upregulates the expression of a wide range of genes that help to protect cells against various stressors such as reactive oxygen species (ROS), electrophiles, and xenobiotics. In addition to its role in cellular defense, the Nrf2 pathway has been implicated in numerous physiological and pathophysiological processes, including aging, neurodegeneration, cancer, and metabolic disorders [77]. Overall, it is not entirely clear what stress-activation mechanisms might be induced by acetylcarnitine to activate Nrf2 pathway and related gene expression. In many in vitro studies, acetylcarnitine concentrations exceed physiological levels by up to 1000-fold [18, 101, 145, 146]. Therefore, acetylcarnitine activities observed in vitro do not always represent pharmacological effects that could be achieved by acetylcarnitine supplementation in humans.
Clinical efficacy of acetylcarnitine supplementation in neuropsychiatric diseases
Acetylcarnitine supplementation has been shown to reduce the levels of fatigue-associated with several medical conditions, including aging [79], cancer [84], and chronic hepatitis [80]. There is increasing evidence that acetylcarnitine supplementation may also be effective in neuropsychiatric conditions. For example, acetylcarnitine supplementation improved mental fatigue in an open-label, randomized trial in patients with ME/CFS [142].
Multiple sclerosis (MS) is a neuroinflammatory disease. In addition to neurological symptoms, fatigue is reported by most patients with MS and is associated with a poor quality of life [56]. A randomized cross-over trial in thirty-six MS patients with fatigue showed that 3 months of acetylcarnitine supplementation had a more favourable effect on fatigue severity than amantadine supplementation [131]. However, 1 month of acetylcarnitine supplementation showed only a trend-level improvement in the impact of fatigue on daily life in a placebo-controlled, randomised trial in sixty people with relapsing–remitting MS [70].
MDD is another common neuropsychiatric disease associated with fatigue and cognitive dysfunction. A substantial number of patients do not respond adequately to traditional agents [9], and the non-response rate is estimated to be higher in the immuno-metabolic phenotype [147]. Consistent findings indicate the benefit of acetylcarnitine treatment in general and senile MDD patients [10, 11, 41]. In their meta-analysis combining the results of twelve randomized controlled trials, Veronese and colleagues reported a significant decrease in depression severity after acetylcarnitine supplementation as monotherapy compared with placebo intake or no intervention [143]. The incidence of adverse effects with acetylcarnitine supplementation was comparable to that with placebo and lower than with antidepressants, in line with a previous meta-analysis [85]. Furthermore, the acetylcarnitine supplementation has been reported to be as effective as antidepressants in meta-analyses [64, 143]. To the authors’ knowledge, there are no published results on the effectiveness of acetylcarnitine supplementation in immuno-metabolic depression.
There is preliminary evidence in the literature for the benefit of acetylcarnitine in the treatment of long COVID syndrome. A recent observational case–control study reported improvements in the quality of life, depressive complaints, and pain scores after 1 month of combined physical exercise and acetylcarnitine supplementation compared with physical exercise alone [115]. A recent study of patients with long COVID syndrome reported a decrease in fatigue and an increase in subjective energy levels after 2 weeks of taking a supplement containing 150 mg of acetylcarnitine [93]. These findings suggest that acetylcarnitine supplementation is a promising potential treatment for long COVID syndrome. However, to the authors’ knowledge, there are no ongoing, withdrawn or completed clinical trials investigating the potential benefits of acetylcarnitine supplementation in people with long COVID syndrome. It is imperative that future studies are conducted to assess the effect of acetylcarnitine supplementation on the symptoms associated with long COVID syndrome.
Conclusion
In conclusion, we have shown in this manuscript, that neuropsychiatric long COVID syndrome shares considerable symptomatic and multi-level biological overlap with other PAIS [23, 62]. Hence, at least a partial overlap in the underlying pathophysiology and thus potential treatment strategies can be assumed for long COVID, PAIS and ME/CFS. In addition to several classical drugs, a large number of dietary interventions and dietary/nutritional supplements, such as amino acids, probiotics, and plant-based extracts, have been tested or proposed for the treatment of long COVID, due to the usually good accessibility, affordability, safety, and easy application of the respective dietary/nutritional supplements [132].
Acetylcarnitine, which, as we have described, plays an important role in mitochondrial energy metabolism, is an FDA-approved dietary supplement that has been studied for the treatment of fatigue in aging, cancer, chronic hepatitis, ME/CFS, MS, and MDD. Treatment with acetylcarnitine alone or as a part of a combined dietary intervention has resulted in reduced levels of fatigue, decreased depression, improved cognitive status, and/or improved physical function in these disorders.
Interestingly, recent pilot studies have reported preliminary evidence of potential benefits of acetylcarnitine supplementation alone or as part of a combined dietary intervention in the treatment of long COVID-associated fatigue, energy metabolism alterations and immune changes [93, 110]. However, there is still no clear evidence if and how acetylcarnitine supplementation alone can improve neuropsychiatric symptoms of long COVID. Given the clinical success of acetylcarnitine supplementation in other fatigue-associated diseases and the small number of currently available treatments for long COVID, we believe that acetylcarnitine may also be a potentially effective dietary supplement for neuropsychiatric long COVID syndrome and call for further action to investigate this hypothesis in further clinical trials.
