Abstract
Purpose
The purpose of this study is to pilot test the effectiveness of using recently developed clinical guidelines from Australia for conducting palliative care family meetings in Japan.
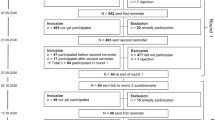
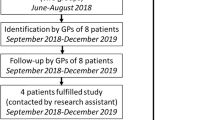
Methods
Palliative care family meetings were conducted using clinical guidelines with 15 primary family carers of cancer patients who were admitted to an acute care hospital in Japan. Using the pre-family meeting questionnaire, the primary carers were asked to write key concerns to discuss during the family meetings and rate their concerns via a numerical rating scale: how upset/worried they were about the problem, frequency in which problem occurs, life interference with the problem, and the confidence to deal with the problem. Within 3 days after the meeting, the primary carers were asked to complete the post-meeting questionnaire to evaluate the effectiveness of the family meeting.
Results
There was a significant improvement in family carers’ psychological well-being in the post-meeting questionnaires compared to the pre-meeting questionnaires as follows: how upset/worried they were about the problem, t(14) = 3.1071, p < 0.000011; frequency in which problem occurs, t(14) = 3.2857, p < 0.000013; life interference with the problem, t(14) = 2.7857, p < 0.000008; and the confidence to deal with the problem, t(13) = −2.3007, p < 0.005480.
Conclusions
In accordance with the study aims, we were able to demonstrate the utility of a questionnaire as an essential tool to plan and conduct effective communication between health professionals and primary family carers in Japanese cancer patients. This pilot test should be followed up with a larger sample and a controlled trial.
Similar content being viewed by others
References
World Health Organization (2003) Cancer pain release. WHO, Geneva
Hudson PL, Hayman-White K (2006) Measuring the psychosocial characteristics of family caregivers of palliative care patients; psychomotor properties of nine self-report instruments. J Pain Symptom Manage 31(3):215–228
Gough K, Hudson P (2009) Psychometric properties of the hospital anxiety and depression scale in family caregivers of palliative care patients. J Pain Symptom Manage 37(5):797–806
Walsh K, Jones L, Tookman A, Mason C, McLoughlin J, Blizard R, King M (2007) Reducing emotional distress in people caring for patients receiving specialist palliative care. Randomized trial. Br J Psychiatry 190:142–147
Hudson PL, Quinn K, O’Hanlon B, Aranda S (2009) Family meetings in palliative care: multidisciplinary clinical practice guidelines. BMC Palliat care 7:12
Hudson PL, Thomas T, Quinn K (2009) Family meetings in palliative care: are they effective? Palliat Med 23:150–157
Fujimori M, Parker PA, Akechi T, Sakano Y, Basile WF, Uchitomi Y (2007) Japanese cancer patients’ communication style preferences when receiving bad news. Psychooncology 16(7):617–625
Hudson P (2009) Conducting a family meeting, a resource for health professionals working in cancer and palliative care. The Centre for Palliative Care Education & Research and the Peter MacCallum Cancer Centre
Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, Erikson P (2005) Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health 8(2):94–104
Morita T, Akechi T, Ikenaga M, Kizawa Y, Kohara H, Mukaiyama T, Nakaho T, Nakashima N, Shima Y, Matsubara T, Fujimori M, Uchitomi Y (2004) Communication about the ending of anticancer treatment and transition to palliative care. Ann Oncol 15:1551–1557
Uchitomi Y, Yamawaki S (2006) Truth-telling practice in cancer care in Japan. Ann N Y Acad Sci 809(1):290–299
Shinjo T, Morita T, Hirai K, Miyashita M, Sato K, Tsuneto S (2010) Care for immediately dying cancer patients: family member’s experience and recommendations. J Clin Oncol 28:142–148
Conflict of interest
We have nothing to declare in relation to conflicts of interest. We, the authors, all agree to submit the manuscript and are responsible for the contents.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 45 kb)
Rights and permissions
About this article
Cite this article
Fukui, M., Iwase, S., Sakata, N. et al. Effectiveness of using clinical guidelines for conducting palliative care family meetings in Japan. Support Care Cancer 21, 53–58 (2013). https://doi.org/10.1007/s00520-012-1491-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-012-1491-y