Abstract
Background
People with brain cancer and their support persons (SPs) are critical sources of information on the components of care that contribute to psychosocial outcomes.
Aims
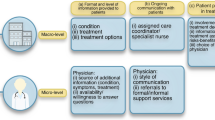
To determine the proportion of studies that examined (1) at least one of 14 nominated components of psychosocial cancer care and (2) more than one component of care.
Methods
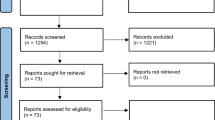
Medline, The Cochrane Library, PsycINFO and Embase were electronically searched for publications from January 1999 to December 2019. Publications that met the inclusion criteria were coded according to the number and type of psychosocial care components assessed from 14 listed components, and whether patient and/or SPs’ views about care were elicited.
Results
Of the 113 included publications, 61 publications included patient-reported data only (54%), 27 included both patient and SP-reported data (24%) and 25 included SP-reported data only (22%). Most assessed a single component of care (77% of patient-reported and 71% of SP-reported). No publications assessed all 14 components. The “Psychosocial” component was the most frequently assessed component of care for patient-reported (n = 80/88, 91%) and SP-reported publications (n = 46/52, 88%).
Conclusions
Publications reporting on psychosocial care in brain cancer present a relatively narrow view of patient and support person experiences. The inclusion of both patient and support person perspectives and the assessment of multiple components of care are required in future research to optimize psychosocial outcomes in brain cancer.



Similar content being viewed by others
Data availability
Datasets are available from the corresponding author on reasonable request.
References
Sterckx W, Coolbrandt A, Dierckx de Casterle B, Van den Heede K, Decruyenaere M, Borgenon S et al (2013) The impact of a high-grade glioma on everyday life: a systematic review from the patient’s and caregiver’s perspective. Eur J Oncol Nurs 17(1):107–117
Taphoorn MJ, Klein M (2004) Cognitive deficits in adult patients with brain tumours. Lancet Neurol 3(3):159–168
The Brain Tumour Charity (2015) Losing myself: the reality of life with a brain tumour. United Kingdom, The Brain Tumour Charity
Halkett GK, Lobb EA, Oldham L, Nowak AK (2010) The information and support needs of patients diagnosed with high grade glioma. Patient Educ Couns 79(1):112–119
Langbecker D, Yates P (2016) Primary brain tumor patients’ supportive care needs and multidisciplinary rehabilitation, community and psychosocial support services: awareness, referral and utilization. J Neuro-Oncol 127(1):91–102
Morra ME, Thomsen C, Vezina A, Akkerman D, Bright MA, Dickens C et al (2007) The International Cancer Information Service: a worldwide resource. J Cancer Educ 22(1 Suppl):S61–S69
Chambers SK, Grassi L, Hyde MK, Holland J, Dunn J (2015) Integrating psychosocial care into neuro-oncology: challenges and strategies. Front Oncol 5:41
Huang J, Zeng C, Xiao J, Zhao D, Tang H, Wu H, Chen J (2017) Association between depression and brain tumor: a systematic review and meta-analysis. Oncotarget. 8(55):94932–94943
Halkett GKB, Lobb EA, Shaw T, Sinclair MM, Miller L, Hovey E, Nowak AK (2018) Do carer’s levels of unmet needs change over time when caring for patients diagnosed with high-grade glioma and how are these needs correlated with distress? Support Care Cancer 26(1):275–286
Sherwood PR, Cwiklik M, Donovan HS (2016)Neuro-oncology family caregiving: review and directions for future research. CNS Oncol 5(1):41–48
Li Q, Loke AY (2014) A literature review on the mutual impact of the spousal caregiver–cancer patients dyads: ‘communication’, ‘reciprocal influence’, and ‘caregiver–patient congruence’. Eur J Oncol Nurs 18(1):58–65
Catt S, Chalmers A, Fallowfield L (2008) Psychosocial and supportive-care needs in high-grade glioma. Lancet Oncol 9(9):884–891
Epstein RM, Street RL (2011) The values and value of patient-centered care. Ann Fam Med 9(2):100–103. https://doi.org/10.1370/afm.1239
Institute of Medicine (2001) Crossing the quality chasm: a new health system for the 21st century. National Academies Press, Washington D.C. https://www.nap.edu/openbook.php?record_id=10027&page=39. Accessed December 2019
Rathert C, Wyrwich MD, Boren SA (2013)Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev 70(4):351–379