Abbreviations
- BBB:
-
Blood–brain barrier
- CFS:
-
Chronic fatigue syndrome
- CNS:
-
Central nervous system
- CoA:
-
Coenzyme A
- COVID-19:
-
Coronavirus disease 2019
- CrAT:
-
Carnitine acetyltransferase
- CRP:
-
C-reactive protein
- HPA:
-
Hypothalamic–pituitary–adrenal
- IDO:
-
Indoleamine 2,3-dioxygenase
- IL-2:
-
Interleukin-2
- IMD:
-
Immunometabolic depression
- MDD:
-
Major depressive disorder
- ME:
-
Myalgic encephalomyelitis
- mGluR2:
-
Metabotropic glutamate receptor 2
- MS:
-
Multiple sclerosis
- NMDA:
-
N-Methyl-d-aspartate
- NMR:
-
Nuclear magnetic resonance
- Nrf2:
-
Nuclear factor erythroid 2-related factor 2
- OCTN2:
-
Organic cation novel type 2 transporter
- OCT1:
-
Organic cation transporter 1
- PAIS:
-
Post-acute infection syndromes
- PASC:
-
Post-acute sequelae of SARS-CoV-2 infection
- PDC:
-
Pyruvate dehydrogenase complex
- PGD2S:
-
Prostaglandin D2 synthase gene
- QUIN:
-
Quinolinic acid
- ROS:
-
Reactive oxygen species
- Trp:
-
Tryptophan
- TCA:
-
Tricarboxylic acid
- HO-1:
-
Heme oxygenase 1
- PUFAs:
-
Polyunsaturated fatty acids
- CACT:
-
Carnitine-acylcarnitine translocase
- MRI:
-
Magnetic resonance imaging
- [18F]FDG-PET/CT:
-
[18F]Fluorodeoxyglucose positron emission tomography/computed tomography
References
Abraham NG, Kappas A (2008) Pharmacological and clinical aspects of heme oxygenase. Pharmacol Rev 60:79–127
Afshin-Majd S, Bashiri K, Kiasalari Z, Baluchnejadmojarad T, Sedaghat R, Roghani M (2017) Acetyl-l-carnitine protects dopaminergic nigrostriatal pathway in 6-hydroxydopamine-induced model of Parkinson’s disease in the rat. Biomed Pharmacother 89:1–9
Al-Dhuayan IS (2023) Biomedical role of l-carnitine in several organ systems, cellular tissues, and Covid-19. Braz J Biol 82:e267633
Alghamdi HY, Alrashed AM, Jawhari AM, Abdel-Moneim AS (2022) Neuropsychiatric symptoms in post-Covid-19 long haulers. Acta Neuropsychiatr 34:318–329
Altamimi TR, Thomas PD, Darwesh AM, Fillmore N, Mahmoud MU, Zhang L, Gupta A, Al Batran R, Seubert JM, Lopaschuk GD (2018) Cytosolic carnitine acetyltransferase as a source of cytosolic acetyl-COA: a possible mechanism for regulation of cardiac energy metabolism. Biochem J 475:959–976
Astin R, Banerjee A, Baker MR, Dani M, Ford E, Hull JH, Lim PB, McNarry M, Morten K, O’Sullivan O, Pretorius E, Raman B, Soteropoulos DS, Taquet M, Hall CN (2023) Long covid: mechanisms, risk factors and recovery. Exp Physiol 108:12–27
Badenoch JB, Rengasamy ER, Watson C, Jansen K, Chakraborty S, Sundaram RD, Hafeez D, Burchill E, Saini A, Thomas L, Cross B, Hunt CK, Conti I, Ralovska S, Hussain Z, Butler M, Pollak TA, Koychev I, Michael BD, Holling H, Nicholson TR, Rogers JP, Rooney AG (2022) Persistent neuropsychiatric symptoms after Covid-19: a systematic review and meta-analysis. Brain Commun 4:fcab297
Barker-Davies RM, Ladlow P, Chamley R, Nicol E, Holdsworth DA (2023) Reduced athletic performance post-Covid-19 is associated with reduced anaerobic threshold. BMJ Case Rep 16:1
Bauer M, Pfennig A, Severus E, Whybrow PC, Angst J, Moller HJ, World Federation of Societies of Biological Psychiatry. Task Force on Unipolar Depressive D (2013) World federation of societies of biological psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, part 1: update 2013 on the acute and continuation treatment of unipolar depressive disorders. World J Biol Psychiatry 14:334–385
Bella R, Biondi R, Raffaele R, Pennisi G (1990) Effect of acetyl-l-carnitine on geriatric patients suffering from dysthymic disorders. Int J Clin Pharmacol Res 10:355–360
Bersani G, Meco G, Denaro A, Liberati D, Colletti C, Nicolai R, Bersani FS, Koverech A (2013) L-acetylcarnitine in dysthymic disorder in elderly patients: a double-blind, multicenter, controlled randomized study vs. Fluoxetine. Eur Neuropsychopharmacol 23:1219–1225
Besteher B, Machnik M, Troll M, Toepffer A, Zerekidze A, Rocktaschel T, Heller C, Kikinis Z, Brodoehl S, Finke K, Reuken PA, Opel N, Stallmach A, Gaser C, Walter M (2022) Larger gray matter volumes in neuropsychiatric long-covid syndrome. Psychiatry Res 317:114836
Borsini A, Merrick B, Edgeworth J, Mandal G, Srivastava DP, Vernon AC, Nebbia G, Thuret S, Pariante CM (2022) Neurogenesis is disrupted in human hippocampal progenitor cells upon exposure to serum samples from hospitalized Covid-19 patients with neurological symptoms. Mol Psychiatry 27:5049–5061
Bot M, Milaneschi Y, Al-Shehri T, Amin N, Garmaeva S, Onderwater GLJ, Pool R, Thesing CS, Vijfhuizen LS, Vogelzangs N, Arts ICW, Demirkan A, van Duijn C, van Greevenbroek M, van der Kallen CJH, Kohler S, Ligthart L, van den Maagdenberg A, Mook-Kanamori DO, de Mutsert R, Tiemeier H, Schram MT, Stehouwer CDA, Terwindt GM, Willems van Dijk K, Fu J, Zhernakova A, Beekman M, Slagboom PE, Boomsma DI, Penninx B, Consortium B-NM (2020) Metabolomics profile in depression: a pooled analysis of 230 metabolic markers in 5283 cases with depression and 10,145 controls. Biol Psychiatry 87:409–418
Brealey D, Brand M, Hargreaves I, Heales S, Land J, Smolenski R, Davies NA, Cooper CE, Singer M (2002) Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet (London) 360:219–223
Burlina AP, Sershen H, Debler EA, Lajtha A (1989) Uptake of acetyl-l-carnitine in the brain. Neurochem Res 14:489–493
