Abstract
Purpose
To determine if cardiopulmonary exercise testing (CPET) was useful in predicting response to exercise in cancer patients preoperatively. A secondary aim was to explore if exercise was associated with improved postoperative outcomes.
Methods
A retrospective cohort study was performed on consecutive cancer patients from 2012 to 2014, referred for exercise prehabilitation and had two CPET preoperatively.
Results
Twenty-six patients were analysed. There was a significant overall increase in oxygen uptake at anaerobic threshold (AT) from 10.4 to 11.6 ml kg−1 min−1 (ΔAT = 1.2 ± 3.0 ml kg−1 min−1 [9 %]; p = 0.046); peak oxygen uptake (pVO2) from 16.0 to 17.7 ml kg−1 min−1 (ΔpVO2 = 1.7 ± 2.4 ml kg−1 min−1 [9 %]; p = 0.002); and pVO2/BSA from 658 to 726 ml min−1 m−2; (ΔpVO2/BSA = 68 ± 112.3 mL min−1 m2 [10 %]; p = 0.004). Fifty percent of patients were responders to exercise, defined as having >10 % increase in AT. Responders had a median increase in AT of 26 % [IQR 7 %, 45 %] with an absolute increase in AT of 2.5 ml kg−1 min−1 [IQR 1.1, 3.9] (p = 0.002) and a median increase in pVO2 of 22 % [IQR 11.5, 32.5 %] with an absolute increase in pVO2 of 3.8 ml.kg−1.min−1 [IQR 2.0, 5.7] (p < 0.001). Responders were more likely to have a lower baseline AT (9.1 ml kg−1 min−1; p = 0.002).
Conclusions
Exercise improved cardiorespiratory fitness prior to major cancer surgery. Not all patients responded the same, with only 50 % of the study cohort being responders to exercise. A low AT, pVO2 and ratio of AT/pVO2 at baseline were good predictors of response to exercise, with a tendency for responders to suffer fewer major postoperative complications.
Similar content being viewed by others
Introduction
Patients are often deconditioned due to their underlying disease, associated medical comorbidities and through lifestyle choice. In cancer patients, neoadjuvant chemoradiotherapy further reduces physical fitness [1]. Cardiopulmonary exercise testing (CPET), the gold standard for assessing the integrated cardiorespiratory, vascular and metabolic (mitochondrial) systems, allows for objective evaluation of functional capacity and preoperative risk stratification; with gas exchange derived variables such as oxygen consumption at anaerobic threshold (AT) and oxygen consumption at peak exercise (peak VO2) identified as good predictors of postoperative morbidity [2–8].
Exercise programs in cancer patients and, more specific to perioperative medicine, prehabilitation programs prior to major surgery are an emerging field of investigation [1, 9, 10]. Prehabilitation involves multimodal interventions targeted to improve psychological, nutritional and physical well-being from time of cancer diagnosis to definitive treatment, including surgery [10]. Li and colleagues showed that a trimodal prehabilitation program using exercise, nutrition and psychological support improved recovery of functional capacity 8 weeks after surgery [11]. Patients who had prehabilitation were able to walk further at 2 months postoperatively compared with those that only had rehabilitation [10]. Since cancer surgery is often urgent, but not emergent, it allows for prehabilitation of deconditioned patients to improve their functional capacity prior to major surgery, with potential for reduced postoperative morbidity (which often requires costly extensive postoperative rehabilitation). However, implementation of a 4–6-week prehabilitation program with exercise prior to surgery is relatively resource and time intensive, and it is unknown if all patients will be responders to such an exercise program, and if response to exercise improves postoperative outcomes. Bouchard and colleagues reported that genomics plays a central role in response to an exercise program and improved peak VO2 [12].
Although there have been studies published on the efficacy of an exercise program in patients from various cancer types or selected surgeries [1, 10, 13–18], data on predicting the response to exercise programs and the impact on associated postoperative outcome is still unknown. Determining which group of patients are more likely to improve their functional capacity in response to an exercise program would be useful, allowing rational use of resources with selective referral for prehabilitation and associated postponement of surgery.
