Abstract
Background
Breast cancer remains the most frequently diagnosed malignancy among women worldwide, with rising incidence numbers. In Belgium, one out of eight women will be diagnosed with breast cancer. Fortunately, 80% of those breast cancer patients will still be alive 10 years after diagnosis due to improvements in screening and treatment strategies. However, an important portion of the breast cancer survivors (BCS) will face side effects, such as sleep disturbances, long after treatment ends. It has been demonstrated that untreated insomnia in BCS negatively impacts mood, physical symptoms, pain sensitivity, fatigue, and quality of life. Furthermore, insomnia is increasingly considered an independent risk factor for future depression in BCS. The importance of understanding sleep disturbances in cancer populations has been highlighted and recognized as warranting further research. Therefore, the purpose of this systematic review was to determine the prevalence and the risk factors for the development of sleep disturbances in BCS.
Methods
PubMed, Web of Science, and PEDro were systematically screened for studies encompassing data regarding the prevalence or risk factors of sleep disturbances in BCS. If possible, meta-analyses were performed. Subgroup analyses were undertaken based on the methodological quality, study design, type of sleep disturbance, and the use of a measurement tool with strong psychometric properties to investigate significant heterogeneity (I2 > 50%) across studies.
Results
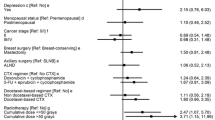
A total of 27 studies were found eligible. The pooled estimate for sleep disturbances prevalence is 0.40 (95% confidence interval (CI) = [0.29–0.52], I2 = 100%, p < 0.00001) and ranged from 0.14 (95% CI = [0.04–0.24]) to 0.93 (95% CI = [0.91–0.95]). Subgroup analyses did not reduce the heterogeneity among studies. Meta-analyses were performed for seven risk factors. Significant differences for the odds of developing sleep disturbances were found for hot flashes (pooled OR (ORp) 2.25, 95% CI = [1.64–3.08], I2 = 0%, p = 0.90), race (ORp 2.31, 95% CI = [1.56–3.42], I2 = 0%, p = 0.47), and menopause (ORp 1.84, 95% CI = [1.11–3.06], I2 = 0%, p = 0.70). After withdrawing the studies that did not rely on the use of a measurement tool with strong psychometric properties, pain (ORp 2.31, 95% CI = [1.36–3.92], I2 = 27%, p = 0.25), depressive symptoms (ORp 3.20, 95% CI [2.32–4.42], I2 = 0%, p = 0.63), and fatigue (ORp 2.82, 95% CI = [1.98–4.02], I2 = 0%, p = 0.60) became significant as well, with a substantial decrease of heterogeneity.
Conclusion
Prevalence for sleep disturbances ranged from 0.14 to 0.93 with the vast majority of the studies investigating insomnia and sleep-wake disturbances. High heterogeneity makes it difficult to draw firm conclusions. Pain, depressive symptoms, hot flashes, fatigue, non-Caucasian race, and menopausal status were significantly associated with increased odds for developing sleep disturbances.


Similar content being viewed by others
References
Fitzmaurice C et al (2016) Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol
Coleman MP, Quaresma M, Berrino F, Lutz JM, de Angelis R, Capocaccia R, Baili P, Rachet B, Gatta G, Hakulinen T, Micheli A, Sant M, Weir HK, Elwood JM, Tsukuma H, Koifman S, E Silva GA, Francisci S, Santaquilani M, Verdecchia A, Storm HH, Young JL, CONCORD Working Group (2008) Cancer survival in five continents: a worldwide population-based study (CONCORD). Lancet Oncol 9(8):730–756
Roth T (2007) Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med 3(5 Suppl):S7–S10
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders-IV-TR. American Psychiatric Association, Washington, DC
Colten H, Altevogt B (2006) Sleep disorders and sleep deprivation: an unmet public health problem, vol 2007. National Academies Press, Washington, DC
Janz NK et al (2007) Symptom experience and quality of life of women following breast cancer treatment. J Womens Health 16(9):1348–1361
Reinsel RA, Starr TD, O'Sullivan B, Passik SD, Kavey NB (2015) Polysomnographic study of sleep in survivors of breast Cancer. J Clin Sleep Med 11(12):1361–1370
