Abstract
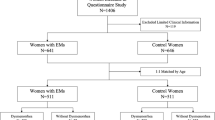
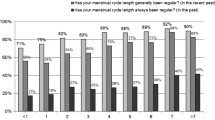
Dysmenorrhoea is the most common gynaecological symptom in adolescents. Secondary dysmenorrhoea is mostly due to endometriosis. There are no known follow-up studies of dysmenorrhoea into adulthood. Cases of endometriosis often have a long history of dysmenorrhea; however, studies to date have been retrospective. This longitudinal cohort study aimed at analysing the long-term outcomes of dysmenorrhoea and associated rate of endometriosis identified in this cohort. Participants of a study of adolescents seen for dysmenorrhoea were followed-up at an average of 10.24 years. Of those contactable (74), 70 (94.6%) were included. As adults, 19 (27.1%) had slight or no pain with menstruation. Increased age of menarche was found to be associated with no menstrual pain in adulthood (OR 2.10, p = 0.034). No adolescent characteristic studied was found to be associated with severe or very severe dysmenorrhoea as an adult. At follow-up, 13 young women (18.6%) had been diagnosed with endometriosis. All cases of endometriosis were mild. The use of the oral contraceptive pill as an adolescent and feeling an improvement in symptoms with treatment as an adolescent were found to be associated with a diagnosis of endometriosis.
Conclusion: These findings are important for counselling adolescents regarding this common presentation.
What is Known: •Dysmenorrhoea is the most common gynaecological complaint for adolescents What is New: •Dysmenorrhoea from adolescence resolves in 1 in 4 of young women and no adolescent characteristics predict severe or very severe pain with menstruation in adults. •Only 1 in 5 of women were found to have endometriosis (all mild disease), despite a mean of 10 years of preceding dysmenorrhoea. |


Similar content being viewed by others
Abbreviations
- DIE:
-
Deep infiltrating endometriosis
- HMB:
-
Heavy menstrual bleeding
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- OCP:
-
Oral contraceptive pill
References
Audebert A, Lecointre L, Afors K, Koch A, Wattiez A, Akladios C (2015) Adolescent endometriosis: report of a series of 55 cases with a focus on clinical presentation and long-term issues. J Minim Invasive Gynecol 22(5):834–840. https://doi.org/10.1016/j.jmig.2015.04.001
Barnhart KT, Schreiber CA (2009) Return to fertility following discontinuation of oral contraceptives. Fertil Steril 91(3):659–663
Chantler I, Mitchell D, Fuller A (2009) Actigraphy quantifies reduced voluntary physical activity in women with primary dysmenorrhea. J Pain 10(1):38–46
Chapron C, Souza C, Borghese B, Lafay-Pillet MC, Santulli P, Bijaoui G, Goffinet F, de Ziegler D (2011) Oral contraceptives and endometriosis: the past use of oral contraceptives for treating severe primary dysmenorrhea is associated with endometriosis, especially deep infiltrating endometriosis. Hum Reprod 26(8):2028–2035. https://doi.org/10.1093/humrep/der156
Chen C, Kwekkeboom K (2015) How do women deal with dysmenorrhea? J Pain 1(4):S32. https://doi.org/10.1016/j.jpain.2015.01.141
Chen CH, Lin YH, Heitkemper MM, Wu KM (2006) The self-care strategies of girls with primary dysmenorrhea: a focus group study in Taiwan. Health Care Women Int 27(5):418–427
Cheong Y, Tay P, Luk F, Gan HC, Li TC, Cooke I (2008) Laparoscopic surgery for endometriosis: how often do we need to re-operate? J Obstet Gynaecol 28(1):82–85. https://doi.org/10.1080/01443610701811761
De Sanctis V, Soliman A, Bernasconi S, Bianchin L, Bona G, Bozzola M, Buzi F, De Sanctis C, Tonini G, Rigon F, Perissinotto E (2015) Primary dysmenorrhea in adolescents: prevalence, impact and recent knowledge. Pediatr Endocrinol Rev 13(2):512–520
De Sanctis V, Soliman AT, Elsedfy H, Soliman NA, Elalaily R, El Kholy M (2016) Dysmenorrhea in adolescents and young adults: a review in different countries. Acta Biomed 87(3):233–246
Farland LV, Tamimi RM, Eliassen AH, Spiegelman D, Hankinson SE, Chen WY, Missmer SA (2016) Laparoscopically confirmed endometriosis and breast cancer in the Nurses’ Health Study II. Obstet Gynecol 128(5):1025–1031. https://doi.org/10.1097/AOG.0000000000001684
