Summary
Background
Globally, it is estimated that approximately 1.3 billion people live with some form of hearing impairment. Major causes of hearing loss include infection/disease, age-related factors, and occupational factors. Numerous systematic reviews and meta-analyses have attempted to synthesise literature on these topics. To date there has not been a systematic evaluation of the relationships between hearing impairment and diverse physical, mental, and social outcomes.
Objective
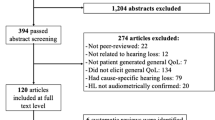
We performed an umbrella review of systematic reviews of observational studies with meta-analyses for any physical disease, biomarkers of disease, mental health or cognitive outcomes, and/or modifiable risk factors associated with hearing impairment.
Methods
For each meta-analytic association, random effects summary effect size, 95% confidence intervals, heterogeneity, evidence for small-study effect, excess significance bias and 95% prediction intervals were calculated, and risk of bias was assessed via the AMSTAR2 tool. These were used to grade significant evidence (p < 0.05) from I to IV, using the recommendations from the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) criteria.
Results
From 3747 studies, 21 were included covering 54 outcomes. Overall, 44/54 outcomes (82%) yielded significant results. Of the highest quality evidence, age-related hearing loss and non-specific hearing impairment were negatively associated with several types of cognitive impairments; pediatric bilateral hearing loss was negatively associated with quality of life, sensorineural hearing loss was positively associated with rheumatoid arthritis and tinnitus was positively associated with temporomandibular disorders.
Conclusion and relevance
Results show moderate quality evidence for associations between several types of hearing impairments and cognitive difficulties, quality of life and systemic diseases such as rheumatoid arthritis. Practitioners and public health policies should note these findings when developing relevant healthcare policies.

Similar content being viewed by others
References
Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800.
World Health Organization. Deafness and hearing loss. 2020. https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss. Accessed 27 July 2020.
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–96.
Forouzanfar MH, Afshin A, Alexander LT, Anderson HR, Bhutta ZA, Biryukov S, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1659–724.
Huddle MG, Goman AM, Kernizan FC, Foley DM, Price C, Frick KD, et al. The economic impact of adult hearing loss: a systematic review. JAMA Otolaryngol Head Neck Surg. 2017;143:1040–8.
Horikawa C, Kodama S, Tanaka S, Fujihara K, Hirasawa R, Yachi Y, et al. Diabetes and risk of hearing impairment in adults: a meta-analysis. J Clin Endocrinol Metab. 2013;98:51–8.
Chang IJ, Kang CJ, Yueh CY, Fang KH, Yeh RM, Te Tsai Y. The relationship between serum lipids and sudden sensorineural hearing loss: a systematic review and meta-analysis. Plos One. 2015;10:e121025.
Lin RJ, Krall R, Westerberg BD, Chadha NK, Chau JK. Systematic review and meta-analysis of the risk factors for sudden sensorineural hearing loss in adults. Laryngoscope. 2012;122:624–35.
Purcell PL, Shinn JR, Davis GE, Sie KC. Children with unilateral hearing loss may have lower intelligence quotient scores: a meta-analysis. Laryngoscope. 2016;126:746–54.
Linszen MM, Brouwer RM, Heringa SM, Sommer IE. Increased risk of psychosis in patients with hearing impairment: review and meta-analyses. Neurosci Biobehav Rev. 2016;62:1–20.
Lawrence BJ, Jayakody DM, Bennett RJ, Eikelboom RH, Gasson N, Friedland PL. Hearing loss and depression in older adults: a systematic review and meta-analysis. Gerontologist. 2020;60:e137–e54.
Roland L, Fischer C, Tran K, Rachakonda T, Kallogjeri D, Lieu JE. Quality of life in children with hearing impairment: systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2016;155:208–19.
Stevenson J, Kreppner J, Pimperton H, Worsfold S, Kennedy C. Emotional and behavioural difficulties in children and adolescents with hearing impairment: A systematic review and meta-analysis. Eur Child Adolesc Psychiatry. 2015;24:477–96.