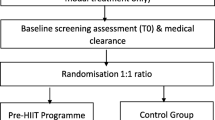
Given the current paucity of evidence to support the notion that postponement of cancer surgery to allow recovery of physiologic capacity is beneficial to cancer patients, this study sets out to determine the effectiveness of a prehabilitation exercise program at improving preoperative functional capacity, and if CPET-derived gas exchange variables were useful in predicting a response to exercise prehabilitation programs. A secondary aim of the study explored if exercise prehabilitation was associated with improved postoperative outcomes in cancer patients.
Methods
Patients
The Peter MacCallum Cancer Centre (PMCC) Human Ethics Research Committee approved this retrospective cohort study (#13/44 L). For this type of study, formal consent is not required. All consecutive patients referred to exercise physiology for a structured exercise program preoperatively at PMCC between September 2012 and August 2014 were included in this study. The exclusion criteria were patients who did not have two CPET evaluations (baseline and postprehabilitation), patients who did not proceed to surgery and patients who had their exercise program commenced prior to their first CPET, as they did not have a baseline CPET result. Patients who were referred for exercise physiology input were a high-risk cancer group who were deconditioned and deemed at risk of postoperative complications during preoperative CPET evaluation. Surgery types included oesophagogastrectomy, complex colorectal (pelvic exenteration, anterior resection, abdominoperineal resection, hyperthermic intraperitoneal chemotherapy) and thoracic cancer surgery. They were referred to haematology for preoperative optimisation of haemoglobin or for nutritional input prior to surgery, from the preadmission clinic, at the discretion of the anaesthetist, if clinically warranted. Patients received standard perioperative care. Their anaesthetist determined their postoperative destination either intensive care unit (ICU), high dependency unit (HDU) or ward.
Cardiopulmonary exercise testing
Patients underwent a baseline CPET test (CPX1) prior to their exercise program and a final CPET test following prehabilitation prior to surgery (CPX2). Some patients underwent an extra CPET test between their baseline and final CPET test, usually after completion of their neoadjuvant chemoradiotherapy.
CPET was chosen as the measurement tool in this study because it provides a non-invasive and objective global assessment of the body’s response to exercise. CPET incorporates cardiovascular, pulmonary, metabolic, haemopoietic and musculoskeletal systems and surpasses individual end-organ tests as a method of assessing progress of cardiopulmonary fitness. CPET has been shown to have good inter-observer reliability of 4.5 % [19] with a 10 % coefficient of variation for repeated testing [20].
CPET was performed as per the American Thoracic Society/American College of Chest Physicians (ATS/ACCP) practice guidelines [21]. A static respiratory function test was performed prior to exercise. Baseline data, collected with the patient at rest for 3 min, included the following: blood pressure, continuous 12-lead electrocardiogram (ECG), oxygen saturation and breath-by-breath gas exchange through a tight fitting mask (CardiO2/CP System, Medical Graphics Corporation, USA). During the exercise phase, patients cycled at 60–70 RPM on a cycle ergometer: 3 min of unloaded cycling, then a ramp protocol of 20 W per minute through increasing pedal resistance until peak exercise, and then 5 min of unloaded cycling during the recovery period. A clinician was present throughout. Ramping was stopped after achieving peak exercise at the patient or clinician’s discretion, either due to patient fatigue, dyspnoea, chest pain, leg pain or signs of myocardial ischaemia, hypotension or arrhythmia. AT was determined using both the V-slope and ventilator equivalent methods [22] by two experienced anaesthetists trained in cardiopulmonary exercise testing. Two independent reviewers analysed and crosschecked the CPET data to ensure accuracy.
Exercise program
The Australia Association for Exercise and Sport Science position statement on optimising cancer outcomes through exercise recommends an individualised exercise prescription, consisting of both aerobic and resistance exercises, taking into consideration the patient’s disease process, treatment stage and level of function [23]. An exercise physiologist prescribed individualised exercise programs according to the patient’s baseline CPET results. The exercise program was adapted to the needs of the patient and patient’s environment (either home-, community- or hospital-based), with weekly follow-up and assessment of compliance. The program consisted of progressive aerobic (interval training) and strength training exercises, three to five times per week, at an intensity of 60 to 80 % of the maximum heart rate at peak VO2, and lasting 20 to 45 min in duration.
