Abstract
Purpose
The aim of this study was to determine the effects of high-intensity aerobic interval training (AIT) on exercise hemodynamics in metabolic syndrome (MetS) volunteers.
Methods
Thirty-eight, MetS participants were randomly assigned to a training (TRAIN) or to a non-training control (CONT) group. TRAIN consisted of stationary interval cycling alternating bouts at 70–90% of maximal heart rate during 45 min day−1 for 6 months.
Results
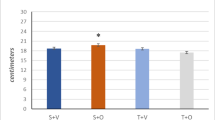
CONT maintained baseline physical activity and no changes in cardiovascular function or MetS factors were detected. In contrast, TRAIN increased cardiorespiratory fitness (14% in VO2PEAK; 95% CI 9–18%) and improved metabolic syndrome (−42% in Z score; 95% CI 83–1%). After TRAIN, the workload that elicited a VO2 of 1500 ml min−1 increased 15% (95% CI 5–25%; P < 0.001). After TRAIN when subjects pedaled at an identical submaximal rate of oxygen consumption, cardiac output increased by 8% (95% CI 4–11%; P < 0.01) and stroke volume by 10% (95% CI, 6–14%; P < 0.005) being above the CONT group values at that time point. TRAIN reduced submaximal exercise heart rate (109 ± 15–106 ± 13 beats min−1; P < 0.05), diastolic blood pressure (83 ± 8–75 ± 8 mmHg; P < 0.001) and systemic vascular resistances (P < 0.01) below CONT values. Double product was reduced only after TRAIN (18.2 ± 3.2–17.4 ± 2.4 bt min−1 mmHg 10−3; P < 0.05).
Conclusions
The data suggest that intense aerobic interval training improves hemodynamics during submaximal exercise in MetS patients. Specifically, it reduces diastolic blood pressure, systemic vascular resistances, and the double product. The reduction in double product, suggests decreased myocardial oxygen demands which could prevent the occurrence of adverse cardiovascular events during exercise in this population.
Clinicaltrials.gov identifier
NCT03019796.



Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular disease
- CRF:
-
Cardiorespiratory fitness
- DBP:
-
Diastolic blood pressure
- DP:
-
Double product
- GXT:
-
Graded exercise testing
- MetS:
-
Metabolic syndrome
- SBP:
-
Systolic blood pressure
- W MAX :
-
Maximal power output
- VO2PEAK :
-
Peak oxygen consumption rate
References
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SCJ (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645
Amati F, Dube JJ, Shay C, Goodpaster BH (2008) Separate and combined effects of exercise training and weight loss on exercise efficiency and substrate oxidation. J Appl Physiol 105(3):825–831. doi:10.1152/japplphysiol.90384.2008
Andrew GM, Guzman CA, Becklake MR (1966) Effect of athletic training on exercise cardiac output. J Appl Physiol 21(2):603–608
Arbab-Zadeh A, Dijk E, Prasad A, Fu Q, Torres P, Zhang R, Thomas JD, Palmer D, Levine BD (2004) Effect of aging and physical activity on left ventricular compliance. Circulation 110(13):1799–1805. doi:10.1161/01.CIR.0000142863.71285.74
Balady GJ, Schick EC Jr, Weiner DA, Ryan TJ (1986) Comparison of determinants of myocardial oxygen consumption during arm and leg exercise in normal persons. Am J Cardiol 57(15):1385–1387
Baynard T, Carhart RL Jr, Ploutz-Snyder LL, Weinstock RS, Kanaley JA (2008) Short-term training effects on diastolic function in obese persons with the metabolic syndrome. Obesity (Silver Spring) 16(6):1277–1283
Brage S, Wedderkopp N, Ekelund U, Franks PW, Wareham NJ, Andersen LB, Froberg K, European Youth Heart S (2004) Features of the metabolic syndrome are associated with objectively measured physical activity and fitness in Danish children: the European Youth Heart Study (EYHS). Diabetes Care 27(9):2141–2148