Ioannidis JP. Integration of evidence from multiple meta-analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. CMAJ. 2009;181:488–93.
Ioannidis J. Next-generation systematic reviews: prospective meta-analysis, individual-level data, networks and umbrella reviews. Br J Sport Med. 2017;51:1456–8
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13:132–40.
Radua J, Ramella-Cravaro V, Ioannidis JP, Reichenberg A, Phiphopthatsanee N, Amir T, et al. What causes psychosis? An umbrella review of risk and protective factors. 2018;17:49–66.
Raglan O, Kalliala I, Markozannes G, Cividini S, Gunter MJ, Nautiyal J, et al. Risk factors for endometrial cancer: an umbrella review of the literature. Int J Cancer. 2019;145:1719–30.
Theodoratou E, Tzoulaki I, Zgaga L, Ioannidis JP. Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ. 2014;348:g2035.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549.
Bortolato B, Köhler CA, Evangelou E, León-Caballero J, Solmi M, Stubbs B, et al. Systematic assessment of environmental risk factors for bipolar disorder: an umbrella review of systematic reviews and meta-analyses. Bipolar Disord. 2017;19:84–96.
Dragioti E, Evangelou E, Larsson B, Gerdle B. Effectiveness of multidisciplinary programmes for clinical pain conditions: an umbrella review. J Rehabil Med. 2018;50:779–91.
Ioannidis JP, Trikalinos TA. An exploratory test for an excess of significant findings. Clin Trials. 2007;4:245–53.
Ioannidis JP. Clarifications on the application and interpretation of the test for excess significance and its extensions. J Math Psychol. 2013;57:184–7.
Dragioti E, Karathanos V, Gerdle B, Evangelou E. Does psychotherapy work? An umbrella review of meta-analyses of randomized controlled trials. Acta Psychiatr Scand. 2017;136:236–46.
Li X, Meng X, Timofeeva M, Tzoulaki I, Tsilidis KK, Ioannidis JP, et al. Serum uric acid levels and multiple health outcomes: umbrella review of evidence from observational studies, randomised controlled trials, and Mendelian randomisation studies. BMJ. 2017;357:j2376.
Veronese N, Solmi M, Caruso MG, Giannelli G, Osella AR, Evangelou E, et al. Dietary fiber and health outcomes: an umbrella review of systematic reviews and meta-analyses. Am J Clin Nutr. 2018;107:436–44.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Do B, Lynch P, Macris E‑M, Smyth B, Stavrinakis S, Quinn S, et al. Systematic review and meta-analysis of the association of Autism Spectrum Disorder in visually or hearing impaired children. Ophthalmic Physiol Opt. 2017;37:212–24.
Wei J, Hu Y, Zhang L, Hao Q, Yang R, Lu H, et al. Hearing impairment, mild cognitive impairment, and dementia: a meta-analysis of cohort studies. Dement Geriatr Cogn Disord Extra. 2017;7:440–52.
Teng Z‑P, Tian R, Xing F‑L, Tang H, Xu J‑J, Zhang B‑W, et al. An association of type 1 diabetes mellitus with auditory dysfunction: a systematic review and meta-analysis. Laryngoscope. 2017;127:1689–97.
Upala S, Rattanawong P, Vutthikraivit W, Sanguankeo A. Significant association between osteoporosis and hearing loss: a systematic review and meta-analysis. Braz J Otorhinolaryngol. 2017;83:646–52.
Loughrey DG, Kelly ME, Kelley GA, Brennan S, Lawlor BA. Association of Age-related hearing loss with cognitive function, cognitive impairment, and dementia: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg. 2018;144:115–26.
Lee DY, Kim YH. Risk factors of pediatric tinnitus: systematic review and meta-analysis. Laryngoscope. 2018;128:1462–8.