Patient characteristics and outcome measures
Using case note review, data was collected on patient demographics, comorbidities, neoadjuvant treatment, prescribed exercise program, surgical procedure, postoperative complications and mortality at 30 days, 6 months and 1 year.
In our study, we defined responders to the exercise program as having >10 % improvement in AT, since 10 % is reported as the coefficient of variation for repeated testing during CPET [20]. Non-responders were defined as patients who had ≤10 % increase in AT after their exercise program. Major postoperative complications were defined as those represented by a Clavien-Dindo classification >3, representing a life threatening complication, either single organ or multi-organ failure, requiring ICU management, or death. This cutoff was chosen as a Clavien-Dindo classification ≤3 may be the result of surgical technique or surgical complications, rather than impaired cardiopulmonary reserve.
Statistical analysis
Statistical analysis was performed using SPSS Statistics Version 22 (IBM Corp. in Armonk, NY). Continuous variables are presented as mean +/− standard deviation (SD) if normally distributed or median +/− interquartile range [IQR] for skewed data, and categorical variables are presented as the absolute number with percentages (%). Parametric data was analysed using paired Student’s t test or independent Student’s t test. Non-parametric data was analysed using Mann-Whitney U test. Categorical data was analysed using Fisher’s exact test. Multivariable analysis using an exact logistic regression model assessed for predictors of a major postoperative complication (Clavien-Dindo classification >3) and also whether responders could be predicted from CPX1 or if CPX2 was required. Odds ratios are presented. As this was hypothesis generating, p < 0.1 was considered significant for predictors of a major postoperative complication and worth consideration for further research. There was no adjustment for multiple testing in the analysis for non-primary outcomes. A p value <0.05 was considered statistically significant for the remaining analysis.
Results
Thirty-two consecutive patients were referred for a prehabilitation exercise program within the defined study period. Of the patients eligible for the study, six were excluded: One patient had only one CPET, one patient did not proceed to surgery and four patients had exercise programs that were initiated prior to their baseline CPET. The remaining 26 patients were analysed. Baseline patient characteristics are reported in Table 1.
Following prehabilitation, a significant overall improvement in functional capacity was observed for the study cohort across three measured CPET-derived domains: AT increased 9 % from 10.4 to 11.6 ml kg−1 min−1; p = 0.046; pVO2 increased 9 % from 16.0 to 17.7 ml kg−1 min−1; p = 0.002; and peak VO2/BSA increased 10 % from 658 to 726 ml min−1 m−2; p = 0.004 (Tables 2, 3 and 4). The exercise program consisted of aerobic exercise only in 35 % of the patients and aerobic combined with resistance exercise programs in 65 % of patients. Location of exercise program was as follows: 50 % of patients conducted their exercise program at home, 27 % in the community and 23 % at a hospital. The median duration of exercise program was 74 days [IQR 28, 120 days]; (range 26 to 461 days).
Fifty percent of the cohort was considered responders to their tailored exercise program. Responders had a median increase in AT of 26 % [IQR 7 %, 45 %] with an absolute increase in AT of 2.5 ml kg−1 min−1 [IQR 1.1, 3.9] (p = 0.002) and a median increase in pVO2 of 22 % [IQR 11.5, 32.5 %] with an absolute increase in pVO2 of 3.8 ml kg−1 min−1 [IQR 2.0, 5.7] (p < 0.001). Of the non-responders, 19 % of patients did not have a change in AT, and 31 % of patients had a decline (>10 % decline from baseline) of their functional capacity. Responders had a lower baseline AT (9.1 ml kg−1 min−1) and AT/pVO2 ratio (62 %) when compared to the non-responders, who had a higher baseline AT (11.6 ml kg−1 min−1) (p = 0.002) and AT/pVO2 ratio (70 %) (p = 0.002) (Tables 2, 3 and 4). Figure 1 demonstrates a plot of VO2 at AT and peak VO2 at CPX1 and CPX2 in responders and non-responders. There was a median improvement in peak work performed in all patients between CPX1 and CPX2 by 14 % from 100 to 113 W; p = 0.018. Responders had a 19 % increase in peak work from 94 to 115 W; p = 0.024. This improvement was not observed in the non-responder group; p = 0.40 (Tables 2, 3 and 4).