Sanson-Fisher R, Fakes K, Waller A, Mackenzie L, Bryant J, Herrmann A (2019) Assessing patients’ experiences of cancer care across the treatment pathway: a mapping review of recent psychosocial cancer care publications. Support Care Cancer 27(6):1997–2006
King A, Hoppe RB (2013) "Best practice" for patient-centered communication: a narrative review. J Grad Med Educ 5(3):385–393
De Vries AM et al (2014) Clinician characteristics, communication, and patient outcome in oncology: a systematic review. Psychooncology 23(4):375–381
van der Velden NCA et al (2020) The effect of prognostic communication on patient outcomes in palliative cancer care: a systematic review. Curr Treat Options Oncol 21(5):40
Fletcher C et al (2017) The information needs of adult cancer survivors across the cancer continuum: A scoping review. Patient Educ Couns 100(3):383–410
Shin DW, Cho J, Roter DL, Kim SY, Sohn SK, Yoon MS, Kim YW, Cho BL, Park JH (2013) Preferences for and experiences of family involvement in cancer treatment decision-making: patient–caregiver dyads study. Psycho-Oncology. 22(11):2624–2631
Laidsaar-Powell RC et al (2013) Physician-patient-companion communication and decision-making: a systematic review of triadic medical consultations. Patient Educ Couns 91(1):3–13
Lamore K, Montalescot L, Untas A (2017) Treatment decision-making in chronic diseases: What are the family members' roles, needs and attitudes? A systematic review. Patient Educ Couns 100(12):2172–2181
Shay LA, Lafata JE (2015) Where is the evidence? A systematic review of shared decision making and patient outcomes. Medical decision making : An International Journal of the Society for Medical Decision Making 35(1):114–131
Woodhouse KD et al (2017) A review of shared decision-making and patient decision aids in radiation oncology. Journal of cancer education : the official Journal of the American Association for Cancer Education 32(2):238–245
Kane HL et al (2014) Implementing and evaluating shared decision making in oncology practice. CA Cancer J Clin 64(6):377–388
Waller A et al (2015) Preparatory education for cancer patients undergoing surgery: A systematic review of volume and quality of research output over time. Patient Educ Couns
Halkett G et al (2016) Communication skills training for radiation therapists: preparing patients for radiation therapy. J Med Radiat Sci 63(4):232–241
Heshmati Nabavi F et al (2016) Effect of pre-treatment education programs on the anxiety of patients receiving radiotherapy: an integrative literature review. J Evidence Based Care 6(1):49–62
Hu J et al (2019) Peer support interventions for breast cancer patients: a systematic review. Breast Cancer Res Treat 174(2):325–341
Hoey LM et al (2008) Systematic review of peer-support programs for people with cancer. Patient Educ Couns 70(3):315–337
Kowitt SD et al (2019) Peer support opportunities across the cancer care continuum: a systematic scoping review of recent peer-reviewed literature. Supportive Care in Cancer : Official Journal of the Multinational Association of Supportive Care in Cancer 27(1):97–108
Azzani M, Roslani AC, Su TT (2015) The perceived cancer-related financial hardship among patients and their families: a systematic review. Support Care Cancer 23(3):889–898
Altice CK et al (2017) Financial hardships experienced by cancer survivors: a systematic review. J Natl Cancer Inst 109(2)
Slavova-Azmanova NS, Newton JC, Saunders CM (2020) Marked variation in out-of-pocket costs for cancer care in Western Australia. Med J Aust 212(11):525–526
Loiselle CG et al (2020) The nurse pivot-navigator associated with more positive cancer care experiences and higher patient satisfaction. Can Oncol Nurs J 30(1):48–53
Bernardo BM et al (2019) The efficacy and cost-effectiveness of patient navigation programs across the cancer continuum: A systematic review. Cancer 125(16):2747–2761
Robinson-White S et al (2010) Patient navigation in breast cancer: a systematic review. Cancer Nurs 33(2):127–140
Carlson LE, Waller A, Mitchell AJ (2012) Screening for distress and unmet needs in patients with cancer: review and recommendations. J Clin Oncol 30(11):1160–1177
Basch E et al (2012) Recommendations for incorporating patient-reported outcomes into clinical comparative effectiveness research in adult oncology. J Clin Oncol 30(34):4249–4255
Howell D et al (2015) Patient-reported outcomes in routine cancer clinical practice: a scoping review of use, impact on health outcomes, and implementation factors. Annals of Oncology 26(9):1846–1858
Australia C (2014) Clinical guidance for responding to suffering in adults with cancer. Cancer Australia: Sydney.