Giudice LC, Kao LC (2004) Endometriosis. Lancet 364(9447):1789–1799. https://doi.org/10.1016/s0140-6736(04)17403-5
Guo S-W (2009) Recurrence of endometriosis and its control. Hum Reprod Update 15(4):441–461. https://doi.org/10.1093/humupd/dmp007
Hadfield R, Mardon H, Barlow D, Kennedy S (1996) Delay in the diagnosis of endometriosis: a survey of women from the USA and the UK. Hum Reprod 11(4):878–880
Harlow SD, Park M (1996) A longitudinal study of risk factors for the occurrence, duration and severity of menstrual cramps in a cohort of college women. B J Obstet Gynaecol 103(11):1134–1142
Husby GK, Haugen RS, Moen MH (2003) Diagnostic delay in women with pain and endometriosis. Acta Obstet Gynecol Scand 82(7):649–653
Iacovides S, Avidon I, Baker FC (2015) What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update 21(6):762–778. https://doi.org/10.1093/humupd/dmv039
Jamieson D, Steege JF (1996) The prevalence of dysmenorrhea, dyspareunia, pelvic pain, and irritable bowel syndrome in primary care practices. Obstet Gynecol 87(1):55–58
Janssen EB, Rijkers AC, Hoppenbrouwers K, Meuleman C, D’Hooghe TM (2013) Prevalence of endometriosis diagnosed by laparoscopy in adolescents with dysmenorrhea or chronic pelvic pain: a systematic review. Hum Reprod Update 19(5):570–582. https://doi.org/10.1093/humupd/dmt016
Jarrell J, Brant R, Leung W, Taenzer P (2007) Women’s pain experience predicts future surgery for pain associated with endometriosis. J Obstet Gynaecol Can 29(12):988–991. https://doi.org/10.1016/s1701-2163(16)32689-5
Ju H, Jones M, Mishra G (2014) The prevalence and risk factors of dysmenorrhea. Epidemiol Rev 36(1):104–113. https://doi.org/10.1093/epirev/mxt009
Ju H, Jones M, Mishra GD (2015) A U-shaped relationship between body mass index and dysmenorrhea: a longitudinal study. PLoS One 10(7) (no pagination)):e0134187
Klein JR, Lift IF (1981) Epidemiology of adolescent dysmenorrhea. Pediatrics 68(5):661–664
Knox B, Azurah AGN, Grover SR (2015) Quality of life and menstruation in adolescents. Curr Opin Obstet Gynecol 27(5):309–314. https://doi.org/10.1097/GCO.0000000000000199
Latthe P, Latthe M, Say L, Gülmezoglu M, Khan KS (2006) WHO systematic review of prevalence of chronic pelvic pain: a neglected reproductive health morbidity. BMC Public Health 6(1):177. https://doi.org/10.1186/1471-2458-6-177
Liu DT, Hitchcock A (1986) Endometriosis: its association with retrograde menstruation, dysmenorrhoea and tubal pathology. Br J Obstet Gynaecol 93(8):859–862
Macer ML, Taylor HS (2012) Endometriosis and infertility: a review of the pathogenesis and treatment of endometriosis-associated infertility. Obstet Gynecol Clin N Am 39(4):535–549. https://doi.org/10.1016/j.ogc.2012.10.002
Magrina JF (2002) Complications of laparoscopic surgery. Clin Obstet Gynecol 45(2):469–480
Marjoribanks J, Ayeleke RO, Farquhar C, Proctor M (2015) Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev (7). doi:https://doi.org/10.1002/14651858.CD001751.pub3
Moen MH, Stokstad T (2002) A long-term follow-up study of women with asymptomatic endometriosis diagnosed incidentally at sterilization. Fertil Steril 78(4):773–776. https://doi.org/10.1016/S0015-0282(02)03336-8
Ohde S, Tokuda Y, Takahashi O, Yanai H, Hinohara S, Fukui T (2008) Dysmenorrhea among Japanese women. Elsevier Science B.V, Amsterdam., Italy
Osman A, Barrios FX, Kopper BA, Hauptmann W, Jones J, O’Neill E (1997) Factor structure, reliability, and validity of the pain catastrophizing scale. J Behav Med 20(6):589–605. https://doi.org/10.1023/a:1025570508954
Parker M, Sneddon A, Arbon P (2010) The menstrual disorder of teenagers (MDOT) study: determining typical menstrual patterns and menstrual disturbance in a large population-based study of Australian teenagers. BJOG 117(2):185–192
Proctor M, Farquhar C (2006) Diagnosis and management of dysmenorrhoea. BMJ: Brit Med J 332(7550):1134–1138
Rogers PA, D’Hooghe TM, Fazleabas A, Gargett CE, Giudice LC, Montgomery GW, Rombauts L, Salamonsen LA, Zondervan KT (2009) Priorities for endometriosis research: recommendations from an international consensus workshop. Reprod Sci 16(4):335–346. https://doi.org/10.1177/1933719108330568
