Abstract
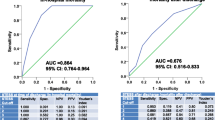
Prediction of mortality, functional outcome and recovery after status epilepticus (SE) is a challenge. Biological and clinical markers have been proposed to reflect the brain injury or to monitor critical ill patients’ severity. The aim of this study was to characterize short-term and long-term prognostic factors for SE patients hospitalized in intensive care unit. Patient’s outcome was assessed using the modified Rankin Scale at discharge and after 6–12 months. We first assessed the univariate prognosis significance of 51 clinical, demographic or biochemical markers. Next, we built multivariate clinico-biological models by combining most important factors. Statistical models’ performances were compared to those of two previous published scales STESS and mSTESS. Eighty-one patients were enrolled. Thirty-five patients showed a steady state while 46 patients clinically worsened at discharge: 14 died, 14 had persistent disability at 6–12 months and 18 recovered. Logistic regression analysis revealed that clinical markers (SE refractoriness, SE duration, de novo SE) were significant independent predictors of worsening while lipids markers and progranulin better predicted mortality. The association of clinico-biological variables allowed to accurately predict worsening at discharge (AUC > 0.72), mortality at discharge (AUC 0.83) and recovery at long-term (AUC 0.89). Previous scales provided lower prediction for worsening (AUC 0.63, STESS; 0.53, mSTESS) and mortality (AUC 0.56, STESS; 0.62, mSTESS) (p < 0.001). We proposed new clinico-biological models with a strong discrimination power for prediction of short- and long-term outcome of hospitalized status epilepticus patients. Their implementation in electronic devices may enhance their clinical liability.


Similar content being viewed by others
Availability of data and material
All data are available on request upon the corresponding author.
Code availability
The codes are available on request upon the corresponding author.
Abbreviations
- AUC:
-
Area under the receiver operating characteristic curve
- CSF:
-
Cerebrospinal fluid
- FC:
-
Free cholesterol
- ICU:
-
Intensive care unit
- ML:
-
Machine learning
- mRS:
-
Modified Rankin score
- NORSE:
-
New-onset refractory status epilepticus
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- RSE:
-
Refractory status epilepticus
- S100B:
-
S100-beta protein
- SE:
-
Status epilepticus
- SVM:
-
Support vector machine
References
Trinka E, Kälviäinen R (2017) 25 years of advances in the definition, classification and treatment of status epilepticus. Seizure 44:65–73. https://doi.org/10.1016/j.seizure.2016.11.001
Leitinger M, Trinka E, Giovannini G et al (2019) Epidemiology of status epilepticus in adults: a population-based study on incidence, causes, and outcomes. Epilepsia 60:53–62. https://doi.org/10.1111/epi.14607
Alkhachroum A, Der-Nigoghossian CA, Rubinos C, Claassen J (2020) Markers in status epilepticus prognosis. J Clin Neurophysiol 37:422–428. https://doi.org/10.1097/WNP.0000000000000761
Kantanen A-M, Reinikainen M, Parviainen I, Kälviäinen R (2017) Long-term outcome of refractory status epilepticus in adults: a retrospective population-based study. Epilepsy Res 133:13–21. https://doi.org/10.1016/j.eplepsyres.2017.03.009
Rossetti AO, Logroscino G, Bromfield EB (2006) A clinical score for prognosis of status epilepticus in adults. Neurology 66:1736–1738. https://doi.org/10.1212/01.wnl.0000223352.71621.97
González-Cuevas M, Santamarina E, Toledo M et al (2016) A new clinical score for the prognosis of status epilepticus in adults. Eur J Neurol 23:1534–1540. https://doi.org/10.1111/ene.13073