Univariate analyses and multivariable logistic regression were performed to examine for differences in baseline characteristics and determine if there were any predictors of responder vs. non-responder groups. However, there was no statistically significant difference between the baseline characteristics of the responder and non-responder groups (Table 1). Non-responders trended toward suffering more major postoperative complications (Clavien-Dindo classification >3 = 30.8 % in non-responders vs. 0 % in responders; p = 0.096). Responders were less likely to experience complications: Odds ratio = 0.15 (95 % CI 0.00–0.98); p = 0.10 (Table 5). There was no difference in major complication rates between the two sub-groups of non-responders: those that showed ‘no change’ and those who showed a decline in functional capacity during the exercise program.
Responder status could be predicted from CPET-derived variables at CPX1: AT, AT/pVO2 ratio or from variables combined from CPX1 and CPX2: absolute and percentage difference in AT and pVO2, absolute and percentage difference in AT/pVO2 ratio (Table 6). Univariate and multivariate logistic regression did not detect any other predictors of suffering a major complication. All postoperative details and complications are presented in Table 7.
Responders were less likely to have completed their exercise program at home (31 %); in contrast, the majority (69 %) of non-responders completed their exercise programs at home (p = 0.03). In terms of exercise compliance, 77 % of responders and 39 % of non-responders had excellent compliance with their exercise program—defined as completing >80 % of their prescribed exercise, but this was not statistically significant (p = 0.097).
Eleven patients had a third test in between CPX1 and CPX2, of which seven patients had this test after completion of neoadjuvant chemotherapy (nCRT). In these patients, functional capacity showed an insignificant decline following neoadjuvant chemoradiotherapy (AT decreased 5.1 % [IQR −5.9 %, 16.1 %] from 10.4 ± 2.8 to 9.7 ± 1.3 ml kg−1 min−1; p = 0.23 and pVO2 decreased 6.8 % [IQR −3.6 %, 17.2 %] from 15.7 ± 4.6 to 14.7 ± 3.0 ml kg−1 min−1; p = 0.24). A significant improvement in cardiopulmonary fitness was observed from this test when compared to the final presurgical CPET (CPX2) test (AT increased 13.6 % [IQR 4.6 %, 22.7 %] from 9.7 ± 1.3 to 11.4 ± 1.6 ml kg−1 min−1, p < 0.001 and pVO2 increased 11.2 % [IQR 2.7 %, 19.8 %] from 14.7 ± 3.0 to 16.5 ± 3.6 ml kg−1 min−1, p = 0.004).
Discussion
This study adds to the emerging body of evidence that prehabilitation of patients with an exercise program prior to major cancer surgery can improve functional capacity without causing harm [1, 9, 10, 13, 15–18, 24–27]. We have also shown that patients, particularly those in the responder group, have increased their peak work performance. This can be attributed to the success of the exercise program. Using a statistically valid conservative measure of success (10 % increase in AT), this study was able to differentiate responders from non-responders to exercise. Responder’s status could be predicted from CPX1 and CPX2 variables: absolute and percentage difference in AT and absolute and percentage difference in AT/pVO2 ratio (Table 6). An interesting finding of this study was that responders were associated with lower baseline levels of cardiorespiratory fitness—AT (OR = 0.13; 95 % CI 0.01-0.56; p = 0.002) and AT/pVO2 ratio (OR = 0.1; 95 % CI 0.01–0.53; p = 0.002). The reason for this is unclear. It is plausible that more deconditioned patients derived greater benefit from the exercise program, but could also be attributed to yet undiscovered genomic factors [12]. More evident factors include the findings that responders were more likely to have completed their exercise program in a community or hospital environment, rather than at home, with a trend toward improved compliance as potential confounding factors. Previous research has found that patients who exercised at home without supervision had lesser adherence to their exercise program [28]. This supports further work by our team examining the role of technology aids (bluetooth-linked heart rate monitors and smartphone applications [apps]) to assist with real-time monitoring to allow improved supervision of home- and community-based exercise programs.