Ford AH, Hankey GJ, Yeap BB, Golledge J, Flicker L, Almeida OP. Hearing loss and the risk of dementia in later life. Maturitas. 2018;112:1–11.
Ji S, Chen X, Shi H, Zhang B, Yao S, Deng S, et al. Relationship between platelet parameters and sudden sensorineural hearing loss: a systematic review and meta-analysis. Biosci Rep. 2018. https://doi.org/10.1042/BSR20181183.
Yu H, Li H. Association of vertigo with hearing outcomes in patients with sudden sensorineural hearing loss: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg. 2018;144:677–83.
Bayat A, Saki N, Nikakhlagh S, Mirmomeni G, Raji H, Soleimani H, et al. Is COPD associated with alterations in hearing? A systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2019;14:149.
Mohammed SH, Shab-Bidar S, Abuzerr S, Habtewold TD, Alizadeh S, Djafarian K. Association of anemia with sensorineural hearing loss: a systematic review and meta-analysis. BMC Res Notes. 2019;12:283.
Omidvar S, Jafari Z. Association between Tinnitus and temporomandibular disorders: a systematic review and meta-analysis. Ann Otol Rhinol Laryngol. 2019;128:662–75.
Chaitidis N, Theocharis P, Festas C, Aritzi I. Association of rheumatoid arthritis with hearing loss: a systematic review and meta-analysis. Rheumatol Int. 2020;40:1771–9.
Li X, Rong X, Wang Z, Lin A. Association between smoking and noise-induced hearing loss: a meta-analysis of observational studies. Int J Environ Res Public Health. 2020. https://doi.org/10.3390/ijerph17041201.
Rönnberg J, Lunner T, Zekveld A, Sörqvist P, Danielsson H, Lyxell B, et al. The Ease of Language Understanding (ELU) model: theoretical, empirical, and clinical advances. Front Syst Neurosci. 2013;7:31.
van der Werf M, Thewissen V, Dominguez M, Lieb R, Wittchen H, van Os J. Adolescent development of psychosis as an outcome of hearing impairment: a 10-year longitudinal study. Psychol Med. 2011;41:477–85.
van der Werf M, van Winkel R, van Boxtel M, van Os J. Evidence that the impact of hearing impairment on psychosis risk is moderated by the level of complexity of the social environment. Schizophr Res. 2010;122:193–8.
Zhu T, Feng L. Comparison of anti-mutated citrullinated vimentin, anti-cyclic citrullinated peptides, anti-glucose-6-phosphate isomerase and anti-keratin antibodies and rheumatoid factor in the diagnosis of rheumatoid arthritis in Chinese patients. Int J Rheum Dis. 2013;16:157–61.
Li L, Deng C, Chen S, Zhang S, Wu Z, Hu C, et al. Meta-analysis: diagnostic accuracy of anti-carbamylated protein antibody for rheumatoid arthritis. Plos One. 2016;11:e159000.
National Health Service. 5 ways to prevent hearing loss. 2021. https://www.nhs.uk/live-well/healthy-body/-5-ways-to-prevent-hearing-loss-/. Accessed 27 Apr 2021.
Ioannidis JPA. The mass production of redundant, misleading, and conflicted systematic reviews and meta-analyses. Milbank Q. 2016;94:485–514.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Trott, L. Smith, T. Xiao, N. Veronese, A. Koyanagi, L. Jacob, G. F. Lopez-Sanchez, Y. Barnett and S. Pardhan have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work. Transparency statement: the lead author confirms that the manuscript is an honest, accurate, and transparent account of the study being reported. No important aspects of the study have been omitted.
Ethical standards
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case. Because this is a systematic review, ethical approval was not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Table 1:
Full details of AMSTAR2 results
Rights and permissions
About this article
Cite this article
Trott, M., Smith, L., Xiao, T. et al. Hearing impairment and diverse health outcomes. Wien Klin Wochenschr 133, 1028–1041 (2021). https://doi.org/10.1007/s00508-021-01893-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-021-01893-0