Calabrese V, Colombrita C, Sultana R, Scapagnini G, Calvani M, Butterfield DA, Stella AM (2006) Redox modulation of heat shock protein expression by acetylcarnitine in aging brain: relationship to antioxidant status and mitochondrial function. Antioxid Redox Signal 8:404–416
Calabrese V, Ravagna A, Colombrita C, Scapagnini G, Guagliano E, Calvani M, Butterfield DA, Giuffrida Stella AM (2005) Acetylcarnitine induces heme oxygenase in rat astrocytes and protects against oxidative stress: involvement of the transcription factor NRF2. J Neurosci Res 79:509–521
Carruthers BM, Jain AK, De Meirleir KL, Peterson DL, Klimas NG, Lerner AM, Bested AC, Flor-Henry P, Joshi P, Powles ACP, Sherkey JA, van de Sande MI (2011) Myalgic encephalomyelitis/chronic fatigue syndrome. J Chronic Fatigue Syndr 11:7–115
Casaril AM, Dantzer R, Bas-Orth C (2021) Neuronal mitochondrial dysfunction and bioenergetic failure in inflammation-associated depression. Front Neurosci 15:725547
Chang X, Ismail NI, Rahman A, Xu D, Chan RWY, Ong SG, Ong SB (2023) Long Covid-19 and the heart: Is cardiac mitochondria the missing link? Antioxid Redox Signal 38:599–618
Che X, Brydges CR, Yu Y, Price A, Joshi S, Roy A, Lee B, Barupal DK, Cheng A, Palmer DM, Levine S, Peterson DL, Vernon SD, Bateman L, Hornig M, Montoya JG, Komaroff AL, Fiehn O, Lipkin WI (2022) Evidence for peroxisomal dysfunction and dysregulation of the CDP-choline pathway in myalgic encephalomyelitis/chronic fatigue syndrome. medRxiv 2022:1
Choutka J, Jansari V, Hornig M, Iwasaki A (2022) Unexplained post-acute infection syndromes. Nat Med 28:911–923
Correia AS, Vale N (2022) Tryptophan metabolism in depression: a narrative review with a focus on serotonin and kynurenine pathways. Int J Mol Sci 23:1
Cowen PJ, Parry-Billings M, Newsholme EA (1989) Decreased plasma tryptophan levels in major depression. J Affect Disord 16:27–31
Crook H, Raza S, Nowell J, Young M, Edison P (2021) Long covid-mechanisms, risk factors, and management. BMJ 374:n1648
Cysique LA, Jakabek D, Bracken SG, Allen-Davidian Y, Heng B, Chow S, Dehhaghi M, Pires AS, Darley DR, Byrne A, Phetsouphanh C, Kelleher A, Dore GJ, Matthews GV, Guillemin GJ, Brew BJ (2022) Post-acute Covid-19 cognitive impairment and decline uniquely associate with kynurenine pathway activation: a longitudinal observational study. medRxiv:2022.2006.2007.22276020
Dambrova M, Liepinsh E (2015) Risks and benefits of carnitine supplementation in diabetes. Exp Clin Endocrinol Diabetes 123:95–100
Dambrova M, Makrecka-Kuka M, Kuka J, Vilskersts R, Nordberg D, Attwood MM, Smesny S, Sen ZD, Guo AC, Oler E, Tian S, Zheng J, Wishart DS, Liepinsh E, Schioth HB (2022) Acylcarnitines: nomenclature, biomarkers, therapeutic potential, drug targets, and clinical trials. Pharmacol Rev 74:506–551
Daneman R, Prat A (2015) The blood–brain barrier. Cold Spring Harb Perspect Biol 7:a020412
Davis HE, McCorkell L, Vogel JM, Topol EJ (2023) Long covid: major findings, mechanisms and recommendations. Nat Rev Microbiol 21:133–146
de Boer E, Petrache I, Goldstein NM, Olin JT, Keith RC, Modena B, Mohning MP, Yunt ZX, San-Millan I, Swigris JJ (2022) Decreased fatty acid oxidation and altered lactate production during exercise in patients with post-acute Covid-19 syndrome. Am J Respir Crit Care Med 205:126–129
de Oliveira LG, Angelo YDS, Iglesias AH, Peron JPS (2021) Unraveling the link between mitochondrial dynamics and neuroinflammation. Front Immunol 12:1
DiSabato DJ, Quan N, Godbout JP (2016) Neuroinflammation: the devil is in the details. J Neurochem 139(Suppl 2):136–153
Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, Lange F, Andersson JLR, Griffanti L, Duff E, Jbabdi S, Taschler B, Keating P, Winkler AM, Collins R, Matthews PM, Allen N, Miller KL, Nichols TE, Smith SM (2022) SARS-COV-2 is associated with changes in brain structure in uk biobank. Nature 604:697–707
Duan K, Premi E, Pilotto A, Cristillo V, Benussi A, Libri I, Giunta M, Bockholt HJ, Liu J, Campora R, Pezzini A, Gasparotti R, Magoni M, Padovani A, Calhoun VD (2021) Alterations of frontal-temporal gray matter volume associate with clinical measures of older adults with Covid-19. Neurobiol Stress 14:100326
Efstathiou V, Stefanou MI, Demetriou M, Siafakas N, Makris M, Tsivgoulis G, Zoumpourlis V, Kympouropoulos SP, Tsoporis JN, Spandidos DA, Smyrnis N, Rizos E (2022) Long covid and neuropsychiatric manifestations (review). Exp Ther Med 23:363
Ferrario M, Cambiaghi A, Brunelli L, Giordano S, Caironi P, Guatteri L, Raimondi F, Gattinoni L, Latini R, Masson S, Ristagno G, Pastorelli R (2016) Mortality prediction in patients with severe septic shock: a pilot study using a target metabolomics approach. Sci Rep 6:20391
Fries GR, Saldana VA, Finnstein J, Rein T (2023) Molecular pathways of major depressive disorder converge on the synapse. Mol Psychiatry 28:284–297
Frost G, Sleeth ML, Sahuri-Arisoylu M, Lizarbe B, Cerdan S, Brody L, Anastasovska J, Ghourab S, Hankir M, Zhang S, Carling D, Swann JR, Gibson G, Viardot A, Morrison D, Louise Thomas E, Bell JD (2014) The short-chain fatty acid acetate reduces appetite via a central homeostatic mechanism. Nat Commun 5:3611
Garzya G, Corallo D, Fiore A, Lecciso G, Petrelli G, Zotti C (1990) Evaluation of the effects of l-acetylcarnitine on senile patients suffering from depression. Drugs Exp Clin Res 16:101–106
