Abstract
Purpose
Given the high survival rate of cervical cancer patients, understanding women’s health-related quality of life (HRQL) during and after treatment is of major clinical importance. We conducted a systematic review to synthesize all available evidence about the effects of each contemporary treatment modality for cervical cancer on all dimensions of women’s HRQL, including symptoms, functioning, and global HRQL.
Methods
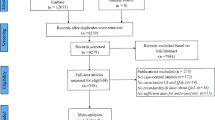
We searched four electronic databases from January 2000 to September 2019, cross-referenced and searched by author name for studies of patients treated for cervical cancer that reported patient-reported outcomes (PROs) before treatment and with at least one post-treatment measurement. Two independent reviewers applied inclusion and quality criteria and extracted findings. Studies were categorized by treatment to determine specific treatment effects on PROs. Results were narratively summarized.
Results
We found twenty-nine papers reporting 23 studies. After treatments with curative intent for early or locally advanced disease, lymphedema, diarrhea, menopausal symptoms, tight and shorter vagina, pain during intercourse, and sexual worries remained long-term problems; however, sexual activity improved over time. HRQL and psychological distress were impacted during treatment with also worsening of global HRQL but improved 3–6 months after treatment. In patients with metastatic or recurrent disease, pain improved during palliative treatment or remained stable, with no differences in global HRQL found over time.
Conclusion
Whereas most symptoms worsen during treatment and improve in the first 3 months after completing treatment, symptoms like lymphedema, menopausal symptoms, and sexual worries develop gradually and persist after curative treatment. These findings can be used to inform clinical practice and facilitate communication and shared decision-making. More research is needed in very early cervical cancer and the impact of fertility sparing therapy on PROs.





Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Noone AM, H N, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds) (2018) SEER Cancer Statistics Review, 1975-2015, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2015/, based on November 2017 SEER data submission, posted to the SEER web site
Marth C et al (2017) Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol 28(suppl_4):iv72–iv83
Cohen PA, Jhingran A, Oaknin A, Denny L (2019) Cervical cancer. Lancet 393(10167):169–182
Bhatla N et al (2018) Cancer of the cervix uteri. Int J Gynaecol Obstet 143(Suppl 2):22–36
Bhatla N et al (2019) Revised FIGO staging for carcinoma of the cervix uteri. Int J Gynaecol Obstet 145(1):129–135
Shimamoto K, Saito T, Kitade S, Tomita Y, Nagayama R, Yamaguchi S, Ariyoshi K, Okadome M (2018) A study of treatments and outcomes in elderly women with cervical cancer. Eur J Obstet Gynecol Reprod Biol 228:174–179
Osoba D (1994) Lessons learned from measuring health-related quality of life in oncology. J Clin Oncol 12(3):608–616
Rutherford C, M-B R., Tait M, Mileshkin L, King M (2017) Quality of life in cervical cancer. In: Farghaly S (editor) Uterine cervical cancer: clinical and therapeautic perspectives. Springer, New York. https://doi.org/10.1007/978-3-030-02701-8 [ISBN (Print): 978-3-030-02700-1; ISBN (EBook): 978-3-030-02700-1]
Food and Drug Administration (2009) Patient reported outcome measures: use in medical product development to support labelling claims. MD: US Department of Health & Human Support Food & Drug Administration
Moher D et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7)
Kmet LM, Lee RC, Cook LS (2004) Standard quality assessment criteria for evaluating primary research papers froma variety of fields. Alberta Heritage Foundation for Medical Research, Edmonton
Calvert MP et al (2013) Reporting of patient-reported outcomes in randomized trials: the CONSORT PRO extension. JAMA 309(8):814–822