Gao Q, Ou-Yang T, Sun X et al (2016) Prediction of functional outcome in patients with convulsive status epilepticus: the END-IT score. Crit Care 20:46. https://doi.org/10.1186/s13054-016-1221-9
Leitinger M, Höller Y, Kalss G et al (2015) Epidemiology-based mortality score in status epilepticus (EMSE). Neurocrit Care 22:273–282. https://doi.org/10.1007/s12028-014-0080-y
Yuan F, Gao Q, Jiang W (2018) Prognostic scores in status epilepticus-a critical appraisal. Epilepsia 59(Suppl 2):170–175. https://doi.org/10.1111/epi.14483
Rossetti AO, Logroscino G, Milligan TA et al (2008) Status Epilepticus Severity Score (STESS): a tool to orient early treatment strategy. J Neurol 255:1561–1566. https://doi.org/10.1007/s00415-008-0989-1
Madžar D, Geyer A, Knappe RU et al (2016) Association of seizure duration and outcome in refractory status epilepticus. J Neurol 263:485–491. https://doi.org/10.1007/s00415-015-7992-0
Kang BS, Kim DW, Kim KK et al (2016) Prediction of mortality and functional outcome from status epilepticus and independent external validation of STESS and EMSE scores. Crit Care 20:25. https://doi.org/10.1186/s13054-016-1190-z
Ciurans J, Grau-López L, Jiménez M et al (2018) Refractory status epilepticus: Impact of baseline comorbidity and usefulness of STESS and EMSE scoring systems in predicting mortality and functional outcome. Seizure 56:98–103. https://doi.org/10.1016/j.seizure.2018.02.007
Giovannini G, Monti G, Tondelli M et al (2017) Mortality, morbidity and refractoriness prediction in status epilepticus: comparison of STESS and EMSE scores. Seizure 46:31–37. https://doi.org/10.1016/j.seizure.2017.01.004
Chaudhry F, Hunt RJ, Hariharan P et al (2020) Machine learning applications in the neuro ICU: a solution to big data mayhem? Front Neurol 11:554633. https://doi.org/10.3389/fneur.2020.554633
von Elm E, Altman DG, Egger M et al (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 4:e296. https://doi.org/10.1371/journal.pmed.0040296
DeGiorgio CM, Correale JD, Gott PS et al (1995) Serum neuron-specific enolase in human status epilepticus. Neurology 45:1134–1137
DeGiorgio CM, Heck CN, Rabinowicz AL et al (1999) Serum neuron-specific enolase in the major subtypes of status epilepticus. Neurology 52:746–749
Hanin A, Baudin P, Demeret S et al (2021) Disturbances of brain cholesterol metabolism: a new excitotoxic process associated with status epilepticus. Neurobiol Dis 154:105346. https://doi.org/10.1016/j.nbd.2021.105346
Trinka E, Cock H, Hesdorffer D et al (2015) A definition and classification of status epilepticus—report of the ILAE task force on classification of status epilepticus. Epilepsia 56:1515–1523. https://doi.org/10.1111/epi.13121
Hirsch LJ, Gaspard N, van Baalen A et al (2018) Proposed consensus definitions for new-onset refractory status epilepticus (NORSE), febrile infection-related epilepsy syndrome (FIRES), and related conditions. Epilepsia 59:739–744. https://doi.org/10.1111/epi.14016
Wu YW, Shek DW, Garcia PA et al (2002) Incidence and mortality of generalized convulsive status epilepticus in California. Neurology 58:1070–1076. https://doi.org/10.1212/wnl.58.7.1070
Hanin A, Denis JA, Frazzini V et al (2022) Neuron Specific Enolase, S100-beta protein and progranulin as diagnostic biomarkers of status epilepticus. J Neurol. https://doi.org/10.1007/s00415-022-11004-2
Hanin A, Demeret S, Denis JA et al (2021) Serum neuron-specific enolase: a new tool for seizure risk monitoring after status epilepticus. Eur J Neurol. https://doi.org/10.1111/ene.15154
Hanin A, Lambrecq V, Denis JA et al (2020) Cerebrospinal fluid and blood biomarkers of status epilepticus. Epilepsia 61:6–18. https://doi.org/10.1111/epi.16405