Geary DC (2021) Mitochondrial functioning and the relations among health, cognition, and aging: where cell biology meets cognitive science. Int J Mol Sci 22:1
Germain A, Ruppert D, Levine SM, Hanson MR (2017) Metabolic profiling of a myalgic encephalomyelitis/chronic fatigue syndrome discovery cohort reveals disturbances in fatty acid and lipid metabolism. Mol Biosyst 13:371–379
Gibson EM, Monje M (2021) Microglia in cancer therapy-related cognitive impairment. Trends Neurosci 44:441–451
Gottschalk CG, Peterson D, Armstrong J, Knox K, Roy A (2023) Potential molecular mechanisms of chronic fatigue in long haul covid and other viral diseases. Infect Agent Cancer 18:7
Groven N, Reitan SK, Fors EA, Guzey IC (2021) Kynurenine metabolites and ratios differ between chronic fatigue syndrome, fibromyalgia, and healthy controls. Psychoneuroendocrinology 131:105287
Guedj E, Campion JY, Dudouet P, Kaphan E, Bregeon F, Tissot-Dupont H, Guis S, Barthelemy F, Habert P, Ceccaldi M, Million M, Raoult D, Cammilleri S, Eldin C (2021) (18)F-FDG brain pet hypometabolism in patients with long covid. Eur J Nucl Med Mol Imaging 48:2823–2833
Guntur VP, Nemkov T, de Boer E, Mohning MP, Baraghoshi D, Cendali FI, San-Millan I, Petrache I, D’Alessandro A (2022) Signatures of mitochondrial dysfunction and impaired fatty acid metabolism in plasma of patients with post-acute sequelae of Covid-19 (PASC). Metabolites 12:1
Hafiz R, Gandhi TK, Mishra S, Prasad A, Mahajan V, Di X, Natelson BH, Biswal BB (2022) Higher limbic and basal ganglia volumes in surviving covid-negative patients and the relations to fatigue. Neuroimage Rep 2:100095
Heine J, Schwichtenberg K, Hartung TJ, Rekers S, Chien C, Boesl F, Rust R, Hohenfeld C, Bungenberg J, Costa AS, Scheibenbogen C, Bellmann-Strobl J, Paul F, Franke C, Reetz K, Finke C (2023) Structural brain changes in patients with post-covid fatigue: a prospective observational study. eClin Med 58:1
Henn RE, Noureldein MH, Elzinga SE, Kim B, Savelieff MG, Feldman EL (2022) Glial-neuron crosstalk in health and disease: a focus on metabolism, obesity, and cognitive impairment. Neurobiol Dis 170:105766
Hoglund E, Overli O, Winberg S (2019) Tryptophan metabolic pathways and brain serotonergic activity: a comparative review. Front Endocrinol (Lausanne) 10:158
Hugon J, Queneau M, Sanchez Ortiz M, Msika EF, Farid K, Paquet C (2022) Cognitive decline and brainstem hypometabolism in long covid: a case series. Brain Behav 12:e2513
Inano A, Sai Y, Nikaido H, Hasimoto N, Asano M, Tsuji A, Tamai I (2003) Acetyl-l-carnitine permeability across the blood–brain barrier and involvement of carnitine transporter OCTN2. Biopharm Drug Dispos 24:357–365
Israr MZ, Ibrahim W, Salzano A, Sarmad S, Wilde MJ, Cordell RL, Greening NJ, Brightling CE, Siddiqui S, Suzuki T, Consortium E (2022) Association of gut-related metabolites with respiratory symptoms in Covid-19: a proof-of-concept study. Nutrition 96:111585
Janardhan V, Bakshi R (2000) Quality of life and its relationship to brain lesions and atrophy on magnetic resonance images in 60 patients with multiple sclerosis. Arch Neurol 57:1485–1491
Jensterle M, Herman R, Janež A, Mahmeed WA, Al-Rasadi K, Al-Alawi K, Banach M, Banerjee Y, Ceriello A, Cesur M, Cosentino F, Galia M, Goh SY, Kalra S, Kempler P, Lessan N, Lotufo P, Papanas N, Rizvi AA, Santos RD, Stoian AP, Toth PP, Viswanathan V, Rizzo M (2022) The relationship between Covid-19 and hypothalamic–pituitary–adrenal axis: a large spectrum from glucocorticoid insufficiency to excess—the capisco international expert panel. Int J Mol Sci 23:1
Kadry H, Noorani B, Cucullo L (2020) A blood–brain barrier overview on structure, function, impairment, and biomarkers of integrity. Fluids Barriers CNS 17:69
Kido Y, Tamai I, Ohnari A, Sai Y, Kagami T, Nezu J, Nikaido H, Hashimoto N, Asano M, Tsuji A (2001) Functional relevance of carnitine transporter OCTN2 to brain distribution of l-carnitine and acetyl-l-carnitine across the blood–brain barrier. J Neurochem 79:959–969
Kim HI, Raffler J, Lu W, Lee JJ, Abbey D, Saleheen D, Rabinowitz JD, Bennett MJ, Hand NJ, Brown C, Rader DJ (2017) Fine mapping and functional analysis reveal a role of SLC22A1 in acylcarnitine transport. Am J Hum Genet 101:489–502
Klein R, Soung A, Sissoko C, Nordvig A, Canoll P, Mariani M, Jiang X, Bricker T, Goldman J, Rosoklija G, Arango V, Underwood M, Mann JJ, Boon A, Dowrk A, Boldrini M (2021) Covid-19 induces neuroinflammation and loss of hippocampal neurogenesis. Res Sq 2021:1
Komaroff AL, Lipkin WI (2021) Insights from myalgic encephalomyelitis/chronic fatigue syndrome may help unravel the pathogenesis of postacute Covid-19 syndrome. Trends Mol Med 27:895–906
Kovarik JJ, Bileck A, Hagn G, Meier-Menches SM, Frey T, Kaempf A, Hollenstein M, Shoumariyeh T, Skos L, Reiter B, Gerner MC, Spannbauer A, Hasimbegovic E, Schmidl D, Garhofer G, Gyongyosi M, Schmetterer KG, Gerner C (2023) A multi-omics based anti-inflammatory immune signature characterizes long Covid-19 syndrome. iScience 26:105717
Kriston L, von Wolff A, Westphal A, Holzel LP, Harter M (2014) Efficacy and acceptability of acute treatments for persistent depressive disorder: a network meta-analysis. Depress Anxiety 31:621–630
