Abstract
Background
Inborn errors of metabolism (IEM), including organic acidemias and urea cycle defects, are characterized by systemic accumulation of toxic metabolites with deleterious effect on the developing brain. While hemodialysis (HD) is most efficient in clearing IEM-induced metabolic toxins, data regarding its use during the neonatal period is scarce.
Methods
We retrospectively summarize our experience with HD in 20 neonates with IEM-induced metabolic intoxication (seven with maple syrup urine disease, 13 with primary hyperammonia), over a 16-year period, between 2004 and 2020. All patients presented with IEM-induced neurologic deterioration at 48 h to 14 days post-delivery, and were managed with HD in a pediatric intensive care setting. HD was performed through an internal jugular acute double-lumen catheter (6.5–7.0 French), using an AK-200S (Gambro, Sweden) dialysis machine and tubing, with F3 or FXpaed (Fresenius, Germany) dialyzers.
Results
Median (interquartile range) age and weight at presentation were 5 (3–8) days and 2830 (2725–3115) g, respectively. Two consecutive HD sessions decreased the mean leucine levels from 2281 ± 631 to 179 ± 91 μmol/L (92.1% reduction) in MSUD patients, and the mean ammonia levels from 955 ± 444 to 129 ± 55 μmol/L (86.5% reduction), in patients with hyperammonemia. HD was uneventful in all patients, and led to marked clinical improvement in 17 patients (85%). Three patients (15%) died during the neonatal period, and four died during long-term follow-up.
Conclusions
Taken together, our results indicate that HD is safe, effective, and life-saving for most neonates with severe IEM-induced metabolic intoxication, when promptly performed by an experienced and multidisciplinary team.
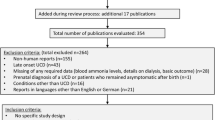
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information



Similar content being viewed by others
References
Chuang D, Shih V (2001) Maple syrup urine disease (branched-chain ketoaciduria). In: Scriver C, Beaudet A, Sly W, Valle D (eds) The Metabolic and Molecular Bases of Inherited Disease, 8th edn. McGraw-Hill, New-York, pp 1971–2006
Nellis MM, Kasinski A, Carlson M, Allen R, Schaefer AM, Schwartz EM, Danner DJ (2003) Relationship of causative genetic mutations in maple syrup urine disease with their clinical expression. Mol Genet Metab 80:189–195
Batshaw ML, Tuchman M, Summar M, Seminara J (2014) A longitudinal study of urea cycle disorders. Mol Genet Metab 113:127–130
Enns GM, Berry SA, Berry GT, Rhead WJ, Brusilow SW, Hamosh A (2007) Survival after treatment with phenylacetate and benzoate for urea-cycle disorders. N Engl J Med 356:2282–2292
Couce ML, Ramos F, Bueno MA, Díaz J, Meavilla S, Bóveda MD, Fernández-Marmiesse A, García-Cazorla A (2015) Evolution of maple syrup urine disease in patients diagnosed by newborn screening versus late diagnosis. Eur J Paediatr Neurol 19:652–659
Herrin JT, McCredie DA (1969) Peritoneal dialysis in the reduction of blood ammonia levels in a case of hyperammonaemia. Arch Dis Child 44:149–151
Gortner L, Leupold D, Pohlandt F, Bartmann P (1989) Peritoneal dialysis in the treatment of metabolic crises caused by inherited disorders of organic and amino acid metabolism. Acta Paediatr Scand 78:706–711
Robert MF, Schultz DJ, Wolf B, Cochran WD, Schwartz AL (1979) Treatment of a neonate with propionic acidaemia and severe hyperammonaemia by peritoneal dialysis. Arch Dis Child 54:962–965
Picca S, Dionisi-Vici C, Bartuli A, De Palo T, Papadia F, Montini G, Materassi M, Donati MA, Verrina E, Schiaffino MC, Pecoraro C, Iaccarino E, Vidal E, Burlina A, Emma F (2015) Short-term survival of hyperammonemic neonates treated with dialysis. Pediatr Nephrol 30:839–847
Jouvet P, Poggi F, Rabier D, Michel JL, Hubert P, Sposito M, Saudubray JM, Man NK (1997) Continuous venovenous haemodiafiltration in the acute phase of neonatal maple syrup urine disease. J Inherit Metab Dis 20:463–472