Patients who responded to exercise showed a trend toward a lower rate of life-threatening postoperative complications, in spite of the observed poorer baseline functional capacity. This may suggest an innate ability to mount a better metabolic response to stress. Poor baseline fitness and impaired chronotropic response to exercise have been shown to predict response to exercise programs in cardiac rehabilitation studies [29]. This concept is further supported by research showing that patients with increased mobilisation of endothelial progenitor cells into their peripheral circulation after exercise were more likely to have a reduced risk of postoperative complications [30]. Our study suggests that patients that are more deconditioned, with lower baseline AT and AT/pVO2 ratio on CPET, are more likely to be responders and may derive more benefit from an exercise program and potentially result in less major complications postoperatively. In a laboratory controlled animal model, non-response to aerobic exercise training was associated with pronounced metabolic dysfunction, insulin resistance and increased inflammatory signalling [31] and may provide an insight into the greater tendency for life-threatening complications in our study patients. Given the ability to identify responder vs. non-responder to exercise, patients predicted to be non-responders should be monitored more closely for postoperative complications, e.g. postoperative care in a high dependency unit (HDU).
This is the first study that has made the differentiation between responders and non-responders to exercise in cancer patients and supports that notion that not all patients respond to exercise in the same manner. The heterogeneity of the population studied makes the results more generalizable to deconditioned surgical patients preoperatively.
Weaknesses of this study include the small sample size and retrospective nature. Validated general performance status tools such as ECOG were not recorded at the time of data collection. As this is a retrospective study, these tools were therefore not able to be included in our analysis. However, ECOG has been included in our data collection for the prospective randomised control trial that we are currently undertaking. In addition, the study was conducted in a single institution, and the majority of patients went to HDU for postoperative care due to the complexity of surgery, rather than medical risk. Although this is allowed for standardised management of patients postoperatively to reduce confounders, it also warrants caution in extrapolating results to practice in other hospitals that may not routinely provide HDU care postoperatively. This study, within a high-risk cancer surgery group, was not adequately powered to identify risk factors for major postoperative complications by univariate and multivariate analysis. Therefore, only observed trends have been discussed to allow future studies to investigate them further.
Cost of medical care increases significantly when patients develop postoperative complications [32]. In addition to studies examining predictors of postoperative outcomes to identify these high risk patients [33], further research should investigate the cost effectiveness of selective referral to prehabilitation exercise program, in conjunction with Accelerated / Enhanced Recovery After Surgery (ERAS) programs [34], as strategies to improve postoperative outcomes and thereby build on delivering the value proposition (value = outcomes/cost) in healthcare. The Metapredict Study currently underway in Europe may provide us with a better understanding of whether biomarkers could be used to predict how humans respond to aerobic and high intensity training (HIT) protocols [35]. The causality and pattern on non-response to exercise also warrant further investigation. Our research group is currently conducting a prospective randomised control trial investigating the effect of prehabilitation on colorectal cancer patients and their outcomes.
Conclusions
Prehabilitation with an individualised exercise program resulted in an overall increase in cardiorespiratory fitness prior to major cancer surgery. However, only 50 % of patients were considered responders to exercise in this study. Although responders were more likely to be deconditioned and have lower AT and AT/pVO2 ratio at their first CPX1, they appeared to have derived more benefit from their exercise program, with more significant improvements in their CPET results and a trend for less major complications postoperatively. Selective referral (based on evaluation by cardiopulmonary exercise testing) of more deconditioned patients to prehabilitation and greater supervision of exercise programs may select for cost effective improvement of patient outcomes.