Kubota T, Kuroda N, Sone D (2022) Neuropsychiatric aspects of long covid: a comprehensive review. Psychiatry Clin Neurosci 2022:1
Kucukkarapinar M, Yay-Pence A, Yildiz Y, Buyukkoruk M, Yaz-Aydin G, Deveci-Bulut TS, Gulbahar O, Senol E, Candansayar S (2022) Psychological outcomes of Covid-19 survivors at sixth months after diagnose: the role of kynurenine pathway metabolites in depression, anxiety, and stress. J Neural Transm (Vienna) 129:1077–1089
Kuratsune H, Watanabe Y, Yamaguti K, Jacobsson G, Takahashi M, Machii T, Onoe H, Onoe K, Matsumura K, Valind S, Kitani T, Langstrom B (1997) High uptake of [2-11c]acetyl-l-carnitine into the brain: a pet study. Biochem Biophys Res Commun 231:488–493
Ladds E, Rushforth A, Wieringa S, Taylor S, Rayner C, Husain L, Greenhalgh T (2020) Persistent symptoms after Covid-19: qualitative study of 114 “long covid” patients and draft quality principles for services. BMC Health Serv Res 20:1144
Lamers F, Milaneschi Y, Penninx BWJH (2018) Depression subtypes and inflammation: atypical rather than melancholic depression is linked with immunometabolic dysregulations. Inflammation Immunity Depression 2018:455–471
Ledinek AH, Sajko MC, Rot U (2013) Evaluating the effects of amantadin, modafinil and acetyl-l-carnitine on fatigue in multiple sclerosis—result of a pilot randomized, blind study. Clin Neurol Neurosurg 115(Suppl 1):S86-89
Lim EJ, Ahn YC, Jang ES, Lee SW, Lee SH, Son CG (2020) Systematic review and meta-analysis of the prevalence of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). J Transl Med 18:100
Lin T-N, Cheung W-M, Wu J-S, Chen J-J, Lin H, Chen J-J, Liou J-Y, Shyue S-K, Wu KK (2006) 15d-prostaglandin J2 protects brain from ischemia-reperfusion injury. Arterioscler Thromb Vasc Biol 26:481–487
Liu T, Deng K, Xue Y, Yang R, Yang R, Gong Z, Tang M (2022) Carnitine and depression. Front Nutr 9:853058
Fgc LN, Carneiro BA, Alves GS, Lins Silva DH, Faria Guimaraes D, Souza LS, Bandeira ID, Beanes G, Miranda Scippa A, Quarantini LC (2022) Metabolomics of major depressive disorder: a systematic review of clinical studies. Cureus 14:e23009
Longo N, Frigeni M, Pasquali M (2016) Carnitine transport and fatty acid oxidation. Biochem Biophys Acta 1863:2422–2435
Lukic I, Ivkovic S, Mitic M, Adzic M (2022) Tryptophan metabolites in depression: modulation by gut microbiota. Front Behav Neurosci 16:987697
Ma Q (2013) Role of NRF2 in oxidative stress and toxicity. Annu Rev Pharmacol Toxicol 53:401–426
Magnus P, Gunnes N, Tveito K, Bakken IJ, Ghaderi S, Stoltenberg C, Hornig M, Lipkin WI, Trogstad L, Haberg SE (2015) Chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) is associated with pandemic influenza infection, but not with an adjuvanted pandemic influenza vaccine. Vaccine 33:6173–6177
Malaguarnera M, Gargante MP, Cristaldi E, Colonna V, Messano M, Koverech A, Neri S, Vacante M, Cammalleri L, Motta M (2008) Acetyl l-carnitine (ALC) treatment in elderly patients with fatigue. Arch Gerontol Geriatr 46:181–190
Malaguarnera M, Vacante M, Bertino G, Neri S, Malaguarnera M, Gargante MP, Motta M, Lupo L, Chisari G, Bruno CM, Pennisi G, Bella R (2011) The supplementation of acetyl-l-carnitine decreases fatigue and increases quality of life in patients with hepatitis c treated with pegylated interferon-alpha 2B plus ribavirin. J Interferon Cytokine Res 31:653–659
Malaguarnera M, Vacante M, Giordano M, Pennisi G, Bella R, Rampello L, Malaguarnera M, Li Volti G, Galvano F (2011) Oral acetyl-l-carnitine therapy reduces fatigue in overt hepatic encephalopathy: a randomized, double-blind, placebo-controlled study. Am J Clin Nutr 93:799–808
Marks DF (2023) Converging evidence of similar symptomatology of ME/CFS and pasc indicating multisystemic dyshomeostasis. Biomedicines 11:1
Markwell MA, McGroarty EJ, Bieber LL, Tolbert NE (1973) The subcellular distribution of carnitine acyltransferases in mammalian liver and kidney. A new peroxisomal enzyme. J Biol Chem 248:3426–3432
Marx W, Teleni L, Opie R, Kelly J, Marshall S, Itsiopoulos C, Isenring E (2017) Efficacy and effectiveness of carnitine supplementation for cancer-related fatigue: a systematic literature review and meta-analysis. Nutrients 9:1
Meister R, von Wolff A, Mohr H, Harter M, Nestoriuc Y, Holzel L, Kriston L (2016) Comparative safety of pharmacologic treatments for persistent depressive disorder: a systematic review and network meta-analysis. PLoS ONE 11:e0153380
Milaneschi Y, Lamers F, Berk M, Penninx B (2020) Depression heterogeneity and its biological underpinnings: toward immunometabolic depression. Biol Psychiatry 88:369–380
Miller AH, Maletic V, Raison CL (2009) Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry 65:732–741
Monje M, Iwasaki A (2022) The neurobiology of long covid. Neuron 110:3484–3496
Morand A, Campion JY, Lepine A, Bosdure E, Luciani L, Cammilleri S, Chabrol B, Guedj E (2022) Similar patterns of [(18)F]-FDG brain pet hypometabolism in paediatric and adult patients with long covid: a paediatric case series. Eur J Nucl Med Mol Imaging 49:913–920
Murthy MS, Pande SV (1984) Mechanism of carnitine acylcarnitine translocase-catalyzed import of acylcarnitines into mitochondria. J Biol Chem 259:9082–9089