DeGiorgio CM, Gott PS, Rabinowicz AL et al (1996) Neuron-specific enolase, a marker of acute neuronal injury, is increased in complex partial status epilepticus. Epilepsia 37:606–609
Correale J, Rabinowicz AL, Heck CN et al (1998) Status epilepticus increases CSF levels of neuron-specific enolase and alters the blood-brain barrier. Neurology 50:1388–1391
Freund Y, Bloom B, Bokobza J et al (2015) Predictive value of S100-B and copeptin for outcomes following seizure: the BISTRO international cohort study. PLoS ONE 10:e0122405. https://doi.org/10.1371/journal.pone.0122405
Zhu S, Tai C, Petkau TL et al (2013) Progranulin promotes activation of microglia/macrophage after pilocarpine-induced status epilepticus. Brain Res 1530:54–65. https://doi.org/10.1016/j.brainres.2013.07.023
Sen J, Belli A (2007) S100B in neuropathologic states: the CRP of the brain? J Neurosci Res 85:1373–1380. https://doi.org/10.1002/jnr.21211
Chali F, Djelti F, Eugene E et al (2015) Inhibiting cholesterol degradation induces neuronal sclerosis and epileptic activity in mouse hippocampus. Eur J Neurosci 41:1345–1355. https://doi.org/10.1111/ejn.12911
Chali F, Milior G, Marty S et al (2019) Lipid markers and related transcripts during excitotoxic neurodegeneration in kainate-treated mice. Eur J Neurosci 50:1759–1778. https://doi.org/10.1111/ejn.14375
Bateman RM, Sharpe MD, Jagger JE et al (2016) 36th international symposium on intensive care and emergency medicine: Brussels, Belgium, 15–18 March 2016. Crit Care 20:94. https://doi.org/10.1186/s13054-016-1208-6
Hifumi T, Nakamura K, Kuroda Y et al (2021) High early phase hemoglobin level is associated with favorable neurological outcome in patients with severe traumatic brain injury. Am J Emerg Med 44:373–377. https://doi.org/10.1016/j.ajem.2020.04.065
Lan P, Wang S-J, Shi Q-C et al (2018) Comparison of the predictive value of scoring systems on the prognosis of cirrhotic patients with suspected infection. Medicine (Baltimore) 97:e11421. https://doi.org/10.1097/MD.0000000000011421
Lv Z, Wang W, Qiao B et al (2021) The prognostic value of general laboratory testing in patients with COVID-19. J Clin Lab Anal 35:e23668. https://doi.org/10.1002/jcla.23668
Sonneville R, Mariotte E, Neuville M et al (2016) Early-onset status epilepticus in patients with acute encephalitis. Medicine (Baltimore) 95:e4092. https://doi.org/10.1097/MD.0000000000004092
Madžar D, Reindl C, Mrochen A et al (2021) Value of initial C-reactive protein levels in status epilepticus outcome prediction. Epilepsia 62:e48–e52. https://doi.org/10.1111/epi.16842
Bruno A, Shah N, Lin C et al (2010) Improving modified Rankin Scale assessment with a simplified questionnaire. Stroke 41:1048–1050. https://doi.org/10.1161/STROKEAHA.109.571562
Noble WS (2006) What is a support vector machine? Nat Biotechnol 24:1565–1567
Ojala M, Garriga G (2010) Permutation tests for studying classifier performance. J Mach Learn Res 11:1833–1863
Saito T, Rehmsmeier M (2015) The precision-recall plot is more informative than the ROC plot when evaluating binary classifiers on imbalanced datasets. PLoS ONE 10:e0118432. https://doi.org/10.1371/journal.pone.0118432
Marawar R, Basha M, Mahulikar A et al (2018) Updates in refractory status epilepticus. Crit Care Res Pract 2018:9768949. https://doi.org/10.1155/2018/9768949
Adibhatla RM, Hatcher JF (2008) Altered lipid metabolism in brain injury and disorders. Subcell Biochem 49:241–268. https://doi.org/10.1007/978-1-4020-8831-5_9
Maxfield FR, Tabas I (2005) Role of cholesterol and lipid organization in disease. Nature 438:612–621. https://doi.org/10.1038/nature04399