Aubin M et al (2012) Interventions to improve continuity of care in the follow-up of patients with cancer. Cochrane Database Syst Rev (7):Cd007672
Lawn S, Fallon-Ferguson J, Koczwara B (2017) Shared care involving cancer specialists and primary care providers – What do cancer survivors want? Health Expect 20(5):1081–1087
Smith SM et al (2017) Shared care across the interface between primary and specialty care in management of long term conditions. Cochrane Database Syst Rev 2(2):Cd004910
Wilcoxon H et al (2011) Multidisciplinary cancer care in Australia: a national audit highlights gaps in care and medico-legal risk for clinicians. Asia Pac J Clin Oncol 7(1):34–40
Pereira Gray DJ et al (2018) Continuity of care with doctors—a matter of life and death? A systematic review of continuity of care and mortality. Patient-centred Medicine Research 8(6):e021161
Ly L, et al (2020) Defining and measuring quality cancer survivorship care: An environmental scan. Am Soc Clin Oncol 38(29_suppl):219
Jefford M (2020) Improving the care of adult cancer survivors. Asia Pac J Oncol Nurs 7(1):2–5
Alfano CM et al (2019) Equitably improving outcomes for cancer survivors and supporting caregivers: A blueprint for care delivery, research, education, and policy. CA Cancer J Clin 69(1):35–49
Clayton JM et al (2007) Clinical practice guidelines for communicating prognosis and end-of-life issues with adults in the advanced stages of a life-limiting illness, and their caregivers. Med J Aust 186(S12):S77–S105
Haun MW et al (2017) Early palliative care for adults with advanced cancer. Cochrane Database of Syst Rev 12(6):CD011129
Johnson S et al (2016) Advance care planning for cancer patients: a systematic review of perceptions and experiences of patients, families, and healthcare providers. Psychooncology 25(4):362–386
Jimenez G et al (2018) Overview of systematic reviews of advance care planning: summary of evidence and global lessons. J Pain Symptom Manag 56(3):436–459.e25
Carey M et al (2019) The patient perspective on errors in cancer care: results of a cross-sectional survey. J Patient Saf 15(4):322–327
Bryant J et al (2017) The patients' perspective: hematological cancer patients' experiences of adverse events as part of care. J Patient Saf
Snyder CF, Aaronson NK, Choucair AK, Elliott TE, Greenhalgh J, Halyard MY, Hess R, Miller DM, Reeve BB, Santana M (2012) Implementing patient-reported outcomes assessment in clinical practice: a review of the options and considerations. Qual Life Res 21(8):1305–1314
Tremblay D, Roberge D, Berbiche D (2015) Determinants of patient-reported experience of cancer services responsiveness. BMC Health Serv Res 15(1):425
Davies E, Hopkins A. Good practice in the management of adults with malignant cerebral glioma: clinical guidelines. Working Group, Royal College of Physicians. Br J Neurosurg 1997;11(4):318–330
Butow P, Price MA, Shaw JM, Turner J, Clayton JM, Grimison P, Rankin N, Kirsten L (2015) Clinical pathway for the screening, assessment and management of anxiety and depression in adult cancer patients: Australian guidelines. Psycho-Oncology. 24(9):987–1001
Holland JC, Andersen B, Breitbart WS, Buchmann LO, Compas B, Deshields TL, Dudley MM, Fleishman S, Fulcher CD, Greenberg DB, Greiner CB, Handzo GF, Hoofring L, Hoover C, Jacobsen PB, Kvale E, Levy MH, Loscalzo MJ, McAllister-Black R, Mechanic KY, Palesh O, Pazar JP, Riba MB, Roper K, Valentine AD, Wagner LI, Zevon MA, McMillian NR, Freedman-Cass DA (2013) Distress management. J Natl Compr Cancer Netw 11(2):190–209
Feldstain A, Tomei C, Bélanger M, Lebel S (2014) Screening for distress in patients with cancer: methodologic considerations. Curr Oncol 21(2):e330
Vodermaier A, Millman RD (2011) Accuracy of the Hospital Anxiety and Depression Scale as a screening tool in cancer patients: a systematic review and meta-analysis. Support Care Cancer 19(12):1899–1908
Donovan KA, Grassi L, McGinty HL, Jacobsen PB (2014) Validation of the distress thermometer worldwide: state of the science. Psycho-oncology. 23(3):241–250
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, Haes JCJM, Kaasa S, Klee M, Osoba D, Razavi D, Rofe PB, Schraub S, Sneeuw K, Sullivan M, Takeda F (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
