Abstract
Aims
Offspring of mothers suffering from obesity and/or gestational diabetes mellitus (GDM) were reported to be at risk of higher birth weight (BW), later obesity and diabetes. We hypothesize that infant anthropometry changes related to maternal pathological status are due to dysregulated infant metabolism.
Methods
First, we inspected differences in BMI z-scores (z-BMI) between three infant groups: born to normal weight (NW; n = 49), overweight/obese (OV/OB; n = 40) and GDM mothers (n = 27) at birth and 1 year. Then, we inspected associations between cord blood metabolites and 1-year Δ z-BMI in the three infant groups at birth and 1 year.
Results
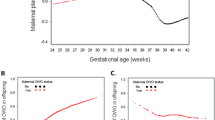
No statistically significant difference was detected in z-BMI between the study groups at birth; however, GDM was associated with heavier infants at 1 year. Regarding the associations between the metabolites and z-BMI, phospholipids, especially those containing polyunsaturated fatty acids, were the species most impacted by the maternal metabolic status, since numerous phosphatidylcholines–PUFA were positively associated with z-BMI in NW but negatively in OV/OB and GDM groups at birth. Conversely, the sum of lysophosphatidylcholines was only positively associated with z-BMI in NW at birth but of no relation in the other two groups. At 1 year, most of the associations seen at birth were reversed in NW and lost in OV/OB and GDM groups. In the NW group, PC-PUFA were found to be negatively associated with Δ z-BMI at 1 year in addition to some medium-chain acylcarnitines, tricarboxylic acid metabolites, Asp and Asn-to-Asp ratio. In OV/OB and GDM groups, the non-esterified fatty acid (NEFA26:0) and His correlated with Δ z-BMI at 1 year in negative and positive directions, respectively.
Conclusions
GDM was associated with overweight in offspring at 1 year, independent of the BW with lack of evidence on existing correlation of this finding with metabolic alterations detected in cord blood metabolome. Associations were found between cord blood metabolites and infant anthropometry at birth and were influenced by maternal OB and GDM. However, an extension of the findings monitored at birth among the three groups was not detected longitudinally showing a lack of predictive power of cord blood metabolome for later development at least 1 year.

Similar content being viewed by others
References
OECD (2016) Overweight and obesity among adults. In: Health at a glance: Europe 2016: state of health in the EU cycle. OECD Publishing, Paris
Ahrens W, Pigeot I, Pohlabeln H et al (2014) Prevalence of overweight and obesity in European children below the age of 10. Int J Obes (Lond) 38(Suppl 2):S99–S107. https://doi.org/10.1038/ijo.2014.140
Schaefer-Graf UM, Pawliczak J, Passow D et al (2005) Birth weight and parental BMI predict overweight in children from mothers with gestational diabetes. Diabetes Care 28(7):1745–1750
Catalano PM, McIntyre HD, Cruickshank JK et al (2012) The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care 35(4):780–786. https://doi.org/10.2337/dc11-1790
Yessoufou A, Moutairou K (2011) Maternal diabetes in pregnancy: early and long-term outcomes on the offspring and the concept of “metabolic memory”. Exp Diabetes Res 2011:218598. https://doi.org/10.1155/2011/218598
Buchanan TA, Xiang AH (2005) Gestational diabetes mellitus. J Clin Investig 115(3):485–491. https://doi.org/10.1172/JCI24531
Blackwell SC, Landon MB, Mele L et al (2016) Relationship between excessive gestational weight gain and neonatal adiposity in women with mild gestational diabetes mellitus. Obstet Gynecol 128(6):1325–1332. https://doi.org/10.1097/aog.0000000000001773
