Abstract
Purpose
To investigate the feasibility of conducting a rehabilitation program for patients following surgery for abdomino-pelvic cancer.
Methods
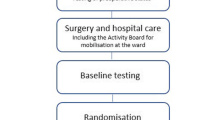
A non-randomised controlled before-and-after study. Patients who had undergone surgery for stage I–III abdomino-pelvic cancer (colorectal, gynaecological or prostate cancer) were recruited. The rehabilitation group (n = 84) received an 8-week, bi-weekly education and exercise program conducted by a physiotherapist, exercise physiologist, health psychologist and dietician, supplemented by exercise diaries and telephone coaching sessions. The comparator group (n = 104) completed postal questionnaires only. Feasibility measures, functional exercise capacity, muscle strength, physical activity levels, pelvic floor symptoms, anxiety and depression, health-related quality of life (HRQoL) and self-efficacy were measured at baseline (time 1), immediately post-intervention (time 2) and at 6 months post-baseline (time 3) and compared within- and between-groups.
Results
The consent rate to the rehabilitation program was 24%. Eighty-one percent of the rehabilitation group attended 85–100% of 16 scheduled sessions. Overall satisfaction with the program was 96%. Functional exercise capacity, handgrip strength in males, bowel symptoms, physical activity levels, depression and HRQoL were significantly improved in the rehabilitation group (p < 0.05) at time 2. The improvements in all these outcomes were sustained at time 3. The rehabilitation group had significantly improved physical activity levels, depression and HRQoL compared with the comparator group at times 2 and 3 (p < 0.05).
Conclusion
Recruitment to this oncology rehabilitation program was more difficult than expected; however, attendance and patient satisfaction were high. This program had positive effects on several important clinical outcomes in patients following abdomino-pelvic cancer treatment.
Trial registration
ANZCTR 12614000580673.

Similar content being viewed by others
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65(2):87–108. https://doi.org/10.3322/caac.21262
Allemani C, Weir HK, Carreira H, Harewood R, Spika D, Wang XS, Bannon F, Ahn JV, Johnson CJ, Bonaventure A, Marcos-Gragera R, Stiller C, Azevedo e Silva G, Chen WQ, Ogunbiyi OJ, Rachet B, Soeberg MJ, You H, Matsuda T, Bielska-Lasota M, Storm H, Tucker TC, Coleman MP, Group CW (2015) Global surveillance of cancer survival 1995-2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet 385(9972):977–1010. https://doi.org/10.1016/S0140-6736(14)62038-9
Geraerts I, Van Poppel H, Devoogdt N, Laenen A, De Groef A, Van Kampen M (2014) Progression and predictors of physical activity levels after radical prostatectomy. BJU Int 114(2):185–192. https://doi.org/10.1111/bju.12465
Lin KY, Edbrooke L, Granger CL, Denehy L, Frawley HC (2018) The impact of gynaecological cancer treatment on physical activity levels: a systematic review of observational studies. Braz J Phys Ther 23:79–92. https://doi.org/10.1016/j.bjpt.2018.11.007
Jefford M, Ward AC, Lisy K, Lacey K, Emery JD, Glaser AW, Cross H, Krishnasamy M, McLachlan SA, Bishop J (2017) Patient-reported outcomes in cancer survivors: a population-wide cross-sectional study. Support care Cancer 25:3171–3179. https://doi.org/10.1007/s00520-017-3725-5
Ramaseshan AS, Felton J, Roque D, Rao G, Shipper AG, Sanses TVD (2018) Pelvic floor disorders in women with gynecologic malignancies: a systematic review. Int Urogynecol J 29(4):459–476. https://doi.org/10.1007/s00192-017-3467-4
Wise J (2017) Urinary incontinence and sexual dysfunction are worse after surgery for prostate cancer, study finds. BMJ 356:j1449. https://doi.org/10.1136/bmj.j1449
Knowles G, Haigh R, McLean C, Phillips HA, Dunlop MG, Din FV (2013) Long term effect of surgery and radiotherapy for colorectal cancer on defecatory function and quality of life. Eur J Oncol Nurs 17(5):570–577. https://doi.org/10.1016/j.ejon.2013.01.010
Schofield C, Newton RU, Cohen PA, Galvao DA, McVeigh JA, Mohan GR, Tan J, Salfinger SG, Straker LM, Peddle-McIntyre CJ (2018) Health-related quality of life and pelvic floor dysfunction in advanced-stage ovarian cancer survivors: associations with objective activity behaviors and physiological characteristics. Support Care Cancer 26(7):2239–2246. https://doi.org/10.1007/s00520-018-4069-5
Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL, Bandera EV, Hamilton KK, Grant B, McCullough M, Byers T, Gansler T (2012) Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin 62(4):243–274. https://doi.org/10.3322/caac.21142