References
West MA, Loughney L, Lythgoe D, Barben CP, Sripadam R, Kemp GJ et al (2015) Effect of prehabilitation on objectively measured physical fitness after neoadjuvant treatment in preoperative rectal cancer patients: a blinded interventional pilot study. Br J Anaesth 114(2):244–251
Snowden CP, Prentis JM, Anderson HL, Roberts DR, Randles D, Renton M et al (2010) Submaximal cardiopulmonary exercise testing predicts complications and hospital length of stay in patients undergoing major elective surgery. Ann Surg 251(3):535–541
West M, Jack S, Grocott MP (2011) Perioperative cardiopulmonary exercise testing in the elderly. Best Pract Res Clin Anaesthesiol 25(3):427–437
Smith TB, Stonell C, Purkayastha S, Paraskevas P (2009) Cardiopulmonary exercise testing as a risk assessment method in non cardio-pulmonary surgery: a systematic review. Anaesthesia 64(8):883–893
Older P, Hall A, Hader R (1999) Cardiopulmonary exercise testing as a screening test for perioperative management of major surgery in the elderly. Chest 116(2):355–362
Stringer W, Casaburi R, Older P (2012) Cardiopulmonary exercise testing: does it improve perioperative care and outcome? Curr Opin Anaesthesiol 25(2):178–184
West MA, Lythgoe D, Barben CP, Noble L, Kemp GJ, Jack S et al (2014) Cardiopulmonary exercise variables are associated with postoperative morbidity after major colonic surgery: a prospective blinded observational study. Br J Anaesth 112(4):665–671
Wilson RJ, Davies S, Yates D, Redman J, Stone M (2010) Impaired functional capacity is associated with all-cause mortality after major elective intra-abdominal surgery. Br J Anaesth 105(3):297–303
Silver JK, Baima J (2013) Cancer prehabilitation: an opportunity to decrease treatment-related morbidity, increase cancer treatment options, and improve physical and psychological health outcomes. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists 92(8):715–727
Gillis C, Li C, Lee L, Awasthi R, Augustin B, Gamsa A et al (2014) Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology 121(5):937–947
Li C, Carli F, Lee L, Charlebois P, Stein B, Liberman AS et al (2013) Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc 27(4):1072–1082
Bouchard C, Sarzynski MA, Rice TK, Kraus WE, Church TS, Sung YJ et al (2011) Genomic predictors of the maximal O(2) uptake response to standardized exercise training programs. J Appl Physiol 110(5):1160–1170
Jones LW, Liang Y, Pituskin EN, Battaglini CL, Scott JM, Hornsby WE et al (2011) Effect of exercise training on peak oxygen consumption in patients with cancer: a meta-analysis. Oncologist 16(1):112–120
Courneya KS, Sellar CM, Stevinson C, McNeely ML, Peddle CJ, Friedenreich CM et al (2009) Randomized controlled trial of the effects of aerobic exercise on physical functioning and quality of life in lymphoma patients. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 27(27):4605–4612
Courneya KS, Segal RJ, Mackey JR, Gelmon K, Reid RD, Friedenreich CM et al (2007) Effects of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized controlled trial. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 25(28):4396–4404
Segal RJ, Reid RD, Courneya KS, Sigal RJ, Kenny GP, Prud’Homme DG et al (2009) Randomized controlled trial of resistance or aerobic exercise in men receiving radiation therapy for prostate cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 27(3):344–351
Barakat HM, Shahin Y, Barnes R, Gohil R, Souroullas P, Khan J et al (2014) Supervised exercise program improves aerobic fitness in patients awaiting abdominal aortic aneurysm repair. Ann Vasc Surg 28(1):74–79
Kothmann E, Batterham AM, Owen SJ, Turley AJ, Cheesman M, Parry A et al (2009) Effect of short-term exercise training on aerobic fitness in patients with abdominal aortic aneurysms: a pilot study. Br J Anaesth 103(4):505–510
Sinclair RC, Danjoux GR, Goodridge V, Batterham AM (2009) Determination of the anaerobic threshold in the pre-operative assessment clinic: inter-observer measurement error. Anaesthesia 64(11):1192–1195
Kothmann E, Danjoux G, Owen SJ, Parry A, Turley AJ, Batterham AM (2009) Reliability of the anaerobic threshold in cardiopulmonary exercise testing of patients with abdominal aortic aneurysms. Anaesthesia 64(1):9–13