Bogani G, Serati M, Nappi R, Cromi A, di Naro E, Ghezzi F (2014) Nerve-sparing approach reduces sexual dysfunction in patients undergoing laparoscopic radical hysterectomy. J Sex Med 11(12):3012–3020
Carter J, Sonoda Y, Baser RE, Raviv L, Chi DS, Barakat RR, Iasonos A, Brown CL, Abu-Rustum NR (2010) A 2-year prospective study assessing the emotional, sexual, and quality of life concerns of women undergoing radical trachelectomy versus radical hysterectomy for treatment of early-stage cervical cancer. Gynecol Oncol 119(2):358–365
Conic I et al (2012) Anxiety levels related to the type of therapy for cervical cancer. Central Eur J Med 7(4):490–496
Ding Y, Hu Y, Hallberg IR (2013) Health-related quality of life and associated factors in Chinese women with cervical cancer: a 9-month follow-up. Cancer Nurs 36(4):E18–E26
Du Toit GC, Kidd M (2015) Prospective quality of life study of south African women undergoing treatment for advanced-stage cervical cancer. Clin Ther 37(10):2324–2331
Ferrandina G, Mantegna G, Petrillo M, Fuoco G, Venditti L, Terzano S, Moruzzi C, Lorusso D, Marcellusi A, Scambia G (2012) Quality of life and emotional distress in early stage and locally advanced cervical cancer patients: a prospective, longitudinal study. Gynecol Oncol 124(3):389–394
Hawighorst-Knapstein S, Fusshoeller C, Franz C, Trautmann K, Schmidt M, Pilch H, Schoenefuss G, Georg Knapstein P, Koelbl H, Kelleher DK, Vaupel P (2004) The impact of treatment for genital cancer on quality of life and body image - results of a prospective longitudinal 10-year study. Gynecol Oncol 94(2):398–403
Heijkoop ST, Nout RA, Quint S, Mens JWM, Heijmen BJM, Hoogeman MS (2017) Dynamics of patient reported quality of life and symptoms in the acute phase of online adaptive external beam radiation therapy for locally advanced cervical cancer. Gynecol Oncol 147(2):439–449
Jiang H et al (2016) Vaginal extension improves sexual function in patients receiving laparoscopic radical hysterectomy. Gynecol Oncol 27
Liu B, Li L, Wang M, Wei L, Li J, Zou W, Lv Y, Zhang H, Liu S (2019) Health-related quality of life in locally advanced cervical cancer patients treated with neoadjuvant therapy followed by radical surgery: a single-institutional retrospective study from a prospective database. Gynecol Oncol 154(3):583–589
Mantegna G, Petrillo M, Fuoco G, Venditti L, Terzano S, Anchora LP, Scambia G, Ferrandina G (2013) Long-term prospective longitudinal evaluation of emotional distress and quality of life in cervical cancer patients who remained disease-free 2-years from diagnosis. BMC Cancer 13:127
Pieterse QD, Kenter GG, Maas CP, de Kroon CD, Creutzberg CL, Trimbos JBMZ, ter Kuile MM (2013) Self-reported sexual, bowel and bladder function in cervical cancer patients following different treatment modalities: longitudinal prospective cohort study. Int J Gynecol Cancer 23(9):1717–1725
He H et al (2017) Laparoscopic radical surgery in early-stage cervical cancer: short-term and long-term outcomes and survival analysis. Int J Clin Exp Med 10(8):12044–12055
Barnas E et al (2012) The quality of life of women treated for cervical cancer. Eur J Oncol Nurs 16(1):59–63
Fleming ND, Ramirez PT, Soliman PT, Schmeler KM, Chisholm GB, Nick AM, Westin SN, Frumovitz M (2016) Quality of life after radical trachelectomy for early-stage cervical cancer: a 5-year prospective evaluation. Gynecol Oncol 143(3):596–603
Fokdal L, Pötter R, Kirchheiner K, Lindegaard JC, Jensen NBK, Kirisits C, Chargari C, Mahantshetty U, Jürgenliemk-Schulz IM, Segedin B, Hoskin P, Tanderup K (2018) Physician assessed and patient reported urinary morbidity after radio-chemotherapy and image guided adaptive brachytherapy for locally advanced cervical cancer. Radiother Oncol 127(3):423–430
Jensen NBK, Pötter R, Kirchheiner K, Fokdal L, Lindegaard JC, Kirisits C, Mazeron R, Mahantshetty U, Jürgenliemk-Schulz IM, Segedin B, Hoskin P, Tanderup K, EMBRACE Collaborative Group (2018) Bowel morbidity following radiochemotherapy and image-guided adaptive brachytherapy for cervical cancer: physician- and patient reported outcome from the EMBRACE study. Radiother Oncol 127(3):431–439
