Abstract
Purpose
Ocular hypotony secondary to proliferative vitreoretinopathy-related retinal detachment, trauma or inflammation is difficult to treat. Besides endotamponades such as silicone oil, vitreous implants such as iris diaphragms or balloons have been developed to stabilize the eye and to prevent phthisis of the globe. Vitreous implants tested thus far exhibit a seam at the attachment site of the hemispheres, or micropores. This manuscript reports the development of a seamless silicone balloon implant without micropores, which can be filled with silicone oil and surface-modified to improve its biocompatibility. Developed for intraocular placement in the management of chronic hypotony and phthisis prevention, it may also be suitable for tamponading retinal detachments.
Methods
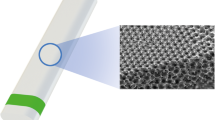
Silicone was used as the basic structure for the fabrication of a seamless balloon-shaped intraocular implant, which was coated by employing a six-arm star-shaped (sP) macromer of a copolymer of 80 % ethylene oxide (EO) and 20 % propylene oxide (PO) with conjugated functional terminal isocyanate groups, NCO-sP(EO-stat-PO), with and without heparin. Three variants of implants, which differ in their surfaces, were manufactured: uncoated silicone, NCO-sP (EO-stat-PO) coated silicone and heparin-NCO-sP (EO-stat-PO) coated silicone implants. To exert a tamponade effect, the implant was filled with silicone oil and its properties were studied.
Results
Seamless thin balloon implants made of silicone, which are considered biocompatible and intrinsically resistant to biological attacks in vivo, could be fabricated in different sizes. The silicone oil-filled implant can mimic the mechanism of buoyant force and high surface tension of silicone oil, which is the only long-term vitreous substitute currently available. The silicone oil-filled implant can also mimic the natural vitreous body by occupying the entire posterior segment.
Conclusions
The intraocular silicone implant as an alternative long-term treatment of chronic ocular hypotony might offer a new option for clinical ophthalmological practice. In vivo studies need to be performed to collect more data on the implant’s long-term mechanical and optical properties, as well as long-term biocompatibility.








Similar content being viewed by others
References
Jonas JB, Vossmerbaeumer U, Kamppeter BA (2004) Chronic prephthisical ocular hypotony treated by intravitreal triamcinolone acetonide. Acta Ophthalmol Scand 825:637
De Smet MD, Gunning F, Feenstra R (2005) The surgical management of chronic hypotony due to uveitis. Eye 191:60–64
Cadera W, Harding PW, Gonder JR, Hooper PL (1993) Management of severe hypotony with intravitreal injection of Healon. Can J Ophthalmol 28(5):236–237
Arevalo JF, Garcia RA, Fernandez CF (2004) Anterior segment inflammation and hypotony after posterior segment surgery. Ophthalmol Clin N Am 17(4):527–537
Kapur R, Birnbaum AD, Goldstein DA, Tessler HH, Shapiro MJ, Ulanski LJ, Blair MP (2010) Treating uveitis-associated hypotony with pars planavitrectomy and silicone oil injection. Retina 30(1):140–145
Küçükerdönmez C, Beutel J, Bartz-Schmidt KU, Gelisken F (2009) Treatment of chronic ocular hypotony with intraocular application of sodium hyaluronate. Br J Ophthalmol 93(2):235–239
Morse LS, McCuen BW (1991) The use of silicone oil in uveitis and hypotony. Retina 11(4):399–404
O’Connell SR, Majji AB, Humayun MS, de Juan E Jr (2000) The surgical management of hypotony. Ophthalmology 107(2):318–323
Pivetti-Pezzi P, Da Dalt S, La Cava M, Pinca M, De Gregorio F, Virno M (2000) Ibopamine treatment in chronic hypotony secondary to long-lasting uveitis. Eur J Ophthalmol 10(4):332–334
Singh K, Byrd S, Egbert PR, Budenz D (1998) Risk of hypotony after primary trabeculectomy with antifibrotic agents in a black West African population. J Glaucoma 7(2):82–85
Tosi GM, Schiff W, Barile G, Yoshida N, Chang S (2005) Management of severe hypotony with intravitreal injection of viseoeplastic. Am J Ophthalmol 140(5):952–954
Schramm C, Spitzer M, Henke-Fahle S, Steinmetz G, Januschowski K, Heiduschka P, Geis-Gerstorfer J, Biedermann T, Bartz-Schmidt K, Szurman P (2012) The cross-linked biopolymer hyaluronic acid as an artificial vitreous substitute. Invest Ophthalmol Vis Sci 2(53(2)):613–621. doi:10.1167/iovs.11-7322
Maruoka S, Matsuura T, Kawasaki K, Okamoto M, Yoshiaki H, Kodama M, Sugiyama M, Annaka M (2006) Biocompatibility of polyvinylalcohol gel as a vitreous substitute. Curr Eye Res 31:599–606
Keller GK, Dahlke C, Kuckelkorn R, Schrage N (2003) Experience with the artificial iris diaphragm in hypotonous eyes. Ophthalmology 100(3):203–208
Glynne GC, Freeman HM, Schepens CL (1970) Vitreous surgery. 3. Intraocular balloon: Instrument Report. Arch Ophthalmol 83:713–714
Tolentino FI, Refojo MF, Liu HS, Schepens CL and Freeman HM (1978) Intravitreous silicone balloon: an experimental study. Ophtalmic Surg. 73–80
Gand H, Paroussis P, Skorpik C (1986) An intraocular balloon for silicone oil implantation. Graefes Arch Exp Clin Ophthalmol 224:18–20
Binder S (1986) Repair of retinl detachments with temporary balloon buckling. Retina 6:210–214