Arbeiter AK, Kranz B, Wingen AM, Bonzel KE, Dohna-Schwake C, Hanssler L, Neudorf U, Hoyer PF, Büscher R (2010) Continuous venovenous haemodialysis (CVVHD) and continuous peritoneal dialysis (CPD) in the acute management of 21 children with inborn errors of metabolism. Nephrol Dial Transplant 25:1257–1265
Tsai IJ, Hwu WL, Huang SC, Lee NC, Wu ET, Chien YH, Tsau YK (2014) Efficacy and safety of intermittent hemodialysis in infants and young children with inborn errors of metabolism. Pediatr Nephrol 29:111–116
Atwal PS, Macmurdo C, Grimm PC (2015) Haemodialysis is an effective treatment in acute metabolic decompensation of maple syrup urine disease. Mol Genet Metab Rep 4:46–48
Pode-Shakked N, Korman SH, Pode-Shakked B, Landau Y, Kneller K, Abraham S, Shaag A, Ulanovsky I, Daas S, Saraf-Levy T, Reznik-Wolf H, Vivante A, Pras E, Almashanu S, Anikster Y (2020) Clues and challenges in the diagnosis of intermittent maple syrup urine disease. Eur J Med Genet 63:103901
Wong KY, Wong SN, Lam SY, Tam S, Tsoi NS (1998) Ammonia clearance by peritoneal dialysis and continuous arteriovenous hemodiafiltration. Pediatr Nephrol 12:589–591
Schaefer F, Straube E, Oh J, Mehls O, Mayatepek E (1999) Dialysis in neonates with inborn errors of metabolism. Nephrol Dial Transplant 14:910–918
Chan WKY, But WM, Law CW (2002) Ammonia detoxification by continuous venovenous haemofiltration in an infant with urea cycle defect. Hong Kong Med J 8:207–210
Lai YC, Huang HP, Tsai IJ, Tsau YK (2007) High-volume continuous venovenous hemofiltration as an effective therapy for acute management of inborn errors of metabolism in young children. Blood Purif 25:303–308
Mateer FM, Greenman L, Danowski TS (1955) Hemodialysis of the uremic child. Am J Dis Child 89:645–655
Häberle J, Burlina A, Chakrapani A, Dixon M, Karall D, Lindner M, Mandel H, Martinelli D, Pintos-Morell G, Santer R, Skouma A, Servais A, Tal G, Rubio V, Huemer M, Dionisi-Vici C (2019) Suggested guidelines for the diagnosis and management of urea cycle disorders: first revision. J Inherit Metab Dis 42:1192–1230
Sadowski RH, Harmon WE, Jabs K (1994) Acute hemodialysis of infants weighing less than five kilograms. Kidney Int 45:903–906
Rutledge SL, Havens PL, Haymond MW, McLean RH, Kan JS, Brusilow SW (1990) Neonatal hemodialysis: effective therapy for the encephalopathy of inborn errors of metabolism. J Pediatr 116:125–128
Rajpoot DK, Gargus JJ (2004) Acute hemodialysis for hyperammonemia in small neonates. Pediatr Nephrol 19:390–395
McBryde KD, Kershaw DB, Bunchman TE, Maxvold NJ, Mottes TA, Kudelka TL, Brophy PD (2006) Renal replacement therapy in the treatment of confirmed or suspected inborn errors of metabolism. J Pediatr 148:770–778
Puliyanda DP, Harmon WE, Peterschmitt MJ, Irons M, Somers MJG (2002) Utility of hemodialysis in maple syrup urine disease. Pediatr Nephrol 17:239–242
Unsinn C, Das A, Valayannopoulos V, Thimm E, Beblo S, Burlina A, Konstantopoulou V, Mayorandan S, de Lonlay P, Rennecke J, Derbinski J, Hoffmann GF, Häberle J (2016) Clinical course of 63 patients with neonatal onset urea cycle disorders in the years 2001–2013. Orphanet J Rare Dis 11:116
Raina R, Bedoyan JK, Lichter-Konecki U, Jouvet P, Picca S, Mew NA, Machado MC, Chakraborty R, Vemuganti M, Grewal MK, Bunchman T, Sethi SK, Krishnappa V, McCulloch M, Alhasan K, Bagga A, Basu RK, Schaefer F, Filler G, Warady BA (2020) Consensus guidelines for management of hyperammonaemia in paediatric patients receiving continuous kidney replacement therapy. Nat Rev Nephrol 16:471–482
Kido J, Nakamura K, Mitsubuchi H, Ohura T, Takayanagi M, Matsuo M, Yoshino M, Shigematsu Y, Yorifuji T, Kasahara M, Horikawa R, Endo F (2012) Long-term outcome and intervention of urea cycle disorders in Japan. J Inherit Metab Dis 35:777–785
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Rambam Health Care Campus Ethics Committee.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Eisenstein, I., Pollack, S., Hadash, A. et al. Acute hemodialysis therapy in neonates with inborn errors of metabolism. Pediatr Nephrol 37, 2725–2732 (2022). https://doi.org/10.1007/s00467-022-05507-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05507-3