Abstract
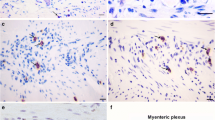
Chagas disease is caused by the parasite, Trypanosoma cruzi that causes chronic cardiac and digestive dysfunction. Megacolon, an irreversible dilation of the left colon, is the main feature of the gastrointestinal form of Chagas disease. Patients have severe constipation, a consequence of enteric neuron degeneration associated with chronic inflammation. Dysmotility, infection, neuronal loss and a chronic exacerbated inflammation, all observed in Chagas disease, can affect enteroendocrine cells (EEC) expression, which in turn, could influence the inflammatory process. In this study, we investigated the distribution and chemical coding of EEC in the dilated and non-dilated portion of T. cruzi-induced megacolon and in non-infected individuals (control colon). Using immunohistochemistry, EECs were identified by applying antibodies to chromogranin A (CgA), glucagon-like peptide 1 (GLP-1), 5-hydroxytryptamine (5-HT), peptide YY (PYY) and somatostatin (SST). Greater numbers of EEC expressing GLP-1 and SST occurred in the dilated portion compared to the non-dilated portion of the same patients with Chagas disease and in control colon, but numbers of 5-HT and PYY EEC were not significantly different. However, it was noticeable that EEC in which 5-HT and PYY were co-expressed were common in control colon, but were rare in the non-dilated and absent in the dilated portion of chagasic megacolon. An increase in the number of CgA immunoreactive EEC in chagasic patients reflected the increases in EEC numbers summarised above. Our data suggests that the denervation and associated chronic inflammation are accompanied by changes in the number and coding of EEC that could contribute to disorders of motility and defence in the chagasic megacolon.




Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
Change history
15 February 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00418-021-01971-4
References
Adad SJ, Cancado CG, Etchebehere RM, Teixeira VP, Gomes UA, Chapadeiro E, Lopes ER (2001) Neuron count reevaluation in the myenteric plexus of chagasic megacolon after morphometric neuron analysis. Virchows Arch 438:254–258. https://doi.org/10.1007/s004280000319
Agersnap M, Rehfeld JF (2014) Measurement of nonsulfated cholecystokinins. Scand J Clin Lab Investig 74(5):424–431
Ahern GP (2011) 5-HT and the immune system. Current Opinion in Pharmacology 11:29–33
Bafutto M, Luquetti AO, Neto SG, Penhavel FAS, Oliveira EC (2017) Constipation is related to small bowel disturbance rather than colonic enlargement in acquired chagasic megacolon. Gastroenterol Res 10:213. https://doi.org/10.14740/gr872w
Baldassano S, Wang G-D, Mulè F, Wood JD (2012) Glucagon-like peptide-1 modulates neurally evoked mucosal chloride secretion in guinea pig small intestine in vitro. Am J Physiol-Gastrointestinal Liv Physiol 302:G352–G358
Benchimol Barbosa PR (2006) The oral transmission of Chagas’ disease: an acute form of infection responsible for regional outbreaks. Int J Cardiol 112:132–133. https://doi.org/10.1016/j.ijcard.2005.11.087
Bermudez R, Vigliano F, Quiroga MI, Nieto JM, Bosi G, Domeneghini C (2007) Immunohistochemical study on the neuroendocrine system of the digestive tract of turbot, Scophthalmus maximus (L.), infected by Enteromyxum scophthalmi (Myxozoa). Fish Shellfish Immunol 22:252–263. https://doi.org/10.1016/j.fsi.2006.05.006
Bern C (2015) Chagas’ disease New England. J Med 373:456–466
Bern C et al (2007) Evaluation and treatment of chagas disease in the United States: a systematic review. JAMA 298:2171–2181. https://doi.org/10.1001/jama.298.18.2171
Brubaker PL, Drucker DJ, Asa SL, Swallow C, Redston M, Greenberg GR (2002) Prolonged gastrointestinal transit in a patient with a glucagon-like peptide (GLP)-1-and-2-producing neuroendocrine tumor. J Clin Endocrinol Metab 87:3078–3083