Kreissig I, Failer J, Lincoff H, Ferrari F (1989) Results of temporary balloon buckle in the treatment of 500 retinal detachments and a comparison with pneumatic retinopexy. Am J Ophthalmol 107:381–389
Peng YJ, Lu YT, Liu KS, Liu SJ, Fan L, Huang WC (2012) Biodegradable balloon-expandable self-locking polycaprolactone stents as buckling explants for the treatment of retinal detachment: an in vitro and in vivo study. J Biomed Mater Res A 101(1):167–175. doi:10.1002/jbm.a.34315, 2013 Jan
Liu Y, Jiang Z, Gao Q, Ge J, Chen J, Cao X, Shen Q, Ma P (2010) Technical standards of a foldable capsular vitreous body in terms of mechanical, optical, and biocompatible properties. Artif Organs 34(10):836–845
Lin X, Wang Z, Jiang Z, Long C, Liu Y, Wang P, Jin C, Yi C, Gao Q (2012) Preliminary efficacy and safety of a silicone oil-filled foldable capsular vitreous body in the treatment of severe retinal detachment. Retina 32(4):729–741
Qian-Ying G, Yue F, Yan-Nian H (2015) Vitreous substitutes: challenges and directions. Int J Ophthalmol 18(8 (3)):437–440
Barr S, Hill E, Bayat A (2009) Current implant surface technology: an examination of their nanostructure and their influence on fibroblast alignment and biocompatibility. Eplasty 9:e22
Fischer S, Carstesen D, Klee D, Walter P, Weinberger AW (2012) Surface-modified siliconefoils for intraocular implantation. Graefes Arch Clin Exp Ophthalmol 250(6):823–827
Groll J, Ameringer T, Spatz JP, Moeller M (2005) Ultrahin coatings form isocyanate- terminated star PEG prepolymers: Layer formation and characterization. Langmuir 1(21(5)):1991–1999
Gates DP (2009) Inorganic and organometallic polymers. Annual Rep ProgChem Sec A 105397–415
Jones RG, Andos W, Chojnowski J (eds) (2000) Silicone-containing polymers: The science and technology of their synthesis and applications. Kluwer Academic Publishers, Boston, MA
Colas A, Curtis J (2002) Silicone biomaterials: History and chemistry in biomaterials science: An introduction to materials in medicine, eds Ratner BD, Hoffmann AS, Schoen FJ, and Lemons JE, 80–6. Amsterdam, Elsevier Academic Press
Janovsky EC, Kupper LL, Hulka BS (2000) Meta-analysis of the relation between silicone breast implants and the risk of connective tissue disease. N Engl J Med 342:781–790
Rachal WF, Burton TC (1979) Changing concepts of failure after retinal detachment surgery. Arch Ophthalmol 97:480–483
Ryan SJ (1985) The pathophysiology of proliferative vitreoretinopathy in its management. Am J Ophthalmol 100:188–193
Hauser J, Esenwein SA, Awakowicz P, Steinau HU, Köller M, Halfmann H (2011) Sterilization of heat-sensitive silicone implant material by low-pressure gas plasma. Biomed Instrum Technol 45(1):75–79
Bartzoka V, McDermott MR, Brook MA (1999) Protein-Silicone Interactions. Adv Mater 11(3):257–259
Heyes CD, Groll J, Möller M, Nienhaus GU (2007) Synthesis, patterning and applications of star-shaped poly(ethylene glycol) biofunctionalized surfaces. Mol Biosyst 3(6):419–430
Nagahama K, Saito T, Quchi T, Ohya Y (2010) Biodegradable nano-aggregates of star-shaped 8-arm PEG-PLLA block co-polymers for encapsulation of water-soluble macromolecules. J Biomater Sci Polym Ed 22:407–416
Satulovsky J, Caringano MA, Szleifer I (2000) Kinetic and thermodynamic control of protein adsorption. Proc Natl Acad Sci U S A 1(97(16)):9037–9041
Hoffmann J, Groll J, Heuts J, Rong H, Klee D, Ziemer G, Moeller M, Wendel HP (2006) Blood cell and plasma protein repellent properties of star-PEG-modified surface. J Biomater Sci Polym Ed 17(9):985–996
Cohen Tervaert JW, Kappel RM (2013) Silicone implant incompatibility syndrome (SIIS): A frequent cause of ASIA (Shoenfeld's syndrome). Immunol Res 56(2–3):293–298
Tervaert JW, Stegeman CA, Kallenberg CG (1998) Silicone exposure and vasculitis. Curr Opin Rheumatol 10:12–17
Parks CG, Conrad K, Cooper GS (1999) Occupational exposure to crystalline silica and autoimmune disease. Environ Health Perspect 107(S5):793–802
Jewell M, Spear SL, Largent J, Oefelein MG, Adams WP Jr (2011) Anaplastic large T-cell lymphoma and breast implants: A review of the literature. Plast Reconstr Surg 128:651–661
Acknowledgments
The technical assistance for this research project, from the Interdisciplinary Centre for Clinical Research BIOMAT within the Faculty of Medicine at the RWTH Aachen University, Aachen Center for Technology Transfer in Ophthalmology , Institute for Technical and Macromolecular Chemistry of RWTH Aachen University, is gratefully appreciated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The Interdisciplinary Centre for Clinical Research BIOMAT and the START program, both within the faculty of Medicine at the RWTH Aachen University, provided financial support in the form of grant funding. The sponsor had no role in the design or conduct of this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Bayoudh, W., Frentz, M., Carstesen, D. et al. Intraocular silicone implant to treat chronic ocular hypotony—preliminary feasibility data. Graefes Arch Clin Exp Ophthalmol 254, 2131–2139 (2016). https://doi.org/10.1007/s00417-016-3364-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3364-4