Gaspard N, Hirsch LJ, Sculier C et al (2018) New-onset refractory status epilepticus (NORSE) and febrile infection-related epilepsy syndrome (FIRES): state of the art and perspectives. Epilepsia 59:745–752. https://doi.org/10.1111/epi.14022
Gaspard N, Foreman BP, Alvarez V et al (2015) New-onset refractory status epilepticus: etiology, clinical features, and outcome. Neurology 85:1604–1613. https://doi.org/10.1212/WNL.0000000000001940
Sutter R, Kaplan PW, Rüegg S (2013) Independent external validation of the status epilepticus severity score. Crit Care Med 41:e475-479. https://doi.org/10.1097/CCM.0b013e31829eca06
Pacha MS, Orellana L, Silva E et al (2016) Role of EMSE and STESS scores in the outcome evaluation of status epilepticus. Epilepsy Behav 64:140–142. https://doi.org/10.1016/j.yebeh.2016.09.036
Hutson M (2018) Artificial intelligence faces reproducibility crisis. Science 359:725–726. https://doi.org/10.1126/science.359.6377.725
The Lancet Respiratory Medicine (2018) Opening the black box of machine learning. Lancet Respir Med 6:801. https://doi.org/10.1016/S2213-2600(18)30425-9
Snodgrass SM, Tsuburaya K, Ajmone-Marsan C (1989) Clinical significance of periodic lateralized epileptiform discharges: relationship with status epilepticus. J Clin Neurophysiol 6:159–172. https://doi.org/10.1097/00004691-198904000-00003
Trinka E, Leitinger M (2022) Management of status epilepticus, refractory status epilepticus, and super-refractory status epilepticus. Continuum (Minneap Minn) 28:559–602. https://doi.org/10.1212/CON.0000000000001103
Acknowledgements
We thank Marion Houot (Sorbonne Université, Institut du Cerveau – Paris Brain Institute – ICM, Pitié-Salpêtrière Hospital) for her advices for statistical analysis.
Funding
This work received support from the “Investissements d’avenir” program ANR-10-IAIHU-06, from the “Fondation pour la Recherche Médicale” (FDM20170839111) and from the Fondation Assitance Publique-Hôpitaux de Paris (EPIRES- Marie Laure PLV Merchandising).
Author information
Authors and Affiliations
Contributions
Conception and design of the study: AH, MC, VN. Acquisition and analysis of data: AH, SD, VL, BR, CM, MB, AD, RB, JAD, FIB, FL, BR, DBR, MC, VN. Drafting a significant portion of the manuscript or figures: AH, SD, VL, BR, CM, MB, AD, JLB, RB, JAD, FIB, FL, BR, DBR, MC, VN. Statistical analysis: AH, MC. Study supervision: SD, DBR, MC, VN.
Corresponding author
Ethics declarations
Conflicts of interest
AH, SD, MC and VN have a patent pending related to the current research. VN reports personal fees from UCB Pharma, EISAI, GW Pharma and LivaNova, outside the submitted work. AD reports grants, personal fees and non-financial support from Philips and Lungpacer, personal fees from Baxter, Getinge, Lowenstein and Gilead, personal fees and non-financial support from Fisher & Paykel and Respinor and grants from French Ministry of Health, outside the submitted work. SD reports individual payment from UCB Pharma, Regeneron and ARGENX. The other authors report no disclosures related to the current research.
Ethics approval
The protocol was approved by our local (2012, CPP Paris-VI) and by the INSERM ethic committees (C16-16, 20152482). The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
Patients or relatives were informed and give their consent.
Consent for publication
Patients or relatives were informed and give their consent.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hanin, A., Demeret, S., Lambrecq, V. et al. Clinico-biological markers for the prognosis of status epilepticus in adults. J Neurol 269, 5868–5882 (2022). https://doi.org/10.1007/s00415-022-11199-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11199-4