Cheville AL, Mustian K, Winters-Stone K, Zucker DS, Gamble GL, Alfano CM (2017) Cancer rehabilitation: an overview of current need, delivery models, and levels of care. Phys Med Rehabil Clin N Am 28(1):1–17. https://doi.org/10.1016/j.pmr.2016.08.001
Gatta G, Ciccolallo L, Faivre J, Bouvier AM, Berrino F, Gerard JP (2007) Late outcomes of colorectal cancer treatment: a FECS-EUROCARE study. J Cancer Surviv 1(4):247–254. https://doi.org/10.1007/s11764-007-0030-1
Resnick MJ, Koyama T, Fan KH, Albertsen PC, Goodman M, Hamilton AS, Hoffman RM, Potosky AL, Stanford JL, Stroup AM, Van Horn RL, Penson DF (2013) Long-term functional outcomes after treatment for localized prostate cancer. N Engl J Med 368(5):436–445. https://doi.org/10.1056/NEJMoa1209978
Rutledge TL, Heckman SR, Qualls C, Muller CY, Rogers RG (2010) Pelvic floor disorders and sexual function in gynecologic cancer survivors: a cohort study. Am J Obstet Gynecol 203(5):514 e511–514 e517. https://doi.org/10.1016/j.ajog.2010.08.004
Fernandez RA, Garcia-Hermoso A, Solera-Martinez M, Correa MT, Morales AF, Martinez-Vizcaino V (2015) Improvement of continence rate with pelvic floor muscle training post-prostatectomy: a meta-analysis of randomized controlled trials. Urol Int 94(2):125–132. https://doi.org/10.1159/000368618
Lin KY, Granger CL, Denehy L, Frawley HC (2015) Pelvic floor muscle training for bowel dysfunction following colorectal cancer surgery: a systematic review. Neurourol Urodyn 34(8):703–712. https://doi.org/10.1002/nau.22654
Des Jarlais DC, Lyles C, Crepaz N, Group T (2004) Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health 94(3):361–366
Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, Lancaster GA, group Pc (2016) CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 355:i5239. https://doi.org/10.1136/bmj.i5239
Slade SC, Dionne CE, Underwood M, Buchbinder R (2016) Consensus on exercise reporting template (CERT): explanation and elaboration statement. Br J Sports Med 50:1428–1437. https://doi.org/10.1136/bjsports-2016-096651
Muyor JM (2013) Exercise intensity and validity of the ratings of perceived exertion (Borg and OMNI scales) in an indoor cycling session. J Hum Kinet 39:93–101. https://doi.org/10.2478/hukin-2013-0072
ATS statement: guidelines for the six-minute walk test (2002). Am J Respir Crit Care Med 166 (1):111–117. https://doi.org/10.1164/ajrccm.166.1.at1102
Spencer LM, Alison JA, McKeough ZJ (2008) Six-minute walk test as an outcome measure: are two six-minute walk tests necessary immediately after pulmonary rehabilitation and at three-month follow-up? Am J Phys Med Rehabil 87(3):224–228. https://doi.org/10.1097/PHM.0b013e3181583e66
Peolsson A, Hedlund R, Oberg B (2001) Intra- and inter-tester reliability and reference values for hand strength. J Rehabil Med 33(1):36–41
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395. https://doi.org/10.1249/01.MSS.0000078924.61453.FB
Vodermaier A, Millman RD (2011) Accuracy of the Hospital Anxiety and Depression Scale as a screening tool in cancer patients: a systematic review and meta-analysis. Support Care Cancer 19(12):1899–1908. https://doi.org/10.1007/s00520-011-1251-4
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
Schwarzer R, Renner B (2005) Health-specific self-efficacy scales. http://userpage.fu-berlin.de/health/healself.pdf
Baessler K, O'Neill SM, Maher CF, Battistutta D (2009) Australian pelvic floor questionnaire: a validated interviewer-administered pelvic floor questionnaire for routine clinic and research. Int Urogynecol J Pelvic Floor Dysfunct 20(2):149–158. https://doi.org/10.1007/s00192-008-0742-4
Lin KY, Frawley HC, Granger CL, Denehy L (2016) The Australian Pelvic Floor Questionnaire is a valid measure of pelvic floor symptoms in patients following surgery for colorectal cancer. Neurourol Urodyn 36:1395–1402. https://doi.org/10.1002/nau.23122
Cotterill N, Norton C, Avery KN, Abrams P, Donovan JL (2011) Psychometric evaluation of a new patient-completed questionnaire for evaluating anal incontinence symptoms and impact on quality of life: the ICIQ-B. Dis Colon Rectum 54(10):1235–1250. https://doi.org/10.1097/DCR.0b013e3182272128
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P (2004) ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn 23(4):322–330. https://doi.org/10.1002/nau.20041
Teare MD, Dimairo M, Shephard N, Hayman A, Whitehead A, Walters SJ (2014) Sample size requirements to estimate key design parameters from external pilot randomised controlled trials: a simulation study. Trials 15:264. https://doi.org/10.1186/1745-6215-15-264
Li C, Carli F, Lee L, Charlebois P, Stein B, Liberman AS, Kaneva P, Augustin B, Wongyingsinn M, Gamsa A, Kim do J, Vassiliou MC, Feldman LS (2013) Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc 27(4):1072–1082. https://doi.org/10.1007/s00464-012-2560-5
