Abstract
Background
Autosomal recessive spastic ataxia of Charlevoix–Saguenay (ARSACS) is a rare early onset neurodegenerative disease that typically results in ataxia, upper motor neuron dysfunction and sensorimotor peripheral neuropathy. Dysarthria and dysphagia are anecdotally described as key features of ARSACS but the nature, severity and impact of these deficits in ARSACS are not known. A comprehensive quantitative and qualitative characterization of speech and swallowing function will support diagnostics, provide insights into the underlying pathology, and guide day-to-day clinical management.
Methods
11 consecutive non-Quebec ARSACS patients were recruited, and compared to healthy participants from several published and unpublished cohorts. A comprehensive behavioural assessment including objective acoustic analysis and expert perceptual ratings of motor speech, the Clinical Assessment of Dysphagia in Neurodegeneration (CADN), videofluoroscopy and standardized tests of dysarthria and swallowing related quality of life was conducted.
Results
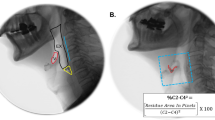
Speech in this ARSACS cohort is characterized by pitch breaks, prosodic deficits including reduced rate and prolonged intervals, and articulatory deficits. The swallowing profile was characterized by delayed initiation of the swallowing reflex and late epiglottic closure. Four out of ten patients were observed aspirating thin liquids on videofluoroscopy. Patients report that they regularly cough or choke on thin liquids and solids during mealtimes. Swallowing and speech-related quality of life was worse than healthy controls on all domains except sleep.
Conclusions
The dysphagia and dysarthria profile of this ARSACS cohort reflects impaired coordination and timing. Dysphagia contributes to a significant impairment in functional quality of life in ARSACS, and appears to manifest distinctly from other ARSACS dysfunctions such as ataxia or spasticity.


Similar content being viewed by others
References
Engert JC, Berube P, Mercier J et al (2000) ARSACS, a spastic ataxia common in northeastern Quebec, is caused by mutations in a new gene encoding an 11.5-kb ORF. Nat Genet 24(2):120–125
Girard M, Larivière R, Parfitt DA et al (2012) Mitochondrial dysfunction and Purkinje cell loss in autosomal recessive spastic ataxia of Charlevoix–Saguenay (ARSACS). Proc Natl Acad Sci 109(5):1661–1666
Pilliod J, Moutton S, Lavie J et al (2015) New practical definitions for the diagnosis of autosomal recessive spastic ataxia of Charlevoix–Saguenay. Ann Neurol 78(6):871–886
Vermeer S, Meijer RPP, Pijl BJ et al (2008) ARSACS in the Dutch population: a frequent cause of early-onset cerebellar ataxia. Neurogenetics 9(3):207–214
Synofzik M, Soehn AS, Gburek-Augustat J et al (2013) Autosomal recessive spastic ataxia of Charlevoix Saguenay (ARSACS): expanding the genetic, clinical and imaging spectrum. Orphanet J Rare Dis 8:41
Ouyang Y, Takiyama Y, Sakoe K et al (2006) Sacsin-related ataxia (ARSACS): Expanding the genotype upstream from the gigantic exon. Neurology 66(7):1103–1104
Isono C, Hirano M, Sakamoto H, Ueno S, Kusunoki S, Nakamura Y (2015) Differential progression of dysphagia in heredity and sporadic ataxias involving multiple systems. Eur Neurol 74(5–6):237–242
Folker JE, Murdoch BE, Cahill LM, Delatycki MB, Corben LA, Vogel AP (2010) Dysarthria in Friedreich’s ataxia: a perceptual analysis. Folia Phoniatrica et Logopaedia 62(3):97–103
Keage MJ, Corben LC, Delatycki MB, Vogel AP (2017) Dysphagia in Friedreich’s ataxia. Dysphagia 32:626–635
Vogel AP, Rommel N, Oettinger A et al (2017) Speech and swallowing abnormalities in adults with POLG associated ataxia (POLG-A). Mitochondrion 37:1–7
Gibilisco P, Vogel AP (2013) Friedreich ataxia. BMJ 347:f7062
Heemskerk A-W, Roos RA (2012) Aspiration pneumonia and death in Huntington’s disease. PLoS Curr 4:RRN1293
Tsou AY, Paulsen EK, Lagedrost SJ et al (2011) Mortality in Friedreich Ataxia. J Neurol Sci 307(1–2):46–49
Schmitz-Hubsch T, Du Montcel ST, Baliko L et al (2006) Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology 66(11):1717–1720
