Abstract
Purpose
To assess the impact of a pathway allowing nurse initiation of first dose intravenous (IV) antibiotics on time to antibiotic administration (TTA) in adult inpatients with febrile neutropenia (FN).
Methods
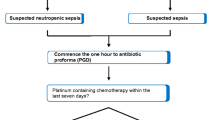
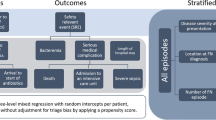
This study evaluated the impact on TTA of a clinical pathway (November 2017 to April 2018) allowing nurse initiation of pre-prescribed antibiotics in adult haematology patients with FN, compared with a prior cohort (November 2016 to April 2017) in which antibiotics were only prescribed and administered after medical review. The primary endpoint for comparison was TTA, calculated as the time between the first recorded fever and IV antibiotic administration. Secondary endpoints included appropriateness of initial antibiotic choice, 30-day all-cause mortality and admission to intensive care unit (ICU).
Results
Forty-seven eligible FN episodes in 40 patients and 61 episodes in 52 patients were evaluated in the pre- and post-implementation groups, respectively. Baseline characteristics were comparable between groups. Median (IQR) TTA, in the pre-implementation group [66 min (40–100 min)] was significantly prolonged versus post-implementation group [29 min (20–41 min); p < 0.001]. A significantly higher proportion of episodes were administered appropriate initial antibiotics in the post-versus pre-implementation groups (100% vs. 89%, p = 0.03). There was no significant change in 30-day all-cause mortality (0% vs. 5%, p = 0.3) or ICU admission within 48 h of fever (0% vs. 2%, p > 0.99) between pre- and post-implementation groups, respectively.
Conclusions
A pathway allowing nurse initiation of pre-prescribed antibiotic orders for FN significantly reduced TTA from first recorded fever and increased the proportion of appropriate initial antibiotic choices without significantly impacting on patient outcomes.

Similar content being viewed by others
References
Tam CS, O'Reilly M, Andresen D, Lingaratnam S, Kelly A, Burbury K, Turnidge J, Slavin MA, Worth LJ, Dawson L, Thursky KA (2011) Use of empiric antimicrobial therapy in neutropenic fever. Australian consensus guidelines 2011 steering committee. Intern Med J 41:90–101
Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, Raad II, Rolston KV, Young JA, Wingard JR (2011) Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of America. Clin Infect Dis 52:56–93
Klastersky J, de Naurois J, Rolston K, Rapoport B, Maschmeyer G, Aapro M, Herrstedt J (2016) Management of febrile neutropaenia: ESMO clinical practice guidelines. Ann Oncol 27:111–118
van Vliet M, Potting CM, Sturm PD, Donnelly JP, Blijlevens NM (2011) How prompt is prompt in daily practice? Earlier initiation of empirical antibacterial therapy for the febrile neutropenic patient. Eur J Cancer Care (Engl) 20:679–685
Wells T, Thomas C, Watt D, Fountain V, Tomlinson M, Hilman S (2015) Improvements in the management of neutropenic sepsis: lessons learned from a district general hospital. Clin Med (Lond) 15:526–530
Meisenberg B, Clemons J, Ness J, Faust N, Clance M (2015) Improving hospital performance in the treatment of febrile neutropenia. Support Care Cancer 23:371–375
Ko HF, Tsui SS, Tse JW, Kwong WY, Chan OY, Wong GC (2015) Improving the emergency department management of post-chemotherapy sepsis in haematological malignancy patients. Hong Kong Med J 21:10–15
Mattison G, Bilney M, Haji-Michael P, Cooksley T (2016) A nurse-led protocol improves the time to first dose intravenous antibiotics in septic patients post chemotherapy. Support Care Cancer 24:5001–5005
Forde C, Scullin P (2017) Chasing the Golden Hour - Lessons learned from improving initial neutropenic sepsis management BMJ Qual Improv Rep 6
Keng MK, Thallner EA, Elson P, Ajon C, Sekeres J, Wenzell CM, Seastone DJ, Gallagher EM, Weber CM, Earl MA, Mukherjee S, Pohlman B, Cober E, Foster VB, Yuhas J, Kalaycio ME, Bolwell BJ, Sekeres MA (2015) Reducing time to antibiotic administration for febrile neutropenia in the emergency department. J Oncol Pract 11:450–455
Clarke RT, Warnick J, Stretton K, Littlewood TJ (2011) Improving the immediate management of neutropenic sepsis in the UK: lessons from a national audit. Br J Haematol 153:773–779
Grigg S, Date P, Goodall E, Grigg A (2017) Reducing time to antibiotics in febrile neutropenia. HAA Annual Scientific Meeting, Sydney, Australia