Jim HS et al (2013) Lagged relationships among sleep disturbance, fatigue, and depressed mood during chemotherapy. Health Psychol 32(7):768–774
Daley M et al (2009) The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep 32(1):55–64
Morin CM (1993) Insomnia: psychological assessment and management. Guilford Press
Savard J et al (2001) Prevalence, clinical characteristics, and risk factors for insomnia in the context of breast cancer. Sleep 24(5):583–590
Hoffman KE et al (2009) Psychological distress in long-term survivors of adult-onset cancer: results from a national survey. Arch Intern Med 169(14):1274–1281
Ness S, Kokal J, Fee-Schroeder K, Novotny P, Satele D, Barton D (2013) Concerns across the survivorship trajectory: results from a survey of cancer survivors. Oncol Nurs Forum 40(1):35–42
Waters EA et al (2013) Worry about cancer progression and low perceived social support: implications for quality of life among early-stage breast cancer patients. Ann Behav Med 45(1):57–68
Berrett-Abebe J et al (2015) Exploring the relationship between fear of cancer recurrence and sleep quality in cancer survivors. J Psychosoc Oncol 33(3):297–309
Irvine DM, Vincent L, Graydon JE, Bubela N (1998) Fatigue in women with breast cancer receiving radiation therapy. Cancer Nurs 21(2):127–135
Palesh OG, Roscoe JA, Mustian KM, Roth T, Savard J, Ancoli-Israel S, Heckler C, Purnell JQ, Janelsins MC, Morrow GR (2010) Prevalence, demographics, and psychological associations of sleep disruption in patients with Cancer: University of Rochester Cancer Center–Community Clinical Oncology Program. J Clin Oncol 28(2):292–298
Liberati A et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1–e34
Office of Cancer Survivorship, NCI About cancer survivorship research: survivorship definitions. 2012. Available from: http://cancercontrol.cancer.gov/ocs/researcher_factsheet.pdf
Elmagarmid A et al (2014) Rayyan: a systematic reviews web app for exploring and filtering searches for eligible studies for Cochrane Reviews. In: Evidence-informed public health: opportunities and challenges. Abstracts of the 22nd Cochrane Colloquium. Wiley, Hyderabad
Green, S., et al., Chapter 1: what is a systematic review. Cochrane handbook for systematic reviews of interventions version, 2008. 5(0)
Dahl AA et al (2011) Arm/shoulder problems and insomnia symptoms in breast cancer survivors: cross-sectional, controlled and longitudinal observations. Sleep Med 12(6):584–590
Kim SH et al (2008) Fatigue and depression in disease-free breast cancer survivors: prevalence, correlates, and association with quality of life. J Pain Symptom Manag 35(6):644–655
Klyushnenkova EN, Sorkin JD, Gallicchio L (2015) Association of obesity and sleep problems among breast cancer survivors: results from a registry-based survey study. Support Care Cancer 23(12):3437–3445
Otte JL et al (2010) Prevalence, severity, and correlates of sleep-wake disturbances in long-term breast cancer survivors. J Pain Symptom Manag 39(3):535–547
Modesti PA et al (2016) Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One 11(1):e0147601
McPheeters ML et al (2012) Closing the quality gap: revisiting the state of the science (vol. 3: quality improvement interventions to address health disparities). Evid Rep Technol Assess (Full Rep) (208.3):1–475
Higgins JP et al (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Deeks JJ, Higgins J, Altman DG (2008) Analysing data and undertaking meta-analyses. In: Cochrane handbook for systematic reviews of interventions: Cochrane book series, pp 243–296
Bao T, Basal C, Seluzicki C, Li SQ, Seidman AD, Mao JJ (2016) Long-term chemotherapy-induced peripheral neuropathy among breast cancer survivors: prevalence, risk factors, and fall risk. Breast Cancer Res Treat 159(2):327–333
Desai K, Mao JJ, Su I, DeMichele A, Li Q, Xie SX, Gehrman PR (2013) Prevalence and risk factors for insomnia among breast cancer patients on aromatase inhibitors. Support Care Cancer 21(1):43–51
Ahn SH et al (2007) Health-related quality of life in disease-free survivors of breast cancer with the general population. Ann Oncol 18(1):173–182