Weitzner MA, Meyers CA, Gelke CK, Byrne KS, Cella DF, Levin VA (1995) The Functional Assessment of Cancer Therapy (FACT) scale. Development of a brain subscale and revalidation of the general version (FACT-G) in patients with primary brain tumors. Cancer. 75(5):1151–1161
Dirven L, Koekkoek JAF, Reijneveld JC, Taphoorn MJB (2016)Health-related quality of life in brain tumor patients: as an endpoint in clinical trials and its value in clinical care. Expert Rev Qual Life Cancer Care 1(1):37–44
Tzelepis F, Sanson-Fisher RW, Zucca AC, Fradgley EA (2015) Measuring the quality of patient-centered care: why patient-reported measures are critical to reliable assessment. Patient Prefer Adherence 9:831–835
Janda M, Eakin EG, Bailey L, Walker D, Troy K (2006) Supportive care needs of people with brain tumours and their carers. Support Care Cancer 14(11):1094–1103
Randazzo D, Peters KB (2016) Psychosocial distress and its effects on the health-related quality of life of primary brain tumor patients. CNS Oncol 5(4):241–249
Kroenke CH, Kubzansky LD, Schernhammer ES, Holmes MD, Kawachi I (2006) Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol 24(7):1105–1111
Lutgendorf SK, De Geest K, Bender D, Ahmed A, Goodheart MJ, Dahmoush L et al (2012) Social influences on clinical outcomes of patients with ovarian cancer. J Clin Oncol 30(23):2885–2890
Cubis L, Ownsworth T, Pinkham MB, Chambers S (2018) The social trajectory of brain tumor: a qualitative metasynthesis. Disabil Rehabil 40(16):1857–1869
Pollak KI, Arnold RM, Jeffreys AS, Alexander SC, Olsen MK, Abernethy AP, Sugg Skinner C, Rodriguez KL, Tulsky JA (2007) Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol 25(36):5748–5752
De Vries A, de Roten Y, Meystre C, Passchier J, Despland JN, Stiefel F (2014) Clinician characteristics, communication, and patient outcome in oncology: a systematic review. Psycho-Oncology. 23(4):375–381
Freund KM, Battaglia TA, Calhoun E, Darnell JS, Dudley DJ, Fiscella K et al (2014) Impact of patient navigation on timely cancer care: the Patient Navigation Research Program. J Natl Cancer Inst 106(6):dju115
Robinson-White S, Conroy B, Slavish KH, Rosenzweig M (2010) Patient navigation in breast cancer: a systematic review. Cancer Nurs 33(2):127–140
Australian Institute of Health and Welfare (2017) Brain and other central nervous system cancers. Cat. no. CAN 106. AIHW, Canberra
Zwakman M, Jabbarian L, van Delden J, van der Heide A, Korfage I, Pollock K et al (2018) Advance care planning: a systematic review about experiences of patients with a life-threatening or life-limiting illness. 32(8):1305–1321
Waller A, Turon H, Bryant J, Zucca A, Evans T-J, Sanson-Fisher R (2019) Medical oncology outpatients’ preferences and experiences with advanced care planning: a cross-sectional study. BMC Cancer 19(1):63
Rodi H, Detering K, Sellars M, Macleod A, Todd J, Fullerton S, Waller A, Nolte L (2020) Exploring advance care planning awareness, experiences, and preferences of people with cancer and support people: an Australian online cross-sectional study. Support Care Cancer
Detering KM, Buck K, Ruseckaite R, Kelly H, Sellars M, Sinclair C, Clayton JM, Nolte L (2019) Prevalence and correlates of advance care directives among older Australians accessing health and residential aged care services: multicentre audit study. BMJ Open 9(1):e025255
Buck K, Detering KM, Pollard A, Sellars M, Ruseckaite R, Kelly H, White BP, Sinclair C, Nolte L (2019) Concordance between self-reported completion of advance care planning documentation and availability of documentation in Australian health and residential aged care services. J Pain Symptom Manag 58(2):264–274
Ngo-Metzger Q, August KJ, Srinivasan M, Liao S, Meyskens Jr FL. End-of-life care: guidelines for patient-centered communication. 2008
Higginson IJ, Evans CJ (2010) What is the evidence that palliative care teams improve outcomes for cancer patients and their families? Cancer J 16(5):423–435
Song K, Amatya B, Voutier C, Khan F (2016) Advance care planning in patients with primary malignant brain tumors: a systematic review. Front Oncol 6:223
Earle CC, Landrum MB, Souza JM, Neville BA, Weeks JC, Ayanian JZ (2008) Aggressiveness of cancer care near the end of life: is it a quality-of-care issue? J Clin Oncol 26(23):3860–3866
Ho TH, Barbera L, Saskin R, Lu H, Neville BA, Earle CC (2011) Trends in the aggressiveness of end-of-life cancer care in the universal health care system of Ontario, Canada. J Clin Oncol 29(12):1587–1591