Nagy-Szakal D, Barupal DK, Lee B, Che X, Williams BL, Kahn EJR, Ukaigwe JE, Bateman L, Klimas NG, Komaroff AL, Levine S, Montoya JG, Peterson DL, Levin B, Hornig M, Fiehn O, Lipkin WI (2018) Insights into myalgic encephalomyelitis/chronic fatigue syndrome phenotypes through comprehensive metabolomics. Sci Rep 8:10056
Nasca C, Xenos D, Barone Y, Caruso A, Scaccianoce S, Matrisciano F, Battaglia G, Mathé AA, Pittaluga A, Lionetto L, Simmaco M, Nicoletti F (2013) L-acetylcarnitine causes rapid antidepressant effects through the epigenetic induction of MGLU2 receptors. Proc Natl Acad Sci 110:4804–4809
Naureen Z, Dautaj A, Nodari S, Fioretti F, Dhuli K, Anpilogov K, Lorusso L, Paolacci S, Michelini S, Guda T, Kallazi M, Bertelli M (2021) Proposal of a food supplement for the management of post-covid syndrome. Eur Rev Med Pharmacol Sci 25:67–73
Nelson T, Zhang LX, Guo H, Nacul L, Song X (2021) Brainstem abnormalities in myalgic encephalomyelitis/chronic fatigue syndrome: a scoping review and evaluation of magnetic resonance imaging findings. Front Neurol 12:769511
Niu YJ, Jiang ZM, Shu H, Li CF, Liu W, Yao GX, Jiang J, Li JQ, Longo A (2002) Assay of carnitine in plasma and urine of healthy adults. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 24:185–187
Noland RC, Koves TR, Seiler SE, Lum H, Lust RM, Ilkayeva O, Stevens RD, Hegardt FG, Muoio DM (2009) Carnitine insufficiency caused by aging and overnutrition compromises mitochondrial performance and metabolic control. J Biol Chem 284:22840–22852
Ong IZ, Kolson DL, Schindler MK (2023) Mechanisms, effects, and management of neurological complications of post-acute sequelae of Covid-19 (NC-PASC). Biomedicines 11:1
Paolini M, Palladini M, Mazza MG, Colombo F, Vai B, Rovere-Querini P, Falini A, Poletti S, Benedetti F (2023) Brain correlates of subjective cognitive complaints in Covid-19 survivors: a multimodal magnetic resonance imaging study. Eur Neuropsychopharmacol 68:1–10
Peter RS, Nieters A, Krausslich HG, Brockmann SO, Gopel S, Kindle G, Merle U, Steinacker JM, Rothenbacher D, Kern WV, Group EPS (2022) Post-acute sequelae of Covid-19 six to 12 months after infection: population based study. BMJ 379:e071050
Petschner P, Gonda X, Baksa D, Eszlari N, Trivaks M, Juhasz G, Bagdy G (2018) Genes linking mitochondrial function, cognitive impairment and depression are associated with endophenotypes serving precision medicine. Neuroscience 370:207–217
Pillich RT, Scarsella G, Risuleo G (2005) Reduction of apoptosis through the mitochondrial pathway by the administration of acetyl-l-carnitine to mouse fibroblasts in culture. Exp Cell Res 306:1–8
Piotrowicz K, Gasowski J, Michel JP, Veronese N (2021) Post-Covid-19 acute sarcopenia: physiopathology and management. Aging Clin Exp Res 33:2887–2898
Prasada Kabekkodu S, Chakrabarty S, Jayaram P, Mallya S, Thangaraj K, Singh KK, Satyamoorthy K (2023) Severe acute respiratory syndrome coronaviruses contributing to mitochondrial dysfunction: implications for post-covid complications. Mitochondrion 69:43–56
Proal AD, VanElzakker MB (2021) Long covid or post-acute sequelae of Covid-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front Microbiol 12:698169
Psychogios N, Hau DD, Peng J, Guo AC, Mandal R, Bouatra S, Sinelnikov I, Krishnamurthy R, Eisner R, Gautam B, Young N, Xia J, Knox C, Dong E, Huang P, Hollander Z, Pedersen TL, Smith SR, Bamforth F, Greiner R, McManus B, Newman JW, Goodfriend T, Wishart DS (2011) The human serum metabolome. PLoS ONE 6:e16957
Ramsay RR, Gandour RD, van der Leij FR (2001) Molecular enzymology of carnitine transfer and transport. Biochem Biophys Acta 1546:21–43
Rebouche CJ (2004) Kinetics, pharmacokinetics, and regulation of l-carnitine and acetyl-l-carnitine metabolism. Ann N Y Acad Sci 1033:30–41
Reuter SE, Evans AM (2012) Carnitine and acylcarnitines: pharmacokinetic, pharmacological and clinical aspects. Clin Pharmacokinet 51:553–572
Ricciolini R, Scalibastri M, Kelleher JK, Carminati P, Calvani M, Arduini A (1998) Role of acetyl-l-carnitine in rat brain lipogenesis: implications for polyunsaturated fatty acid biosynthesis. J Neurochem 71:2510–2517
Rossato MS, Brilli E, Ferri N, Giordano G, Tarantino G (2021) Observational study on the benefit of a nutritional supplement, supporting immune function and energy metabolism, on chronic fatigue associated with the SARS-COV-2 post-infection progress. Clin Nutr ESPEN 46:510–518
Sadlier C, Albrich WC, Neogi U, Lunjani N, Horgan M, O’Toole PW, O’Mahony L (2022) Metabolic rewiring and serotonin depletion in patients with postacute sequelae of Covid-19. Allergy 77:1623–1625
Samin A, Al Kury LT, Imran-Khan M, Hussain S, Alattar A, Alshaman R, Shah FA, Aamir M, Li S (2021) Acetyl-l-carnitine protects against LPS induced depression via PPAR-γ induced inhibition of NF-ΚB/NLRP3 pathway. Arch Med Sci 2021:1
Sampogna G, Di Vincenzo M, Giallonardo V, Perris F, Volpicelli A, Del Vecchio V, Luciano M, Fiorillo A (2022) The psychiatric consequences of long-covid: a scoping review. J Pers Med 12:1
Scafidi S, Fiskum G, Lindauer SL, Bamford P, Shi D, Hopkins I, McKenna MC (2010) Metabolism of acetyl-l-carnitine for energy and neurotransmitter synthesis in the immature rat brain. J Neurochem 114:820–831
Scaturro D, Vitagliani F, Di Bella VE, Falco V, Tomasello S, Lauricella L, Letizia Mauro G (2022) The role of acetyl-carnitine and rehabilitation in the management of patients with post-covid syndrome: case–control study. Appl Sci 12:4084