World Health Organisation (1979) Handbook for report results of cancer treatment. In: Handbook for reporting results of cancer treatment. https://apps.who.int/iris/handle/10665/37200. Accessed 20 October 2019
Averbuch D, Orasch C, Cordonnier C, Livermore DM, Mikulska M, Viscoli C, Gyssens IC, Kern WV, Klyasova G, Marchetti O, Engelhard D, Akova M (2013) European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European conference on infections in leukemia. Haematologica 98:1826–1835
Ortega M, Marco F, Soriano A, Almela M, Martinez JA, Munoz A, Mensa J (2009) Analysis of 4758 Escherichia coli bacteraemia episodes: predictive factors for isolation of an antibiotic-resistant strain and their impact on the outcome. J Antimicrob Chemother 63:568–574
Trecarichi EM, Tumbarello M, Spanu T, Caira M, Fianchi L, Chiusolo P, Fadda G, Leone G, Cauda R, Pagano L (2009) Incidence and clinical impact of extended-spectrum-beta-lactamase (ESBL) production and fluoroquinolone resistance in bloodstream infections caused by Escherichia coli in patients with hematological malignancies. J Inf Secur 58:299–307
Paul M, Yahav D, Bivas A, Fraser A, Leibovici L (2010) Anti-pseudomonal beta-lactams for the initial, empirical, treatment of febrile neutropenia: comparison of beta-lactams. Cochrane database Syst rev: Cd005197
Ferrer R, Martin-Loeches I, Phillips G, Osborn TM, Townsend S, Dellinger RP, Artigas A, Schorr C, Levy MM (2014) Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med 42:1749–1755
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, Gurka D, Kumar A, Cheang M (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 34:1589–1596
Sterling SA, Miller WR, Pryor J, Puskarich MA, Jones AE (2015) The impact of timing of antibiotics on outcomes in severe sepsis and septic shock: a systematic review and meta-analysis. Crit Care Med 43:1907–1915
Rosa RG, Goldani LZ (2014) Cohort study of the impact of time to antibiotic administration on mortality in patients with febrile neutropenia. Antimicrob Agents Chemother 58:3799–3803
Perron T, Emara M, Ahmed S (2014) Time to antibiotics and outcomes in cancer patients with febrile neutropenia. BMC Health Serv Res 14:162
Daniels LM, Durani U, Barreto JN, O'Horo JC, Siddiqui MA, Park JG, Tosh PK (2019) Impact of time to antibiotic on hospital stay, intensive care unit admission, and mortality in febrile neutropenia. Support Care Cancer 27(11):4171–4177
Thursky K, Lingaratnam S, Jayarajan J, Haeusler GM, Teh B, Tew M, Venn G, Hiong A, Brown C, Leung V, Worth LJ, Dalziel K, Slavin MA (2018) Implementation of a whole of hospital sepsis clinical pathway in a cancer hospital: impact on sepsis management, outcomes and costs. BMJ Open Qual 7:e000355
Chen AX, Simpson SQ, Pallin DJ (2019) Sepsis Guidelines. N Engl J Med 380:1369–1371
Keng MK, Sekeres MA (2013) Febrile neutropenia in hematologic malignancies. Curr Hematol Malig Rep 8:370–378
Zimmer AJ, Freifeld AG (2019) Optimal management of neutropenic fever in patients with Cancer. J Oncol Pract 15:19–24
Family L, Li Y, Chen LH, Page JH, Klippel ZK, Chao C (2018) A study of novel febrile neutropenia risk factors related to bone marrow or immune suppression, barrier function, and bacterial Flora. J Natl Compr Cancer Netw 16:1201–1208
Pillinger KE, Bouchard J, Withers ST, Mediwala K, McGee EU, Gibson GM, Bland CM, Bookstaver PB (2019) Inpatient antibiotic stewardship interventions in the adult oncology and hematopoietic stem cell transplant population: a review of the literature. Ann Pharmacother 00(0): 1–17
Acknowledgements
The authors would like to acknowledge Patrick Date for his contribution to the collection of preliminary audit data (12/1/2011 to 4/12/2015).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Steven T Walker and Samuel Grigg. The first draft of the manuscript was written by Steven T Walker, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The authors have full control of all primary data and agree to allow the journal to review this data if requested.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
Walker, S.T., Grigg, S., Kirkpatrick, C. et al. Nurse-initiated pre-prescribed antibiotic orders to facilitate prompt and appropriate antibiotic administration in febrile neutropenia. Support Care Cancer 28, 4337–4343 (2020). https://doi.org/10.1007/s00520-019-05290-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05290-2