Brouwer E (1957) On simple formulae for calculating the heat expenditure and the quantities of carbohydrate and fat oxidized in metabolism of men and animals, from gaseous exchange (Oxygen intake and carbonic acid output) and urine-N. Acta Physiol Pharmacol Neerl 6:795–802
Cohen J (1988) Statistical power analysis for the behavioural sciences, 2nd edn. Lawrence Erlbaum Associates, New Jersey, p 569
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395. doi:10.1249/01.MSS.0000078924.61453.FB
Dill DB, Costill DL (1974) Calculation of percentage changes in volumes of blood, plasma, and red cells in dehydration. J Appl Physiol 37(2):247–248
Edgell H, Petrella RJ, Hodges GJ, Shoemaker JK (2012) Central versus peripheral cardiovascular risk in metabolic syndrome. Front Physiol 3:38. doi:10.3389/fphys.2012.00038
Egginton S (2011) Physiological factors influencing capillary growth. Acta Physiol (Oxf) 202(3):225–239. doi:10.1111/j.1748-1716.2010.02194.x
Ekblom B, Astrand PO, Saltin B, Stenberg J, Wallstrom B (1968) Effect of training on circulatory response to exercise. J Appl Physiol 24(4):518–528
Gledhill N, Cox D, Jamnik R (1994) Endurance athletes’ stroke volume does not plateau: major advantage is diastolic function. Med Sci Sports Exerc 26(9):1116–1121
Gobel FL, Norstrom LA, Nelson RR, Jorgensen CR, Wang Y (1978) The rate-pressure product as an index of myocardial oxygen consumption during exercise in patients with angina pectoris. Circulation 57(3):549–556
Gonzalez-Alonso J, Calbet JA, Boushel R, Helge JW, Sondergaard H, Munch-Andersen T, van Hall G, Mortensen SP, Secher NH (2015) Blood temperature and perfusion to exercising and non-exercising human limbs. Exp Physiol 100(10):1118–1131. doi:10.1113/EP085383
Hagberg JM, Goldberg AP, Lakatta L, O’Connor FC, Becker LC, Lakatta EG, Fleg JL (1998) Expanded blood volumes contribute to the increased cardiovascular performance of endurance-trained older men. J Appl Physiol 85(2):484–489
Ingelsson E, Sullivan LM, Murabito JM, Fox CS, Benjamin EJ, Polak JF, Meigs JB, Keyes MJ, O’Donnell CJ, Wang TJ, D’Agostino RB Sr, Wolf PA, Vasan RS (2007) Prevalence and prognostic impact of subclinical cardiovascular disease in individuals with the metabolic syndrome and diabetes. Diabetes 56(6):1718–1726. doi:10.2337/db07-0078
Kitamura K, Jorgensen CR, Gobel FL, Taylor HL, Wang Y (1972) Hemodynamic correlates of myocardial oxygen consumption during upright exercise. J Appl Physiol 32(4):516–522
Klausen K, Secher NH, Clausen JP, Hartling O, Trap-Jensen J (1982) Central and regional circulatory adaptations to one-leg training. J Appl Physiol 52(4):976–983
Lalande S, Petrella RJ, Shoemaker JK (2013) Effect of exercise training on diastolic function in metabolic syndrome. Appl Physiol Nutr Metab 38(5):545–550. doi:10.1139/apnm-2012-0383
MacDonald JR (2002) Potential causes, mechanisms, and implications of post exercise hypotension. J Hum Hypertens 16(4):225–236. doi:10.1038/sj.jhh.1001377
Moore G, Durstine JL, Painter P (2016) ACSM’s exercise management for persons with chronic diseases and disabilities, 4th edn. Human Kinetics, Champaign
Morales-Palomo F, Ramirez-Jimenez M, Ortega JF, Pallares JG, Mora-Rodriguez R (2017) Cardiovascular drift during training for fitness in patients with metabolic syndrome. Med Sci Sports Exerc 49(3):518–526. doi:10.1249/MSS.0000000000001139
Mora-Rodriguez R, Ortega JF, Hamouti N, Fernandez-Elias VE, Canete Garcia-Prieto J, Guadalupe-Grau A, Saborido A, Martin-Garcia M, Guio de Prada V, Ara I, Martinez-Vizcaino V (2014) Time-course effects of aerobic interval training and detraining in patients with metabolic syndrome. Nutr Metab Cardiovasc Dis 24(7):792–798. doi:10.1016/j.numecd.2014.01.011