Kirchheiner K, Czajka-Pepl A, Ponocny-Seliger E, Scharbert G, Wetzel L, Nout RA, Sturdza A, Dimopoulos JC, Dörr W, Pötter R (2014) Posttraumatic stress disorder after high-dose-rate brachytherapy for cervical cancer with 2 fractions in 1 application under spinal/epidural anesthesia: incidence and risk factors. Int J Radiat Oncol Biol Phys 89(2):260–267
Kirchheiner K, Nout RA, Czajka-Pepl A, Ponocny-Seliger E, Sturdza AE, Dimopoulos JC, Dörr W, Pötter R (2015) Health related quality of life and patient reported symptoms before and during definitive radio(chemo)therapy using image-guided adaptive brachytherapy for locally advanced cervical cancer and early recovery - a mono-institutional prospective study. Gynecol Oncol 136(3):415–423
Kirchheiner K, Pötter R, Tanderup K, Lindegaard JC, Haie-Meder C, Petrič P, Mahantshetty U, Jürgenliemk-Schulz IM, Rai B, Cooper R, Dörr W, Nout RA, Lindegaard J, Tanderup K, Fokdal L, van der Steen Banasik E, Haie-Meder C, Dumas I, Chargari C, Nout RA, van Limbergen E, Petrič P, Segedin B, Hudej R, Erickson B, Hoskin P, Lowe G, Mahantshetty U, Swamidas J, Shrivastava SK, Jürgenliemk-Schulz IM, de Leeuw A, Kirchheiner K, Dörr W, Pötter R, Lutgens LCHW, Hadjiev J, Cooper R, Bownes P, Sundset M, Bruheim K, Hellebust TP, Huang F, Menon G, Villafranca E, Rai B, Oinam AS, Tan LT, Bachand F, Jacobson G, Anttila M, Pieters B (2016) Health-related quality of life in locally advanced cervical cancer patients after definitive chemoradiation therapy including image guided adaptive brachytherapy: an analysis from the EMBRACE study. Int J Radiat Oncol Biol Phys 94(5):1088–1098
Ljuca D, Marosevic G (2011) Impact of chemoradiotherapy on vaginal and sexual function of patients with FIGO IIb cervical cancer. Bosnian J Basic Med Sci 11(1):62–64
Najjari Jamal D, Pötter R, Haie-Meder C, Lindegaard JC, Juergenliemk-Schulz IM, Mahantshetty U, Segedin B, Bruheim K, Hoskin P, Rai B, Wiebe E, Cooper R, Tanderup K, Kirchheiner K, EMBRACE collaborative group (2018) Physician assessed and patient reported lower limb edema after definitive radio(chemo)therapy and image-guided adaptive brachytherapy for locally advanced cervical cancer: a report from the EMBRACE study. Radiother Oncol 127(3):449–455
Smet S, Pötter R, Haie-Meder C, Lindegaard JC, Schulz-Juergenliemk I, Mahantshetty U, Segedin B, Bruheim K, Hoskin P, Rai B, Huang F, Cooper R, van Limbergen E, Tanderup K, Kirchheiner K, EMBRACE Collaborative Group (2018) Fatigue, insomnia and hot flashes after definitive radiochemotherapy and image-guided adaptive brachytherapy for locally advanced cervical cancer: an analysis from the EMBRACE study. Radiother Oncol 127(3):440–448
Cella D, Huang HQ, Monk BJ, Wenzel L, Benda J, McMeekin DS, Cohn D, Ramondetta L, Boardman CH (2010) Health-related quality of life outcomes associated with four cisplatin-based doublet chemotherapy regimens for stage IVB recurrent or persistent cervical cancer: a Gynecologic Oncology Group study. Gynecol Oncol 119(3):531–537
Long IHJ et al (2006) Clinical results and quality of life analysis for the MVAC combination (methotrexate, vinblastine, doxorubicin, and cisplatin) in carcinoma of the uterine cervix: a Gynecologic Oncology Group study. Gynecol Oncol 100(3):537–543
McQuellon RP, Thaler HT, Cella D, Moore DH (2006) Quality of life (QOL) outcomes from a randomized trial of cisplatin versus cisplatin plus paclitaxel in advanced cervical cancer: a Gynecologic Oncology Group study. Gynecol Oncol 101(2):296–304
Monk BJ, Huang HQ, Cella D, Long HJ 3rd, Gynecologic Oncology Group Study (2005) Quality of life outcomes from a randomized phase III trial of cisplatin with or without topotecan in advanced carcinoma of the cervix: a Gynecologic Oncology Group Study. J Clin Oncol Off J Am Soc Clin Oncol 23(21):4617–4625
Moore DH, Blessing JA, McQuellon RP, Thaler HT, Cella D, Benda J, Miller DS, Olt G, King S, Boggess JF, Rocereto TF (2004) Phase III study of cisplatin with or without paclitaxel in stage IVB, recurrent, or persistent squamous cell carcinoma of the cervix: a gynecologic oncology group study. J Clin Oncol 22(15):3113–3119