Singer M (2014) The role of mitochondrial dysfunction in sepsis-induced multi-organ failure. Virulence 5:66–72
Smeland OB, Meisingset TW, Borges K, Sonnewald U (2012) Chronic acetyl-l-carnitine alters brain energy metabolism and increases noradrenaline and serotonin content in healthy mice. Neurochem Int 61:100–107
Soetekouw PM, Wevers RA, Vreken P, Elving LD, Janssen AJ, van der Veen Y, Bleijenberg G, van der Meer JW (2000) Normal carnitine levels in patients with chronic fatigue syndrome. Neth J Med 57:20–24
Sollini M, Morbelli S, Ciccarelli M, Cecconi M, Aghemo A, Morelli P, Chiola S, Gelardi F, Chiti A (2021) Long covid hallmarks on [18F]FDG-pet/ct: a case–control study. Eur J Nucl Med Mol Imaging 48:3187–3197
Stengel A, Malek N, Zipfel S, Goepel S (2021) Long haulers—What is the evidence for post-covid fatigue? Front Psychiatry 12:677934
Stephens FB, Constantin-Teodosiu D, Greenhaff PL (2007) New insights concerning the role of carnitine in the regulation of fuel metabolism in skeletal muscle. J Physiol 581:431–444
Strijbis K, Vaz FM, Distel B (2010) Enzymology of the carnitine biosynthesis pathway. IUBMB Life 62:357–362
Su J, Thapaliya K, Eaton-Fitch N, Marshall-Gradisnik S, Barnden L (2023) Connectivity between salience and default mode networks and subcortical nodes distinguishes between two classes of myalgic encephalomyelitis/chronic fatigue syndrome. Brain Connect 13:164–173
Su Y, Yuan D, Chen DG, Ng RH, Wang K, Choi J, Li S, Hong S, Zhang R, Xie J, Kornilov SA, Scherler K, Pavlovitch-Bedzyk AJ, Dong S, Lausted C, Lee I, Fallen S, Dai CL, Baloni P, Smith B, Duvvuri VR, Anderson KG, Li J, Yang F, Duncombe CJ, McCulloch DJ, Rostomily C, Troisch P, Zhou J, Mackay S, DeGottardi Q, May DH, Taniguchi R, Gittelman RM, Klinger M, Snyder TM, Roper R, Wojciechowska G, Murray K, Edmark R, Evans S, Jones L, Zhou Y, Rowen L, Liu R, Chour W, Algren HA, Berrington WR, Wallick JA, Cochran RA, Micikas ME, Unit IS-SC-B, Wrin T, Petropoulos CJ, Cole HR, Fischer TD, Wei W, Hoon DSB, Price ND, Subramanian N, Hill JA, Hadlock J, Magis AT, Ribas A, Lanier LL, Boyd SD, Bluestone JA, Chu H, Hood L, Gottardo R, Greenberg PD, Davis MM, Goldman JD, Heath JR (2022) Multiple early factors anticipate post-acute Covid-19 sequelae. Cell 185:881-895 e820
Sumbalova Z, Kucharska J, Rausova Z, Palacka P, Kovalcikova E, Takacsova T, Mojto V, Navas P, Lopez-Lluch G, Gvozdjakova A (2022) Reduced platelet mitochondrial respiration and oxidative phosphorylation in patients with post Covid-19 syndrome are regenerated after SPA rehabilitation and targeted ubiquinol therapy. Front Mol Biosci 9:1016352
Taquet M, Sillett R, Zhu L, Mendel J, Camplisson I, Dercon Q, Harrison PJ (2022) Neurological and psychiatric risk trajectories after SARS-COV-2 infection: an analysis of 2-year retrospective cohort studies including 1,284,437 patients. Lancet Psychiatry 9:815–827
Tate W, Walker M, Sweetman E, Helliwell A, Peppercorn K, Edgar C, Blair A, Chatterjee A (2022) Molecular mechanisms of neuroinflammation in ME/CFS and long covid to sustain disease and promote relapses. Front Neurol 13:877772
Tedjasukmana R, Budikayanti A, Islamiyah WR, Witjaksono A, Hakim M (2022) Sleep disturbance in post Covid-19 conditions: prevalence and quality of life. Front Neurol 13:1095606
Thapaliya K, Marshall-Gradisnik S, Staines D, Barnden L (2021) Diffusion tensor imaging reveals neuronal microstructural changes in myalgic encephalomyelitis/chronic fatigue syndrome. Eur J Neurosci 54:6214–6228
Tirelli U, Chierichetti F, Tavio M, Simonelli C, Bianchin G, Zanco P, Ferlin G (1998) Brain positron emission tomography (PET) in chronic fatigue syndrome: preliminary data. Am J Med 105:54S-58S
Tomassini V, Pozzilli C, Onesti E, Pasqualetti P, Marinelli F, Pisani A, Fieschi C (2004) Comparison of the effects of acetyl l-carnitine and amantadine for the treatment of fatigue in multiple sclerosis: results of a pilot, randomised, double-blind, crossover trial. J Neurol Sci 218:103–108
Tosato M, Ciciarello F, Zazzara MB, Pais C, Savera G, Picca A, Galluzzo V, Coelho-Junior HJ, Calvani R, Marzetti E, Landi F, Gemelli Against C-P-ACT (2022) Nutraceuticals and dietary supplements for older adults with long Covid-19. Clin Geriatr Med 38:565–591
Trabado S, Al-Salameh A, Croixmarie V, Masson P, Corruble E, Feve B, Colle R, Ripoll L, Walther B, Boursier-Neyret C, Werner E, Becquemont L, Chanson P (2017) The human plasma-metabolome: reference values in 800 french healthy volunteers; impact of cholesterol, gender and age. PLoS ONE 12:e0173615
Traina G, Federighi G, Brunelli M, Scuri R (2009) Cytoprotective effect of acetyl-l-carnitine evidenced by analysis of gene expression in the rat brain. Mol Neurobiol 39:101–106
Triebelhorn J, Cardon I, Kuffner K, Bader S, Jahner T, Meindl K, Rothhammer-Hampl T, Riemenschneider MJ, Drexler K, Berneburg M, Nothdurfter C, Manook A, Brochhausen C, Baghai TC, Hilbert S, Rupprecht R, Milenkovic VM, Wetzel CH (2022) Induced neural progenitor cells and ips-neurons from major depressive disorder patients show altered bioenergetics and electrophysiological properties. Mol Psychiatry 2022:1
Tsai SY, Chen HJ, Chen C, Lio CF, Kuo CF, Leong KH, Wang YT, Yang TY, You CH, Wang WS (2019) Increased risk of chronic fatigue syndrome following psoriasis: a nationwide population-based cohort study. J Transl Med 17:154