Sanfilippo J, Erb T (2008) Evaluation and management of dysmenorrhea in adolescents. Clin Obstet Gynecol 51(2):257–267
Shadbolt NA, Parker MA, Orthia LA (2013) Communicating endometriosis with young women to decrease diagnosis time. Health Promot J Austr 24(2):151–154. https://doi.org/10.1071/HE12915
Signorello LB, Harlow BL, Cramer DW, Spiegelman D, Hill JA (1997) Epidemiologic determinants of endometriosis: a hospital-based case-control study. Ann Epidemiol 7(4):267–741
Stratton P, Khachikyan I, Sinaii N, Ortiz R, Shah J (2015) Association of chronic pelvic pain and endometriosis with signs of sensitization and myofascial pain. Obstet Gynecol 125(3):719–728. https://doi.org/10.1097/aog.0000000000000663
Strik C, Stommel MW, Schipper LJ, van Goor H, Ten Broek RP (2016) Risk factors for future repeat abdominal surgery. Langenbeck's Arch Surg 401(6):829–837. https://doi.org/10.1007/s00423-016-1414-3
Sundell G, Milsom I, Andersch B (1990) Factors influencing the prevalence and severity of dysmenorrhoea in young women. Br J Obstet Gynaecol 97(7):588–594
Treloar SA, Bell TA, Nagle CM, Purdie DM, Green AC (2010) Early menstrual characteristics associated with subsequent diagnosis of endometriosis. Am J Obstet Gynecol 202(6):534.e531–534.e536. https://doi.org/10.1016/j.ajog.2009.10.857
Unsal A, Ayranci U, Tozun M, Arslan G, Calik E (2010) Prevalence of dysmenorrhea and its effect on quality of life among a group of female university students. Ups J Med Sci 115(2):138–145
Vercellini P, Fedele L, Arcaini L, Bianchi S, Rognoni MT, Candiani GB (1989) Laparoscopy in the diagnosis of chronic pelvic pain in adolescent women. J Reprod Med 34(10):827–830
Viganò P, Parazzini F, Somigliana E, Vercellini P (2004) Endometriosis: epidemiology and aetiological factors. Best Pract Res Clin Obstet Gynaecol 18(2):177–200. https://doi.org/10.1016/j.bpobgyn.2004.01.007
Vignali M, Bianchi S, Candiani M, Spadaccini G, Oggioni G, Busacca M (2005) Surgical treatment of deep endometriosis and risk of recurrence. J Minim Invasive Gynecol 12(6):508–513. https://doi.org/10.1016/j.jmig.2005.06.016
Vincent K, Warnaby C, Stagg CJ, Moore J, Kennedy S, Tracey I (2011) Dysmenorrhoea is associated with central changes in otherwise healthy women. Pain 152(9):1966–1975. https://doi.org/10.1016/j.pain.2011.03.029
Wang L, Wang X, Wang W, Chen C, Ronnennberg AG, Guang W, Huang A, Fang Z, Zang T, Wang L, Xu X (2004) Stress and dysmenorrhoea: a population based prospective study. Occup Environ Med 61(12):1021–1026. https://doi.org/10.1136/oem.2003.012302
Weissman AM, Hartz AJ, Hansen MD, Johnson SR (2004) The natural history of primary dysmenorrhoea: a longitudinal study. BJOG 111(4):345–352
Wong LP (2011) Attitudes towards dysmenorrhoea, impact and treatment seeking among adolescent girls: a rural school-based survey. Aust J Rural Health 19(4):218–223
Yosef A, Allaire C, Williams C, Ahmed AG, Al-Hussaini T, Abdellah MS, Wong F, Lisonkova S, Yong PJ (2016) Multifactorial contributors to the severity of chronic pelvic pain in women. Am J Obstet Gynecol 215(6):760.e761–760.e714. https://doi.org/10.1016/j.ajog.2016.07.023
Author information
Authors and Affiliations
Contributions
Benita Knox performed the literature search and data analysis, and wrote the final manuscript draft. Yi Chen Ong was involved in the initial conceptualisation of the study and literature review, and undertook the follow-up study collecting all the data for the study. Mardiha Abu Bakar undertook the original cohort study and hence provided the comparison data from adolescence. Sonia R Grover conceptualised and designed the study, and contributed to and supervised the literature review, data analysis and manuscript completion.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Communicated by Mario Bianchetti
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 28 kb)
Rights and permissions
About this article
Cite this article
Knox, B., Ong, Y.C., Bakar, M.A. et al. A longitudinal study of adolescent dysmenorrhoea into adulthood. Eur J Pediatr 178, 1325–1332 (2019). https://doi.org/10.1007/s00431-019-03419-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03419-3