Chisholm C, Greenberg GR (2002) Somatostatin-28 regulates GLP-1 secretion via somatostatin receptor subtype 5 in rat intestinal cultures. Am J Physiol-Endocrinol Metab 283:E311–E317
Cho H-J, Callaghan B, Bron R, Bravo DM, Furness JB (2014) Identification of enteroendocrine cells that express TRPA1 channels in the mouse intestine. Cell Tissue Res 356(1):77–82
Cho H-J, Kosari S, Hunne B, Callaghan B, Rivera LR, Bravo DM, Furness JB (2015) Differences inhormone localisation patterns of K and L type enteroendocrine cells in the mouse andpig small intestine and colon. Cell Tissue Res 359(2):693–698
Chowers Y, Cahalon L, Lahav M, Schor H, Tal R, Bar-Meir S, Levite M (2000) Somatostatin through its specific receptor inhibits spontaneous and TNF-α-and bacteria-induced IL-8 and IL-1β secretion from intestinal epithelial cells. J Immunol 165:2955–2961
Coates MD et al (2004) Molecular defects in mucosal serotonin content and decreased serotonin reuptake transporter in ulcerative colitis and irritable bowel syndrome. Gastroenterology 126:1657–1664
Coleman NS et al (2006) Abnormalities of serotonin metabolism and their relation to symptoms in untreated celiac disease. Clin Gastroenterol Hepatol 4:874–881
Costedio MM, Coates MD, Danielson AB, Buttolph TR, Blaszyk HJ, Mawe GM, Hyman NH (2008) Serotonin signaling in diverticular disease. J Gastrointestinal Surg 12:1439
da Silveira AB et al (2007a) Neurochemical coding of the enteric nervous system in chagasic patients with megacolon. Dig Dis Sci 52:2877–2883. https://doi.org/10.1007/s10620-006-9680-5
da Silveira AB, Lemos EM, Adad SJ, Correa-Oliveira R, Furness JB, D’Avila Reis D (2007b) Megacolon in Chagas disease: a study of inflammatory cells, enteric nerves, and glial cells. Hum Pathol 38:1256–1264. https://doi.org/10.1016/j.humpath.2007.01.020
de Freitas M, de Oliveira E, de Oliveira F, Jabari S, Brehmer A, da Silveira A (2015) Is the increased presence of CD 8 T-lymphocytes related to serotonin levels in C hagas disease? Colorectal Dis 17:268–269
De Jonge F et al (2003) Effects of Schistosoma mansoni infection on somatostatin and somatostatin receptor 2A expression in mouse ileum. Neurogastroenterol Motil 15:149–159. https://doi.org/10.1046/j.1365-2982.2003.00400.x
de Oliveira JA, Freitas MAR, de Oliveira EC, Jabari S, Brehmer A, da Silveira ABM (2019) 5-HT3A serotonin receptor in the gastrointestinal tract: the link between immune system and enteric nervous system in the digestive form of Chagas disease. Parasitol Res 118:1325–1329. https://doi.org/10.1007/s00436-019-06241-w
Di Sabatino A et al (2014) Increase in neuroendocrine cells in the duodenal mucosa of patients with refractory celiac disease. Am J Gastroenterol 109:258–269
Dias JC, Silveira AC, Schofield CJ (2002) The impact of Chagas disease control in Latin America: a review. Mem Inst Oswaldo Cruz 97:603–612. https://doi.org/10.1590/s0074-02762002000500002
Duhamel B (1956) Une nouvelle operation pour le megacôlon congenital: L’abaissement retrocecal et trans-anal du côlon et son application posible au traitement de quelques malformations. Press Med 95:2249–2250
El-Salhy M, Gundersen D (2015) Diet in irritable bowel syndrome. Nutr J 14:36. https://doi.org/10.1186/s12937-015-0022-3
El-Salhy M, Gundersen D, Østgaard H, Lomholt-Beck B, Hatlebakk JG, Hausken T (2012) Low densities of serotonin and peptide YY cells in the colon of patients with irritable bowel syndrome. Dig Dis Sci 57:873–878
Everard A, Cani PD (2014) Gut microbiota and GLP-1. Reviews in Endocrine and Metabolic Disorders 15:189–196
Facer P, Bishop AE, Lloyd RV, Wilson BS, Hennessy RJ, Polak JM (1985) Chromogranin: a newly recognized marker for endocrine cells of the human gastrointestinal tract. Gastroenterology 89:1366–1373. https://doi.org/10.1016/0016-5085(85)90657-2