Tsai SY, Chen HJ, Lio CF, Kuo CF, Kao AC, Wang WS, Yao WC, Chen C, Yang TY (2019) Increased risk of chronic fatigue syndrome in patients with inflammatory bowel disease: a population-based retrospective cohort study. J Transl Med 17:55
Tsai SY, Lin CL, Shih SC, Hsu CW, Leong KH, Kuo CF, Lio CF, Chen YT, Hung YJ, Shi L (2018) Increased risk of chronic fatigue syndrome following burn injuries. J Transl Med 16:342
Tsai SY, Yang TY, Chen HJ, Chen CS, Lin WM, Shen WC, Kuo CN, Kao CH (2014) Increased risk of chronic fatigue syndrome following herpes zoster: a population-based study. Eur J Clin Microbiol Infect Dis 33:1653–1659
Van Hoof E, Cluydts R, De Meirleir K (2003) Atypical depression as a secondary symptom in chronic fatigue syndrome. Med Hypotheses 61:52–55
Vanderheiden A, Klein RS (2022) Neuroinflammation and Covid-19. Curr Opin Neurobiol 76:102608
Vermeulen RC, Scholte HR (2004) Exploratory open label, randomized study of acetyl- and propionylcarnitine in chronic fatigue syndrome. Psychosom Med 66:276–282
Veronese N, Stubbs B, Solmi M, Ajnakina O, Carvalho AF, Maggi S (2018) Acetyl-l-carnitine supplementation and the treatment of depressive symptoms: a systematic review and meta-analysis. Psychosom Med 80:154–159
Violante S, Ijlst L, Ruiter J, Koster J, van Lenthe H, Duran M, de Almeida IT, Wanders RJ, Houten SM, Ventura FV (2013) Substrate specificity of human carnitine acetyltransferase: implications for fatty acid and branched-chain amino acid metabolism. Biochem Biophys Acta 1832:773–779
Virmani MA, Biselli R, Spadoni A, Rossi S, Corsico N, Calvani M, Fattorossi A, De Simone C, Arrigoni-Martelli E (1995) Protective actions of l-carnitine and acetyl-l-carnitine on the neurotoxicity evoked by mitochondrial uncoupling or inhibitors. Pharmacol Res 32:383–389
Virmani MA, Caso V, Spadoni A, Rossi S, Russo F, Gaetani F (2001) The action of acetyl-l-carnitine on the neurotoxicity evoked by amyloid fragments and peroxide on primary rat cortical neurones. Ann N Y Acad Sci 939:162–178
Vogelzangs N, Beekman AT, van Reedt Dortland AK, Schoevers RA, Giltay EJ, de Jonge P, Penninx BW (2014) Inflammatory and metabolic dysregulation and the 2-year course of depressive disorders in antidepressant users. Neuropsychopharmacology 39:1624–1634
Wang S, Zhao Y, Li J (2023) True grit and brain: trait grit mediates the connection of DLPFC functional connectivity density to posttraumatic growth following Covid-19. J Affect Disord 325:313–320
Westin MA, Hunt MC, Alexson SE (2008) Short- and medium-chain carnitine acyltransferases and ACYL-COA thioesterases in mouse provide complementary systems for transport of beta-oxidation products out of peroxisomes. Cell Mol Life Sci 65:982–990
White HL, Scates PW (1990) Acetyl-l-carnitine as a precursor of acetylcholine. Neurochem Res 15:597–601
Whitmer JT, Idell-Wenger JA, Rovetto MJ, Neely JR (1978) Control of fatty acid metabolism in ischemic and hypoxic hearts. J Biol Chem 253:4305–4309
Wingrove J, Makaronidis J, Prados F, Kanber B, Yiannakas MC, Magee C, Castellazzi G, Grandjean L, Golay X, Tur C, Ciccarelli O, D’Angelo E, Gandini Wheeler-Kingshott CAM, Batterham RL (2023) Aberrant olfactory network functional connectivity in people with olfactory dysfunction following Covid-19 infection: an exploratory, observational study. eClin Med 58:101883
Woelfer M, Kasties V, Kahlfuss S, Walter M (2019) The role of depressive subtypes within the neuroinflammation hypothesis of major depressive disorder. Neuroscience 403:93–110
Wright-Jin EC, Gutmann DH (2019) Microglia as dynamic cellular mediators of brain function. Trends Mol Med 25:967–979
Wu X, Huang W, Prasad PD, Seth P, Rajan DP, Leibach FH, Chen J, Conway SJ, Ganapathy V (1999) Functional characteristics and tissue distribution pattern of organic cation transporter 2 (OCTN2), an organic cation/carnitine transporter. J Pharmacol Exp Ther 290:1482–1492
Yong SJ (2021) Persistent brainstem dysfunction in long-covid: a hypothesis. ACS Chem Neurosci 12:573–580
Zordoky BN, Sung MM, Ezekowitz J, Mandal R, Han B, Bjorndahl TC, Bouatra S, Anderson T, Oudit GY, Wishart DS, Dyck JR, Alberta H (2015) Metabolomic fingerprint of heart failure with preserved ejection fraction. PLoS ONE 10:e0124844
Acknowledgements
Open access funding provided by Projekt DEAL.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the European Union’s Horizon 2020 research and innovation programme under Grant Agreement No. 857394 (FAT4BRAIN).
Author information
Authors and Affiliations
Contributions
Literature search: DLH, EMD, EL, LVD, LZ, AR, ZDS, BB. Conceptualization: DLH, EMD, EL, LVS, LZ, AR, ZDS, HBS, MW, MD, BB. Original draft preparation: DLH, EMD, EL, LVD, AR, ZDS, BB. Writing—review and editing: DLH, EMD, LVD, LZ, TR, LKS, HBS, MW, MD, BB.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest to declare.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Helbing, D.L., Dommaschk, EM., Danyeli, L.V. et al. Conceptual foundations of acetylcarnitine supplementation in neuropsychiatric long COVID syndrome: a narrative review. Eur Arch Psychiatry Clin Neurosci (2024). https://doi.org/10.1007/s00406-023-01734-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00406-023-01734-3