Abstract
Background
Intraocular gas tamponades are an important tool in modern vitreoretinal surgery. However, there is considerable variation in their use and perceptions amongst clinicians regarding these agents.
Methods
An electronic survey of vitreoretinal surgeons in the UK was undertaken to establish the patterns of use and surgeons’ estimates of the longevity and expansion timing of gas tamponades. In addition, data were prospectively collected on the longevity of gas tamponades in 114 patients from our unit. An analysis was performed to identify patient or surgery factors affecting gas longevity
Results
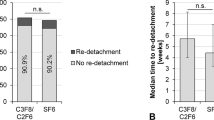
A wide variation in the patterns of use and estimates of longevity and expansion timing of intraocular tamponades was found in the survey of vitreoretinal surgeons. Data from our unit give informed estimates on the longevity of three commonly used tamponades. For 30 % sulphur hexafluoride (SF6), mean 18.0 days, standard deviation (SD) 2.6 days. For 20 % hexafluoroethane (C2F6), mean 34.5 days, SD 3.3 days. For 15 % perfluoropropane (C3F8), mean 67.7 days SD 5.5 days. In the C2F6 group there was correlation between longer duration of the gas bubble and longer axial length (r = 0.438, p = 0.02) and longer gas duration with male sex (p = 0.002).
Conclusions
We present informed gas tamponade longevity figures in clinical practice and report statistically significant associations between longer gas longevity and increasing axial length and male sex.




Similar content being viewed by others
References
Norton EW (1973) Intraocular gas in the management of selected retinal detachments. Trans Am Acad Ophthalmol Otolaryngol 77(2):Op85–Op98
Lincoff H, Coleman J, Kreissig I, Richard G, Chang S, Wilcox LM (1983) The perfluorocarbon gases in the treatment of retinal detachment. Ophthalmology 90(5):546–551
Abrams GW, Swanson DE, Sabates WI, Goldman AI (1982) The results of sulfur hexafluoride gas in vitreous surgery. Am J Ophthalmol 94(2):165–171
Sabates WI, Abrams GW, Swanson DE, Norton EW (1981) The use of intraocular gases. The results of sulfur hexafluoride gas in retinal detachment surgery. Ophthalmology 88(5):447–454
Sigler EJ, Randolph JC, Charles S, Calzada JI (2012) Intravitreal fluorinated gas preference and occurrence of rare ischemic postoperative complications after pars plana vitrectomy: a survey of the american society of retina specialists. J Ophthalmol: 230596
Jackson TL, Donachie PH, Sparrow JM, Johnston RL (2013) United Kingdom National Ophthalmology Database study of vitreoretinal surgery: report 2, macular hole. Ophthalmology 120(3):629–634
Jackson TL, Donachie PH, Sallam A, Sparrow JM, Johnston RL (2014) United Kingdom National Ophthalmology Database study of vitreoretinal surgery: report 3, retinal detachment. Ophthalmology 121(3):643–648
Shunmugam M, Shah AN, Hysi PG, Williamson TH (2014) The pattern and distribution of retinal breaks in eyes with rhegmatogenous retinal detachment. Am J Ophthalmol 157(1):221–226.e1
Williamson TH, Lee E (2014) Idiopathic macular hole: analysis of visual outcomes and the use of indocyanine green or brilliant blue for internal limiting membrane peel. Graefes Arch Clin Exp Ophthalmol 252(3):395–400
Lincoff H, Mardirossian J, Lincoff A, Liggett P, Iwamoto T, Jakobiec F (1980) Intravitreal longevity of three perfluorocarbon gases. Arch Ophthalmol 98(9):1610–1611
Lincoff H, Maisel JM, Lincoff A (1984) Intravitreal disappearance rates of four perfluorocarbon gases. Arch Ophthalmol 102(6):928–929
Lincoff H, Stergiu P, Smith R, Movshovich A (1992) Longevity of expanding gases in vitrectomized eyes. Retina 12(4):364–366
Parver LM, Lincoff H (1978) Mechanics of intraocular gas. Investig Ophthalmol Vis Sci 17(1):77–79
Jacobs PM, Twomey JM, Leaver PK (1988) Behaviour of intraocular gases. Eye (Lond) 2(Pt 6):660–663
Thompson JT (1989) Kinetics of intraocular gases. Disappearance of air, sulfur hexafluoride, and perfluoropropane after pars plana vitrectomy. Arch Ophthalmol 107(5):687–691
Shunmugam M, Shunmugam S, Williamson TH, Laidlaw DA (2011) Air-gas exchange reevaluated: clinically important results of a computer simulation. Invest Ophthalmol Vis Sci 52(11):8262–8265
Geyer O, Silver DM, Mathalon N, Massey AD (2003) Gender and age effects on pulsatile ocular blood flow. Ophthalmic Res 35(5):247–250
Kavroulaki D, Gugleta K, Kochkorov A, Katamay R, Flammer J, Orgul S (2010) Influence of gender and menopausal status on peripheral and choroidal circulation. Acta Ophthalmol 88(8):850–853
Schmidl D, Schmetterer L, Garhofer G, Popa-Cherecheanu A (2015) Gender differences in ocular blood flow. Curr Eye Res 40(2):201–212
Thompson JT (1992) The absorption of mixtures of air and perfluoropropane after pars plana vitrectomy. Arch Ophthalmol 110(11):1594–1597
Hutter J, Luu H, Schroeder L (2002) A biological model of tamponade gases following pneumatic retinopexy. Curr Eye Res 25(4):197–206
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of Interest
AK, AS, and ZS certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript. THW is involved in the following: Bausch and Lomb Insights panel, Software development for Axsys Systems, Glasgow, UK, Invited lectures for Alcon, UK.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kontos, A., Tee, J., Stuart, A. et al. Duration of intraocular gases following vitreoretinal surgery. Graefes Arch Clin Exp Ophthalmol 255, 231–236 (2017). https://doi.org/10.1007/s00417-016-3438-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3438-3