Scott A, Perry A, Bench J (1998) A study of interrater reliability when using videofluoroscopy as an assessment of swallowing. Dysphagia 13(4):223–227
Vogel AP, Rommel N, Sauer C et al (2017) Clinical assessment of dysphagia in neurodegeneration (CADN): development, validity and reliability of a bedside tool for dysphagia assessment. J Neurol 264(6):1107–1117
McHorney CA, Martin-Harris B, Robbins JA, Rosenbek JC (2006) Clinical validity of the SWAL-QOL and SWAL-CARE outcome tools with respect to bolus flow measures. Dysphagia 21(3):141–148
Kraus E-M, Rommel N, Stoll LH, Oettinger A, Vogel AP, Synofzik M (2018) Validation and psychometric properties of the German version of the SWAL-QOL. Dysphagia. https://doi.org/10.1007/s00455-017-9872-5
Nasreddine ZS, Phillips NA, Bédirian V et al (2005) The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53(4):695–699
Katz S (1983) Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc 31(12):721–727
Vogel AP, Rommel N, Sauer C, Synofzik M (2016) Clinical assessment of dysphagia in neurodegeneration (CADN): reliability and validity. Eur J Neurol 23:226
Keage MJ, Delatycki M, Corben LA, Vogel AP (2015) A systematic review of self-reported swallowing assessments in progressive neurological disorders. Dysphagia 30(1):27–46
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL (1996) A penetration-aspiration scale. Dysphagia 11(2):93–98
Vogel AP, Fletcher J, Snyder PJ, Fredrickson A, Maruff P (2011) Reliability, stability, and sensitivity to change and impairment in acoustic measures of timing and frequency. J Voice 25(2):137–149
Vogel AP, Maruff P (2014) Monitoring change requires a rethink of assessment practices in voice and speech. Logop Phoniatr Vocol 39(2):56–61
Vogel AP, Fletcher J, Maruff P (2014) The impact of task automaticity on speech in noise. Speech Commun 65:1–8
Vogel AP, Poole ML, Pemberton H et al (2017) Motor speech signature of behavioral variant frontotemporal dementia: refining the phenotype. Neurology 89(8):837–844
Rosen KM, Folker JE, Vogel AP, Corben LA, Murdoch BE, Delatycki MB (2012) Longitudinal change in dysarthria associated with Friedreich ataxia: a potential clinical endpoint. J Neurol 259(11):2471–2477
Vogel AP, Shirbin C, Churchyard AJ, Stout JC (2012) Speech acoustic markers of early stage and prodromal Huntington’s disease: a marker of disease onset? Neuropsychologia 50(14):3273–3278
Boersma P (2001) Praat, a system for doing phonetics by computer. Glot Int 5(9/10):341–347
Enderby P, Palmer R (2012) FDA-2: Frenchay Dysarthrie assessment—2. Schulz-Kirchner, Idstein
Walshe M, Peach RK, Miller N (2009) Dysarthria impact profile: development of a scale to measure psychosocial effects. Int J Lang Commun Disord 44(5):693–715
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum, Hillsdale
Mariën P, Ackermann H, Adamaszek M et al (2014) Consensus paper: language and the cerebellum: an ongoing enigma. Cerebellum 13(3):386–410
Vogel AP, Wardrop MI, Folker JE et al (2017) Voice in Friedreich Ataxia. J Voice 31(2):243.e249–243.e219
Letanneux A, Walshe M, Viallet F, Pinto S (2013) The Dysarthria impact profile: a preliminary french experience with Parkinson’s disease. Parkinson’s Dis 2013:6
Park S, Theodoros DG, Finch E, Cardell E (2016) Be clear: a new intensive speech treatment for adults with nonprogressive dysarthria. Am J Speech Lang Pathol 25(1):97–110
Theodoros DG, Hill AJ, Russell TG (2016) Clinical and quality of life outcomes of speech treatment for Parkinson’s disease delivered to the home via telerehabilitation: a noninferiority randomized controlled trial. Am J Speech Lang Pathol 25(2):214–232
Baets J, Deconinck T, Smets K et al (2010) Mutations in SACS cause atypical and late-onset forms of ARSACS. Neurology 75(13):1181–1188
Schmidt J, Holas M, Halvorson K, Reding M (1994) Videofluoroscopic evidence of aspiration predicts pneumonia and death but not dehydration following stroke. Dysphagia 9(1):7–11
Vogel AP, Brown SE, Folker JE, Corben LA, Delatycki MB (2014) Dysphagia and swallowing related quality of life in Friedreich ataxia. J Neurol 261(2):392–399