ATS/ACCP (2003) Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 167(2):211–277
American Thoracic S, American College of Chest P (2003) ATS/ACCP statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 167(2):211–277
Hayes SC, Spence RR, Galvao DA, Newton RU (2009) Australian Association for Exercise and Sport Science position stand: optimising cancer outcomes through exercise. Journal of science and medicine in sport / Sports Medicine Australia 12(4):428–434
Jack S, West M, Grocott MP (2011) Perioperative exercise training in elderly subjects. Best Pract Res Clin Anaesthesiol 25(3):461–472
Carli F, Awasthi R, Gillis C, Kassouf W (2014) Optimizing a frail elderly patient for radical cystectomy with a prehabilitation program. Canadian Urological Association journal = Journal de l’Association des urologues du Canada 8(11–12):E884–E887
Arthur HM, Daniels C, McKelvie R, Hirsh J, Rush B (2000) Effect of a preoperative intervention on preoperative and postoperative outcomes in low-risk patients awaiting elective coronary artery bypass graft surgery. A randomized, controlled trial. Ann Intern Med 133(4):253–262
West MA, Parry MG, Lythgoe D, Barben CP, Kemp GJ, Grocott MP et al (2014) Cardiopulmonary exercise testing for the prediction of morbidity risk after rectal cancer surgery. Br J Surg 101(9):1166–1172
Carli F, Charlebois P, Stein B, Feldman L, Zavorsky G, Kim DJ et al (2010) Randomized clinical trial of prehabilitation in colorectal surgery. Br J Surg 97(8):1187–1197
Schmid JP, Zurek M, Saner H (2013) Chronotropic incompetence predicts impaired response to exercise training in heart failure patients with sinus rhythm. European journal of preventive cardiology 20(4):585–592
Schier R, El-Zein R, Cortes A, Liu M, Collins M, Rafat N et al (2014) Endothelial progenitor cell mobilization by preoperative exercise: a bone marrow response associated with postoperative outcome. Br J Anaesth 113(4):652–660
Lessard SJ, Rivas DA, Alves-Wagner AB, Hirshman MF, Gallagher IJ, Constantin-Teodosiu D et al (2013) Resistance to aerobic exercise training causes metabolic dysfunction and reveals novel exercise-regulated signaling networks. Diabetes 62(8):2717–2727
Cologne KG, Hwang GS, Senagore AJ (2014) Cost of practice in a tertiary/quaternary referral center: is it sustainable? Tech Coloproctol 18(11):1035–1039
Hightower CE, Riedel BJ, Feig BW, Morris GS, Ensor JE Jr, Woodruff VD et al (2010) A pilot study evaluating predictors of postoperative outcomes after major abdominal surgery: physiological capacity compared with the ASA physical status classification system. Br J Anaesth 104(4):465–471
Varadhan KK, Neal KR, Dejong CH, Fearon KC, Ljungqvist O, Lobo DN (2010) The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr 29(4):434–440
The metapredict study. Available from: http://www.metapredict.eu/the-metapredict-study/
Acknowledgments
We would like to thank Dr Emma Link, Senior Statistician, Professor Alexander Heriot, Executive Director of Cancer Surgery, Dr John Spillane and Dr Cuong Duong, Surgical Oncology Consultants, Ms Yesim Karabiyik, Respiratory Scientist, and Ms Kay Kenchington, Preadmission Clinic Nurse at Peter MacCallum Cancer Centre, Melbourne, Australia for their assistance with the study.
Financial support and sponsorship
This work was supported by the Peter MacCallum Cancer Foundation and Department of Anaesthesia, Perioperative and Pain Medicine, Peter MacCallum Cancer Centre, Melbourne.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The Peter MacCallum Cancer Centre (PMCC) Human Ethics Research Committee approved this retrospective cohort study (No. 13/44 L). For this type of study, formal consent is not required.
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Grace H. Huang and Hilmy Ismail share joint first authorship on this study.
Rights and permissions
About this article
Cite this article
Huang, G.H., Ismail, H., Murnane, A. et al. Structured exercise program prior to major cancer surgery improves cardiopulmonary fitness: a retrospective cohort study. Support Care Cancer 24, 2277–2285 (2016). https://doi.org/10.1007/s00520-015-3028-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-3028-7