Freitas M, Segatto N, Tischler N, de Oliveira E, Brehmer A, da Silveira A (2017) Relation between mast cells concentration and serotonin expression in chagasic megacolon development. Parasite Immunol 39:e12414. https://doi.org/10.1111/pim.12414
Furness JB, Rivera LR, Cho H-J, Bravo DM, Callaghan B (2013) The Gut as a Sensory Organ Nature reviews. Gastroenterol Hepatol 10:729. https://doi.org/10.1038/nrgastro.2013.180
Gattuso J, Kamm M, Talbot I (1997) Pathology of idiopathic megarectum and megacolon. Gut 41:252–257
Gershon MD (2013) 5-Hydroxytryptamine (serotonin) in the gastrointestinal tract. Curr Opin Endocrinol Diabetes Obes 20:14
Hansen L, Hartmann B, Bisgaard T, Mineo H, Jørgensen PN, Holst JJ (2000) Somatostatin restrains the secretion of glucagon-like peptide-1 and-2 from isolated perfused porcine ileum. Am J Physiol-Endocrinol Metab 278:E1010–E1018
Harrison E, Lal S, McLaughlin JT (2013) Enteroendocrine cells in gastrointestinal pathophysiology. Curr Opin Pharmacol 13:941–945. https://doi.org/10.1016/j.coph.2013.09.012
Helyes Z et al (2001) Anti-inflammatory effect of synthetic somatostatin analogues in the rat. Br J Pharmacol 134:1571–1579
Husted AS, Trauelsen M, Rudenko O, Hjorth SA, Schwartz TW (2017) GPCR-mediated signaling of metabolites. Cell Metab 25:777–796. https://doi.org/10.1016/j.cmet.2017.03.008
Jabari S, da Silveira AB, de Oliveira EC, Neto SG, Quint K, Neuhuber W, Brehmer A (2011) Partial, selective survival of nitrergic neurons in chagasic megacolon. Histochem Cell Biol 135:47–57
Jabari S, da Silveira A, de Oliveira E, Quint K, Wirries A, Neuhuber W, Brehmer A (2013) Interstitial cells of C ajal: crucial for the development of megacolon in human C hagas’ disease? Colorectal Dis 15:e592–e598
Jabari S, da Silveira AB, de Oliveira EC, Quint K, Wirries A, Neuhuber W, Brehmer A (2014a) Mucosal layers and related nerve fibres in non-chagasic and chagasic human colon–a quantitative immunohistochemical study. Cell Tissue Res 358:75–83. https://doi.org/10.1007/s00441-014-1934-5
Jabari S, de Oliveira EC, Brehmer A, da Silveira AB (2014b) Chagasic megacolon: enteric neurons and related structures. Histochem Cell Biol 142:235–244
Kovacs T, Walsh J, Maxwell V, Wong H, Azuma T, Katt E (1989) Gastrin is a major mediator of the gastric phase of acid secretion in dogs: proof by monoclonal antibody neutralization. Gastroenterology 97(6):1406–1413
Kannen V et al (2018) Mast cells and serotonin synthesis modulate Chagas disease in the colon: clinical and experimental evidence. Dig Dis Sci 63:1473–1484
Köberle F (1968) Chagas' Disease and Chagas' syndromes: the pathology of American trypanosomiasis. In: Advances in parasitology, vol 6. Elsevier, pp 63–116. https://doi.org/https://doi.org/10.1016/S0065-308X(08)60472-8
Latorre R, Sternini C, De Giorgio R, Greenwood-Van Meerveld B (2016) Enteroendocrine cells: a review of their role in brain-gut communication. Neurogastroenterol Motil 28:620–630. https://doi.org/10.1111/nmo.12754
Leventhal A, Gimmon Z (1978) Toxic idiopathic megacolon: fatal outcome in a mentally retarded adolescent. Dis Colon Rectum 21:383–386
Lincoln J, Crowe R, Kamm M, Burnstock G, Lennard-Jones J (1990) Serotonin and 5-hydroxyindoleacetic acid are increased in the sigmoid colon in severe idiopathic constipation. Gastroenterology 98:1219–1225
Lindop G (1983) Enterochromaffin cell hyperplasia and megacolon: report of a case. Gut 24:575–578
Lopes ER, Rocha A, Meneses AC, Lopes MA, Fatureto MC Lopes GP, Chapadeiro E (1989) Prevalence of visceromegalies in necropsies carried out in Triangulo Mineiro from 1954 to 1988. Rev Soc Bras Med Trop 22:211–215. https://doi.org/10.1590/s0037-86821989000400008
Lund ML, Egerod KL, Engelstoft MS, Dmytriyeva O, Theodorsson E, Patel BA, Schwartz TW (2018) Enterochromaffin 5-HT cells—a major target for GLP-1 and gut microbial metabolites. Mol Metab 11:70–83. https://doi.org/10.1016/j.molmet.2018.03.004