Zhang B, Wright AA, Huskamp HA, Nilsson ME, Maciejewski ML, Earle CC, Block SD, Maciejewski PK, Prigerson HG (2009) Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med 169(5):480–488
Giammalva GR, Iacopino DG, Azzarello G, Gaggiotti C, Graziano F, Gulì C et al (2018)End-of-life care in high-grade glioma patients. The palliative and supportive perspective. Brain Sci 8(7):125
Pace A, Dirven L, Koekkoek JAF, Golla H, Fleming J, Ruda R et al (2017) European Association for Neuro-Oncology(EANO) guidelines for palliative care in adults with glioma. Lancet Oncol 18(6):e330–ee40
Barry MJ, Edgman-Levitan S (2012) Shared decision making—the pinnacle of patient-centered care. N Engl J Med 366(9):780–781
Davison BJ, Gleave ME, Goldenberg SL, Degner LF, Hoffart D, Berkowitz J (2002) Assessing information and decision preferences of men with prostate cancer and their partners. Cancer Nurs 25(1):42–49
Pardon K, Deschepper R, Stichele RV, Bernheim JL, Mortier F, Bossuyt N, Schallier D, Germonpré P, Galdermans D, van Kerckhoven W, Deliens L, EOLIC-Consortium(2010) Preferences of patients with advanced lung cancer regarding the involvement of family and others in medical decision-making. J Palliat Med 13(10):1199–1203
Gilbar R, Gilbar O (2009) The medical decision-making process and the family: the case of breast cancer patients and their husbands. Bioethics. 23(3):183–192
Institute of Medicine (2008) Cancer care for the whole patient: meeting psychosocial health needs. National Academies Press, Washington D.C. Available from: http://www.nap.edu/openbook.php?record_id=10027&page=39
Badr H, Herbert K, Bonnen MD, Asper JA, Wagner T (2018) Dyadic coping in patients undergoing radiotherapy for head and neck cancer and their spouses. Front Psychol 9
Heckel M, Hoser B, Stiel S (2018) Caring for patients with brain tumors compared to patients with non-brain tumors: experiences and needs of informal caregivers in home care settings. J Psychosoc Oncol 36(2):189–202
Aoun SM, Deas K, Howting D, Lee G (2015) Exploring the support needs of family caregivers of patients with brain cancer using the CSNAT: a comparative study with other cancer groups. PLoS One 10(12):e0145106
Morgan MA, Small BJ, Donovan KA, Overcash J, McMillan S (2011) Cancer patients with pain: the spouse/partner relationship and quality of life. Cancer Nurs 34(1):13–23
Badr H, Carmack CL, Kashy DA, Cristofanilli M, Revenson TA (2010) Dyadic coping in metastatic breast cancer. Health Psychol 29(2):169–180
Chen M-L, Chu L, Chen H-C(2004) Impact of cancer patients’ quality of life on that of spouse caregivers. Support Care Cancer 12(7):469–475
Acknowledgements
The authors would like to acknowledge the assistance of Sarah Tew in preparing the manuscript and Angela Smith for assisting with the search strategy and execution.
Code availability
NA.
Funding
This research was supported by a Strategic Research Partnership Grant (CSR 11–02; RSF) from The Cancer Council NSW. LB is supported by a University of Newcastle PhD Scholarship. These funding sources had no role in the design of this study and did not have any role during its execution, analyses, interpretation of the data or decision to submit results. This research was also supported by infrastructure funding from University of Newcastle and Hunter Medical Research Institute.
Author information
Authors and Affiliations
Contributions
All authors conceived the study design and methodology. Authors 1 and 2 contributed to data acquisition and analysis. All authors contributed to the interpretation of study findings, have read and approved the final version.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
This article does not contain any studies with human participants.
Consent for publication
This article does not contain any studies with human participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOC 57 kb)
Rights and permissions
About this article
Cite this article
Boyd, L.A.P., Waller, A.E., Hill, D. et al. Brain cancer patient and support persons’ experiences of psychosocial care: a mapping of research outputs. Support Care Cancer 29, 5559–5569 (2021). https://doi.org/10.1007/s00520-021-06071-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06071-6