Penson RT, Huang HQ, Wenzel LB, Monk BJ, Stockman S, Long HJ III, Ramondetta LM, Landrum LM, Oaknin A, Reid TJA, Leitao MM, Method M, Michael H, Tewari KS (2015) Bevacizumab for advanced cervical cancer: patient-reported outcomes of a randomised, phase 3 trial (NRG Oncology-Gynecologic Oncology Group protocol 240). Lancet Oncol 16(3):301–311
Cocks K, King MT, Velikova G, de Castro G Jr, Martyn St-James M, Fayers PM, Brown JM (2012) Evidence-based guidelines for interpreting change scores for the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. Eur J Cancer 48(11):1713–1721
Kim JH, Park EC (2015) Impact of socioeconomic status and subjective social class on overall and health-related quality of life. BMC Public Health 15:783
van Gent MD et al (2016) Nerve-sparing radical hysterectomy versus conventional radical hysterectomy in early-stage cervical cancer. A systematic review and meta-analysis of survival and quality of life. Maturitas 94:30–38
Xue Z, Zhu X, Teng Y (2016) Comparison of nerve-sparing radical hysterectomy and radical hysterectomy: a systematic review and meta-analysis. Cell Physiol Biochem 38(5):1841–1850
Gubbala K, Laios A, Gallos I, Pathiraja P, Haldar K, Ind T (2014) Outcomes of ovarian transposition in gynaecological cancers; a systematic review and meta-analysis. J Ovarian Res 7(1):69
Vistad I, Fossa SD, Dahl AA (2006) A critical review of patient-rated quality of life studies of long-term survivors of cervical cancer. Gynecol Oncol 102(3):563–572
Pfaendler KS, Wenzel L, Mechanic MB, Penner KR (2015) Cervical cancer survivorship: long-term quality of life and social support. Clin Ther 37(1):39–48
Klugel S et al (2017) Concomitant psychiatric symptoms and impaired quality of life in women with cervical cancer: a critical review. Int J Women's Health 9:795–805
Ye S, Yang J, Cao D, Lang J, Shen K (2014) A systematic review of quality of life and sexual function of patients with cervical cancer after treatment. Int J Gynecol Cancer 24(7):1146–1157
Lammerink E et al (2012) Sexual functioning of cervical cancer survivors: a review with a female perspective. Int J Gynecol Cancer 22:E649
Author information
Authors and Affiliations
Contributions
Wiltink, L.M: led data extraction, analysis, and manuscript drafting and revision
King, M: conception and design, data interpretation, and manuscript revision and approval
Müller, F: data extraction, analysis, and manuscript revision and approval
Sousa, M.S.: data extraction, analysis, and manuscript revision and approval
Tang, M: data extraction, analysis, and manuscript revision and approval
Pendlebury, A: data extraction, analysis, and manuscript revision and approval
Pittman, J: data extraction, analysis, and manuscript revision and approval
Roberts, N: data extraction, analysis, and manuscript revision and approval
Mileshkin, L: conceptualization, methodology, data interpretation, and manuscript revision and approval
Mercieca-Bebber, R: data extraction, analysis, and manuscript revision and approval
Tait, M.-A: data extraction, analysis, and manuscript revision and approval
Campbell, R: data extraction, analysis, and manuscript revision and approval
Rutherford, C: conceptualization, methodology, data interpretation, writing original draft, writing—review, editing and approval, and supervision
Corresponding author
Ethics declarations
Conflict of interest
MT reports travel support from Roche, outside the submitted work. RMB reports UCB project funding, outside the submitted work. The other authors have no conflicts of interest to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Wiltink, L.M., King, M., Müller, F. et al. A systematic review of the impact of contemporary treatment modalities for cervical cancer on women’s self-reported health-related quality of life. Support Care Cancer 28, 4627–4644 (2020). https://doi.org/10.1007/s00520-020-05554-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05554-2