Maniero VC et al (2007) IFNG? 874T/A polymorphism is not associated with American tegumentary leishmaniasis susceptibility but can influence Leishmania induced IFN-gamma production. BMC Infect Dis 7:33 Misch. https://doi.org/10.1186/1471-2334-7-33
Martins P et al (2017) Analysis of enteroendocrine cell populations in the human colon. Cell Tissue Res 367:161–168. https://doi.org/10.1007/s00441-016-2530-7
Martins PR, Nascimento RD, dos Santos AT, de Oliveira EC, Martinelli PM (2018) Reis DdA Mast cell-nerve interaction in the colon of Trypanosoma cruzi-infected individuals with chagasic megacolon. Parasitol Res 117:1147–1158
Martins PR et al (2015) Mast cells in the colon of Trypanosoma cruzi-infected patients: are they involved in the recruitment, survival and/or activation of eosinophils? Parasitol Res 114:1847–1856
McCall L-I, Tripathi A, Vargas F, Knight R, Dorrestein PC, Siqueira-Neto JL (2018) Experimental Chagas disease-induced perturbations of the fecal microbiome and metabolome. PLoS Neglected Tropical Dis 12:e0006344
Meier-Ruge WA, Müller-Lobeck H, Stoss F, Bruder E (2006) The pathogenesis of idiopathic megacolon. European J Gastroenterol Hepatol 18:1209–1215
Meneghelli UG, Macedo J, Troncon L, Dantas R (1982) Basal motility of dilated and non-dilated sigmoid colon and rectum in Chagas’ disease. Arquivos de Gastroenterol 19:127–132
Neurauter G, Schrocksnadel K, Scholl-Burgi S, Sperner-Unterweger B, Schubert C, Ledochowski M, Fuchs D (2008) Chronic immune stimulation correlates with reduced phenylalanine turnover. Curr Drug Metab 9:622–627
Ng QX, Soh AYS, Loke W, Lim DY, Yeo WS (2018) The role of inflammation in irritable bowel syndrome (IBS). J Inflamm Res 11:345–349. https://doi.org/10.2147/JIR.S174982
Ohkusa T, Koido S, Nishikawa Y, Sato N (2019) Gut microbiota and chronic constipation: a review and update. Frontiers in medicine 6. https://doi.org/10.3389/fmed.2019.00019
Oxenkrug G (2011) Interferon-gamma—inducible inflammation: contribution to aging and aging-associated psychiatric disorders. Aging Dis 2:474–486
Patterson M, Murphy KG, le Roux CW, Ghatei MA, Bloom SR (2005) Characterization of ghrelinlikeimmunoreactivity in human plasma. J Clin Endocrinol Metabolism 90(4):2205–2211
Peeters T, Janssens J, Vantrappen G (1983) Somatostatin and the interdigestive migrating motor complex in man. Regul Pept 5:209–217
Perez-Ayala A, Perez-Molina JA, Norman F, Monge-Maillo B, Faro MV, Lopez-Velez R (2011) Gastro-intestinal Chagas disease in migrants to Spain: prevalence and methods for early diagnosis. Ann Trop Med Parasitol 105:25–29. https://doi.org/10.1179/136485910X12851868780423
Pinto J-J et al (2019) Characterization of digestive disorders of patients with chronic Chagas disease in Cochabamba, Bolivia. Heliyon 5:e01206
Raybould HE (2010) Gut chemosensing: interactions between gut endocrine cells and visceral afferents. Autonomic Neuroscience 153:41–46
Rehfeld JF (1998) Accurate measurement of cholecystokinin in plasma. Clin Chem 44(5):991–1001
Ribeiro U Jr, Safatle-Ribeiro AV, Habr-Gama A, Gama-Rodrigues JJ, Sohn J, Reynolds JC (1998) Effect of Chagas’ disease on nitric oxide-containing neurons in severely affected and unaffected intestine. Dis Colon Rectum 41:1411–1417. https://doi.org/10.1007/bf02237058
Robello C et al (2019) The fecal, oral, and skin microbiota of children with Chagas disease treated with benznidazole. PLoS one. https://doi.org/10.1371/journal.pone.0212593
Rogawski MA, Goodrich J, Gershon M, Touloukian R (1978) Hirschsprung’s disease: absence of serotonergic neurons in the aganglionic colon. J Pediatr Surg 13:608–615
Rowlands J, Heng J, Newsholme P, Carlessi R (2018) Pleiotropic effects of GLP-1 and analogs on cell signaling, metabolism, and function. Front Endocrinol 9 doi:https://doi.org/10.3389/fendo.2018.00672