Leow LP, Huckabee M-L, Anderson T, Beckert L (2010) The impact of dysphagia on quality of life in ageing and Parkinson’s disease as measured by the swallowing quality of life (SWAL-QOL) questionnaire. Dysphagia 25(3):216–220
Vogel AP, Folker JE, Poole ML (2014) Treatment for speech disorder in Friedreich ataxia and other hereditary ataxia syndromes. Cochrane Database Syst Rev 10:CD008953
Vogel AP, Keage MJ, Johansson K, Schalling E. Treatment for dysphagia (swallowing difficulties) in hereditary ataxia. Cochrane Database Syst Rev 2015(11):CD010169
Acknowledgements
This study was supported by the Ataxia Charlevoix–Saguenay Foundation and from the European Union’s Horizon 2020 research and innovation program under the ERA-NET Cofund action N° 643578. It was supported by the BMBF (01GM1607 to M. S.), under the frame of the E-Rare-3 network PREPARE (to M. S. and C. G.). A. P. V. receives salaried support from the National Health and Medical Research Council, Australia (Career Development Fellowship ID 1082910), received funding from the Alexander von Humboldt Foundation.
Funding
A/Prof Vogel is chief science officer of Redenlab who aided the acoustic analysis. He also receives institutional support from The University of Melbourne. Ms. Rommel, Ms. Stoll, Ms. Kraus, Mr. Oettinger, Dr. Gagnon, Prof. Horger, Dr. Krumm all have no conflict of interest.
Author information
Authors and Affiliations
Contributions
Prof. APV contributed to the design of the study, collection, analysis and interpretation of the data, and drafting the manuscript. He also supervised students, led the research team, and obtained funding for the research. Ms. NR contributed to the design of the study, collected data, analysis and interpretation of the data, revising the manuscript for intellectual content, and supervision of students. Mr. AO contributed to data analysis and interpretation, and revising the manuscript for intellectual content. Ms. LHS contributed to data analysis and interpretation, and revising the manuscript for intellectual content. Ms. EK contributed to data analysis and interpretation, and revising the manuscript for intellectual content. Dr. CG contributed to data analysis and interpretation, and revising the manuscript for intellectual content. Prof. MH and Dr. PK contributed to administering and interpreting the VFSS and revising the manuscript for intellectual content. Prof. DT contributed to patient recruitment and examination, data interpretation and revising the manuscript for intellectual content. Prof. Dr. LS and Prof. ES contributed to data interpretation and revising the manuscript for intellectual content. Dr. MS contributed to the design of the study, collection, analysis and interpretation of the data, and revising the manuscript for intellectual content. He also supervised students, led the research team, and obtained funding for the research.
Corresponding author
Ethics declarations
Conflicts of interest
Prof. Timmann receives funding from the German Research Foundation (DFG), the Mercator Research Center Ruhr and the German Heredoataxia Foundation unrelated to this study. Prof. Storey receives funding from the NIH, unrelated to this study. Prof. Dr. Schöls receives funding from the German Research Foundation (DFG), the European Union and the German Hereditary Spastic Paraplegia Foundation unrelated to this study. Dr. Synofzik received honoraria from Actelion pharmaceuticals, unrelated to the current study.
Ethical standards
The study received institutional approval from the Medical Ethics Board, University Hospital Tübingen, Germany (Az. 003/2015BO2) and The University of Melbourne Human Research Ethics Committee. All patients, or representatives, provided written informed consent. The project was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vogel, A.P., Rommel, N., Oettinger, A. et al. Coordination and timing deficits in speech and swallowing in autosomal recessive spastic ataxia of Charlevoix–Saguenay (ARSACS). J Neurol 265, 2060–2070 (2018). https://doi.org/10.1007/s00415-018-8950-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-8950-4