Koutoukidis DA, Beeken RJ, Lopes S, Knobf MT, Lanceley A (2016) Attitudes, challenges and needs about diet and physical activity in endometrial cancer survivors: a qualitative study. Eur J Cancer Care 26. https://doi.org/10.1111/ecc.12531
Adams RN, Mosher CE, Blair CK, Snyder DC, Sloane R, Demark-Wahnefried W (2015) Cancer survivors’ uptake and adherence in diet and exercise intervention trials: an integrative data analysis. Cancer 121(1):77–83. https://doi.org/10.1002/cncr.28978
Courneya KS, Vardy J, Gill S, Jonker D, O’Brien P, Friedenreich CM, Dhillon H, Wong RKS, Meyer RM, Crawford JJ, Campbell KL, Prapavessis H, O’Callaghan C, Turner J, Spencer L, van der Ploeg H, Tu D, Booth CM (2014) Update on the colon health and life-long exercise change trial: a phase III study of the impact of an exercise program on disease-free survival in colon cancer survivors. Curr Color Cancer Rep 10:321–328. https://doi.org/10.1007/s11888-014-0231-8
Leira EC, Viscoli CM, Polgreen LA, Gorman M, Kernan WN, on behalf of the ITI (2018) Distance from home to research center: a barrier to in-person visits but not treatment adherence in a stroke trial. Neuroepidemiology 50(3–4):137–143. https://doi.org/10.1159/000486315
Bourke L, Smith D, Steed L, Hooper R, Carter A, Catto J, Albertsen PC, Tombal B, Payne HA, Rosario DJ (2016) Exercise for men with prostate cancer: a systematic review and meta-analysis. Eur Urol 69(4):693–703. https://doi.org/10.1016/j.eururo.2015.10.047
Shingler E, Hackshaw-McGeagh L, Robles L, Persad R, Koupparis A, Rowe E, Shiridzinomwa C, Bahl A, Martin RM, Lane JA (2017) The feasibility of the prostate cancer: evidence of exercise and nutrition trial (PrEvENT) dietary and physical activity modifications: a qualitative study. Trials 18. https://doi.org/10.1186/s13063-017-1828-4
Dennett AM, Peiris CL, Shields N, Morgan D, Taylor NF (2017) Exercise therapy in oncology rehabilitation in Australia: a mixed-methods study. Asia-Pac J Clin Oncol 13(5):E515–E527. https://doi.org/10.1111/ajco.12642
Gerritsen JK, Vincent AJ (2016) Exercise improves quality of life in patients with cancer: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med 50(13):796–803. https://doi.org/10.1136/bjsports-2015-094787
Sweegers MG, Altenburg TM, Chinapaw MJ, Kalter J, Verdonck-de Leeuw IM, Courneya KS, Newton RU, Aaronson NK, Jacobsen PB, Brug J, Buffart LM (2017) Which exercise prescriptions improve quality of life and physical function in patients with cancer during and following treatment? A systematic review and meta-analysis of randomised controlled trials. Br J Sports Med 52:505–513. https://doi.org/10.1136/bjsports-2017-097891
Lin KY, Frawley HC, Denehy L, Feil D, Granger CL (2016) Exercise interventions for patients with gynaecological cancer: a systematic review and meta-analysis. Physiotherapy 102(4):309–319. https://doi.org/10.1016/j.physio.2016.02.006
Cramer H, Lauche R, Klose P, Dobos G, Langhorst J (2014) A systematic review and meta-analysis of exercise interventions for colorectal cancer patients. Eur J Cancer Care 23(1):3–14. https://doi.org/10.1111/ecc.12093
Bohannon RW, Crouch R (2017) Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: a systematic review. J Eval Clin Pract 23(2):377–381. https://doi.org/10.1111/jep.12629
Morgan AL, Tobar DA, Snyder L (2010) Walking toward a new me: the impact of prescribed walking 10,000 steps/day on physical and psychological well-being. J Phys Act Health 7(3):299–307
Costa ALS, Heitkemper MM, Alencar GP, Damiani LP, Silva RMD, Jarrett ME (2017) Social support is a predictor of lower stress and higher quality of life and resilience in Brazilian patients with colorectal cancer. Cancer Nurs 40(5):352–360. https://doi.org/10.1097/NCC.0000000000000388
Acknowledgements
The authors would like to thank the participants, participating surgeons and the staff from Cabrini Health and the Centre for Allied Health Research and Education at Cabrini Institute for their contribution and assistance to the study. This study was supported by grant funding from the Cabrini Foundation and Cabrini Allied Health Department, Victoria, Australia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest. The authors have full control of all primary data and agree to allow the journal to review their data if requested.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 55 kb)
Rights and permissions
About this article
Cite this article
Frawley, H.C., Lin, KY., Granger, C.L. et al. An allied health rehabilitation program for patients following surgery for abdomino-pelvic cancer: a feasibility and pilot clinical study. Support Care Cancer 28, 1335–1350 (2020). https://doi.org/10.1007/s00520-019-04931-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04931-w