Alfano CM, Lichstein KL, Vander Wal GS, Smith AW, Reeve BB, McTiernan A, Bernstein L, Baumgartner KB, Ballard-Barbash R (2011) Sleep duration change across breast cancer survivorship: associations with symptoms and health-related quality of life. Breast Cancer Res Treat 130(1):243–254
Arraras JI et al (2016) Quality of life in long-term premenopausal early-stage breast cancer survivors from Spain. Effects of surgery and time since surgery. J Buon 21(5):1090–1098
Berger AM et al (2012) Usual and worst symptom severity and interference with function in breast cancer survivors. J Support Oncol 10(3):112–118
Couzi RJ, Helzlsouer KJ, Fetting JH (1995) Prevalence of menopausal symptoms among women with a history of breast cancer and attitudes toward estrogen replacement therapy. J Clin Oncol 13(11):2737–2744
Forsythe L et al (2012) Daytime sleepiness and sleep duration in long-term cancer survivors and non-cancer controls: results from a registry-based survey study. Support Care Cancer 20(10):2425–2432
Gonzalez BD, Lu Q (2018) Sleep disturbance among Chinese breast cancer survivors living in the USA. Support Care Cancer 26(6):1695–1698
Heins MJ et al (2013) For which health problems do cancer survivors visit their general practitioner? Eur J Cancer 49(1):211–218
Kluthcovsky A et al (2012) Fatigue after treatment in breast cancer survivors: prevalence, determinants and impact on health-related quality of life. Support Care Cancer 20(8):1901–1909
Lee ES et al (2011) Health-related quality of life in survivors with breast cancer 1 year after diagnosis compared with the general population a prospective cohort study. Ann Surg 253(1):101–108
Lowery-Allison AE et al (2017) Sleep problems in breast cancer survivors 1-10 years posttreatment. Palliat Support Care:1–10
Marinac CR, Nelson SH, Flatt SW, Natarajan L, Pierce JP, Patterson RE (2017) Sleep duration and breast cancer prognosis: perspectives from the Women's healthy eating and living study. Breast Cancer Res Treat 162(3):581–589
Orre IJ, Reinertsen KV, Aukrust P, Dahl AA, Fosså SD, Ueland T, Murison R (2011) Higher levels of fatigue are associated with higher CRP levels in disease-free breast cancer survivors. J Psychosom Res 71(3):136–141
Palmer SC et al (2016) Symptoms, unmet need, and quality of life among recent breast cancer survivors. J Community Support Oncol 14(7):299–306
Schultz PN et al (2005) Breast cancer: relationship between menopausal symptoms, physiologic health effects of cancer treatment and physical constraints on quality of life in long-term survivors. J Clin Nurs 14(2):204–211
Servaes P, Verhagen S, Bleijenberg G (2002) Determinants of chronic fatigue in disease-free breast cancer patients: a cross-sectional study. Ann Oncol 13(4):589–598
Taylor TR et al (2012) Understanding sleep disturbances in African-American breast cancer survivors: a pilot study. Psycho-Oncology 21(8):896–902
Yang EJ, Kim BR, Shin HI, Lim JY (2012) Use of the international classification of functioning, disability and health as a functional assessment tool for breast cancer survivors. J Breast Cancer 15(1):43–50
Zucca AC, Boyes AW, Linden W, Girgis A (2012) All's well that ends well? Quality of life and physical symptom clusters in long-term cancer survivors across cancer types. J Pain Symptom Manag 43(4):720–731
Sateia MJ (2014) International classification of sleep disorders-third edition: highlights and modifications. Chest 146(5):1387–1394
Fiorentino L, Ancoli-Israel S (2006) Insomnia and its treatment in women with breast cancer. Sleep Med Rev 10(6):419–429
Savard J, Morin CM (2001) Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol 19(3):895–908
Palesh O, Aldridge-Gerry A, Zeitzer JM, Koopman C, Neri E, Giese-Davis J, Jo B, Kraemer H, Nouriani B, Spiegel D (2014) Actigraphy-measured sleep disruption as a predictor of survival among women with advanced breast cancer. Sleep 37(5):837–842
Galiano-Castillo N, Arroyo-Morales M, Ariza-Garcia A, Fernández-Lao C, Fernández-Fernández AJ, Cantarero-Villanueva I (2017) Factors that explain the cancer-related insomnia. Breast J 23(4):387–394
Jansson-Frojmark M, Lindblom K (2008) A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res 64(4):443–449