Mora-Rodriguez R, Ortega JF, Guio de Prada V, Fernandez-Elias VE, Hamouti N, Morales-Palomo F, Martinez-Vizcaino V, Nelson RK (2016) Effects of simultaneous or sequential weight loss diet and aerobic interval training on metabolic syndrome. Int J Sports Med 37(4):274–281. doi:10.1055/s-0035-1564259
Mortensen SP, Svendsen JH, Ersboll M, Hellsten Y, Secher NH, Saltin B (2013) Skeletal muscle signaling and the heart rate and blood pressure response to exercise: insight from heart rate pacing during exercise with a trained and a deconditioned muscle group. Hypertension 61(5):1126–1133. doi:10.1161/HYPERTENSIONAHA.111.00328
Roca J, Agusti AG, Alonso A, Poole DC, Viegas C, Barbera JA, Rodriguez-Roisin R, Ferrer A, Wagner PD (1992) Effects of training on muscle O2 transport at VO2max. J Appl Physiol 73(3):1067–1076
Rowell LB (1986) Circulatory adjustments to dynamic exercise. Human circulation; regulation during physical stress. Oxford University Press, New York, pp 213–256
Saltin B, Blomqvist G, Mitchell JH, Johnson RL, Wildenthal K, Chapman CB (1968) Response to exercise after bed rest and after training. Circulation 38(5):VII1–VII78
Saltin B, Nazar K, Costill DL, Stein E, Jansson E, Essen B, Gollnick D (1976) The nature of the training response; peripheral and central adaptations of one-legged exercise. Acta Physiol Scand 96(3):289–305. doi:10.1111/j.1748-1716.1976.tb10200.x
Sawka MN, Young AJ, Pandolf KB, Dennis RC, Valeri CR (1992) Erythrocyte, plasma, and blood volume of healthy young men. Med Sci Sports Exerc 24(4):447–453
Stensvold D, Tjonna AE, Skaug EA, Aspenes S, Stolen T, Wisloff U, Slordahl SA (2010) Strength training versus aerobic interval training to modify risk factors of metabolic syndrome. J Appl Physiol 108(4):804–810. doi:10.1152/japplphysiol.00996.2009
Strandell T, Shepherd JT (1967) The effect in humans of increased sympathetic activity on the blood flow to active muscles. Acta Med Scand Suppl 472:146–167
Tjonna AE, Lee SJ, Rognmo O, Stolen TO, Bye A, Haram PM, Loennechen JP, Al-Share QY, Skogvoll E, Slordahl SA, Kemi OJ, Najjar SM, Wisloff U (2008) Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: a pilot study. Circulation 118(4):346–354. doi:10.1161/CIRCULATIONAHA.108.772822
Trilk JL, Singhal A, Bigelman KA, Cureton KJ (2011) Effect of sprint interval training on circulatory function during exercise in sedentary, overweight/obese women. Eur J Appl Physiol 111(8):1591–1597. doi:10.1007/s00421-010-1777-z
Warburton DE, Haykowsky MJ, Quinney HA, Blackmore D, Teo KK, Taylor DA, McGavock J, Humen DP (2004) Blood volume expansion and cardiorespiratory function: effects of training modality. Med Sci Sports Exerc 36(6):991–1000
Wilmore JH, Farrell PA, Norton AC, Cote RW 3rd, Coyle EF, Ewy GA, Temkin LP, Billing JE (1982) An automated, indirect assessment of cardiac output during rest and exercise. J Appl Physiol 52(6):1493–1497
Wilmore JH, Stanforth PR, Gagnon J, Rice T, Mandel S, Leon AS, Rao DC, Skinner JS, Bouchard C (2001) Cardiac output and stroke volume changes with endurance training: the HERITAGE Family Study. Med Sci Sports Exerc 33(1):99–106
Acknowledgements
This study was partially funded by a grant from the Spanish Ministry of Economy and Competivity (DEP-2014-52930-R).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Communicated by Carsten Lundby.
Rights and permissions
About this article
Cite this article
Mora-Rodriguez, R., Fernandez-Elias, V.E., Morales-Palomo, F. et al. Aerobic interval training reduces vascular resistances during submaximal exercise in obese metabolic syndrome individuals. Eur J Appl Physiol 117, 2065–2073 (2017). https://doi.org/10.1007/s00421-017-3697-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-017-3697-7