Santos S, Barcelos I, Mesquita M (2000) Total and segmental colonic transit time in constipated patients with Chagas disease without megaesophagus or megacolon. Braz J Med Biol Res 33:43–49
Sei Y et al (2018) Mature enteroendocrine cells contribute to basal and pathological stem cell dynamics in the small intestine. Am J Physiol Gastrointest Liver Physiol 315:G495–g510. https://doi.org/10.1152/ajpgi.00036.2018
Shulkes A, Fletcher D, Hardy K (1983) Organ and plasma metabolism of neurotensin in sheep. Am J Physiol Endocrinol Metab 245(5):E457–E462
Soeda J, O’Briain DS, Puri P (1993) Regional reduction in intestinal neuroendocrine cell populations in enterocolitis complicating Hirschsprung’s disease. J Pediatr Surg 28:1063–1068
Spiller R, Jenkins D, Thornley J, Hebden J, Wright T, Skinner M, Neal K (2000) Increased rectal mucosal enteroendocrine cells T lymphocytes, and increased gut permeability following acutecampylobacter enteritis and in post-dysenteric irritable bowel syndrome. Gut 47:804–811. https://doi.org/10.1136/gut.47.6.804
Stoyanova II, Gulubova MV (2002) Mast cells and inflammatory mediators in chronic ulcerative colitis. Acta Histochem 104:185–192. https://doi.org/10.1078/0065-1281-00641
Tolessa T, Gutniak M, Holst JJ, Efendic S, Hellström PM (1998) Inhibitory effect of glucagon-like peptide-1 on small bowel motility. Fasting but not fed motility inhibited via nitric oxide independently of insulin and somatostatin. J Clin Invest 102:764–774
Torres OA, Calzada JE, Beraún Y, Morillo CA, González A, González CI, Martín J (2010) Role of the IFNG+ 874T/A polymorphism in Chagas disease in a Colombian population Infection. Genet Evol 10:682–685. https://doi.org/10.1016/j.meegid.2010.03.009
Van Der Wielen N et al (2014) Cross-species comparison of genes related to nutrient sensing mechanisms expressed along the intestine. PLoS One 9:e107531
Vezzadini C, Toni R, Vezzadini P (1996) Pancreatic somatostatinoma presenting with chronic intestinal pseudo-obstruction syndrome. Minerva Gastroenterol e Dietol 42:227–231
Voss U, Sand E, Hellström PM, Ekblad E (2012) Glucagon-like peptides 1 and 2 and vasoactive intestinal peptide are neuroprotective on cultured and mast cell co-cultured rat myenteric neurons. BMC gastroenterology 12:30
Wang R et al (2018) Gut microbiota play an essential role in the antidiabetic effects of rhein. Evid Based Complement Alternat Med 2018:609328. https://doi.org/10.1155/2018/6093282
Worthington JJ, Reimann F, Gribble F (2018) Enteroendocrine cells-sensory sentinels of the intestinal environment and orchestrators of mucosal immunity. Mucosal Immunol 11:3–20
Yanaihara N, Yanaihara C, Nagai K, Sato H, Shimizu F, Yamaguchi K, Abe K (1980) Motilin-like immunoreactivity in porcine, canine, human and rat tissues. Biomedical Research 1(1):76–83
Yusta B et al (2015) GLP-1R agonists modulate enteric immune responses through the intestinal intraepithelial lymphocyte GLP-1R. Diabetes 64:2537–2549
Funding
This study was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee of the Federal University of Minas Gerais, number: 04939212.9.0000.5149.
Consent to participate
Informed consent was obtained from the patients before tissue procurement. The colon specimens were obtained in clinically indicated surgeries. When the current study was performed, all diagnostic procedures were completed, and the patients’ data were anonymized.
Consent for publication
All authors have read the manuscript and agree to its publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martins, P.R., Fakhry, J., de Oliveira, A.J. et al. The distribution and chemical coding of enteroendocrine cells in Trypanosoma cruzi-infected individuals with chagasic megacolon. Histochem Cell Biol 155, 451–462 (2021). https://doi.org/10.1007/s00418-020-01947-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-020-01947-w