Morphy H et al (2007) Epidemiology of insomnia: a longitudinal study in a UK population. Sleep 30(3):274–280
Johnson EO, Roth T, Breslau N (2006) The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res 40(8):700–708
Ohayon MM, Roth T (2003) Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res 37(1):9–15
Carpenter JS, Elam JL, Ridner SH, Carney PH, Cherry GJ, Cucullu HL (2004) Sleep, fatigue, and depressive symptoms in breast cancer survivors and matched healthy women experiencing hot flashes. Oncol Nurs Forum 31(3):591–5598
Ford DE, Kamerow DB (1989) Epidemiologic study of sleep disturbances and psychiatric disorders: an opportunity for prevention? Jama 262(11):1479–1484
Ell K et al (2005) Depression, correlates of depression, and receipt of depression care among low-income women with breast or gynecological cancer. J Clin Oncol Off J Am Soc Clin Oncol 23(13):3052
Forsythe LP, Alfano CM, George SM, McTiernan A, Baumgartner KB, Bernstein L, Ballard-Barbash R (2013) Pain in long-term breast cancer survivors: the role of body mass index, physical activity, and sedentary behavior. Breast Cancer Res Treat 137(2):617–630
Anders CK et al (2009) Breast cancer before age 40 years. Semin Oncol 36(3):237–249
Partridge A, Gelber S, Gelber RD, Castiglione-Gertsch M, Goldhirsch A, Winer E (2007) Age of menopause among women who remain premenopausal following treatment for early breast cancer: long-term results from international breast Cancer study group trials V and VI. Eur J Cancer 43(11):1646–1653
Rapkin AJ (2007) Vasomotor symptoms in menopause: physiologic condition and central nervous system approaches to treatment. Am J Obstet Gynecol 196(2):97–106
Kronenberg F (1990) Hot flashes: epidemiology and physiologya. Ann N Y Acad Sci 592(1):52–86
Morales L, Neven P, Timmerman D, Christiaens MR, Vergote I, van Limbergen E, Carbonez A, van Huffel S, Ameye L, Paridaens R (2004) Acute effects of tamoxifen and third-generation aromatase inhibitors on menopausal symptoms of breast cancer patients. Anti-Cancer Drugs 15(8):753–760
Abrahams HJG, Gielissen MFM, Verhagen CAHHVM, Knoop H (2018) The relationship of fatigue in breast cancer survivors with quality of life and factors to address in psychological interventions: a systematic review. Clin Psychol Rev 63:1–11
Rumble ME, Keefe FJ, Edinger JD, Affleck G, Marcom PK, Shaw HS (2010) Contribution of cancer symptoms, dysfunctional sleep related thoughts, and sleep inhibitory behaviors to the insomnia process in breast Cancer survivors: a daily process analysis. Sleep 33(11):1501–1509
Dudley KA, Patel SR (2016) Disparities and genetic risk factors in obstructive sleep apnea. Sleep Med 18:96–102
Beatty DL, Hall MH, Kamarck TA, Buysse DJ, Owens JF, Reis SE, Mezick EJ, Strollo PJ, Matthews KA (2011) Unfair treatment is associated with poor sleep in African American and Caucasian adults: Pittsburgh SleepSCORE project. Health Psychol 30(3):351–359
Hall M, Bromberger J, Matthews K (1999) Socioeconomic status as a correlate of sleep in African-American and Caucasian women. Ann N Y Acad Sci 896(1):427–430
Jüni P et al (2002) Direction and impact of language bias in meta-analyses of controlled trials: empirical study. Int J Epidemiol 31(1):115–123
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have full control of all data acquired from included manuscripts and agree to allow the journal to review the data if requested.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Laurence Leysen and Astrid Lahousse share first authorship
Appendices
Appendix 1
Appendix 2
Appendix 3: Methodological quality
Appendix 4: Study design
Appendix 5: Type of sleep disturbance
Appendix 6
Appendix 7: Pain
Appendix 8: Depressive symptoms
Appendix 9
Appendix 10: Fatigue
Appendix 11
Appendix 12
Appendix 13
Rights and permissions
About this article
Cite this article
Leysen, L., Lahousse, A., Nijs, J. et al. Prevalence and risk factors of sleep disturbances in breast cancersurvivors: systematic review and meta-analyses. Support Care Cancer 27, 4401–4433 (2019). https://doi.org/10.1007/s00520-019-04936-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04936-5