Catalano PM, Hauguel-De Mouzon S (2011) Is it time to revisit the Pedersen hypothesis in the face of the obesity epidemic? Am J Obstet Gynecol 204(6):479–487. https://doi.org/10.1016/j.ajog.2010.11.039
Pintaudi B, Fresa R, Dalfra M et al (2018) The risk stratification of adverse neonatal outcomes in women with gestational diabetes (STRONG) study. Acta Diabetol 55(12):1261–1273. https://doi.org/10.1007/s00592-018-1208-x
Shokry E, Marchioro L, Uhl O et al (2019) Impact of maternal BMI and gestational diabetes mellitus on maternal and cord blood metabolome: results from the PREOBE cohort study. Acta Diabetol 56(4):421–430. https://doi.org/10.1007/s00592-019-01291-z
Berglund SK, García-Valdés L, Torres-Espinola FJ et al (2016) Maternal, fetal and perinatal alterations associated with obesity, overweight and gestational diabetes: an observational cohort study (PREOBE). BMC Public Health 16(1):207. https://doi.org/10.1186/s12889-016-2809-3
Hellmuth C, Uhl O, Standl M et al (2017) Cord blood metabolome is highly associated with birth weight, but less predictive for later weight development. Obes Facts 10(2):85–100. https://doi.org/10.1159/000453001
Sampath H, Ntambi JM (2008) Role of stearoyl-CoA desaturase in human metabolic disease. Future Lipidol 3(2):163–173
Haggarty P (2002) Placental regulation of fatty acid delivery and its effect on fetal growth—a review. Placenta 23:S28–S38. https://doi.org/10.1053/plac.2002.0791
Prieto-Sánchez MT, Ruiz-Palacios M, Blanco-Carnero JE et al (2017) Placental MFSD2a transporter is related to decreased DHA in cord blood of women with treated gestational diabetes. Clin Nutr 36(2):513–521. https://doi.org/10.1016/j.clnu.2016.01.014
Zeijdner EE, Houwelingen ACV, Kester ADM, Hornstra G (1997) Essential fatty acid status in plasma phospholipids of mother and neonate after multiple pregnancy. Prostaglandins Leukot Essent Fatty Acids 56(5):395–401. https://doi.org/10.1016/S0952-3278(97)90590-1
Karlsson M, Mårild S, Brandberg J, Lönn L, Friberg P, Strandvik B (2006) Serum phospholipid fatty acids, adipose tissue, and metabolic markers in obese adolescents. Obesity (Silver Spring) 14(11):1931–1939. https://doi.org/10.1038/oby.2006.225
Uhl O, Demmelmair H, Segura MT et al (2015) Effects of obesity and gestational diabetes mellitus on placental phospholipids. Diabetes Res Clin Pract 109(2):364–371. https://doi.org/10.1016/j.diabres.2015.05.032
Visiedo F, Bugatto F, Sánchez V, Cózar-Castellano I, Bartha JL, Perdomo G (2013) High glucose levels reduce fatty acid oxidation and increase triglyceride accumulation in human placenta. Am J Physiol Endocrinol Metab 305(2):E205–E212. https://doi.org/10.1152/ajpendo.00032.2013
Wells J (2011) An evolutionary perspective on the trans-generational basis of obesity. Ann Hum Biol 38:400–409. https://doi.org/10.3109/03014460.2011.580781
Wells J (2012) A critical appraisal of the predictive adaptive response hypothesis. Int J Epidemiol 41:229–235. https://doi.org/10.1093/ije/dyr239
Dubé E, Gravel A, Martin C et al (2012) Modulation of fatty acid transport and metabolism by maternal obesity in the human full-term placenta. Biol Reprod 87(1):14. https://doi.org/10.1095/biolreprod.111.098095
Barber MN, Risis S, Yang C et al (2012) Plasma lysophosphatidylcholine levels are reduced in obesity and type 2 diabetes. PLoS ONE 7(7):e41456. https://doi.org/10.1371/journal.pone.0041456
Del Bas JM, Caimari A, Rodriguez-Naranjo MI et al (2016) Impairment of lysophospholipid metabolism in obesity: altered plasma profile and desensitization to the modulatory properties of n-3 polyunsaturated fatty acids in a randomized controlled trial. Am J Clin Nutr 104(2):266–279. https://doi.org/10.3945/ajcn.116.130872
Heimerl S, Fischer M, Baessler A et al (2014) Alterations of plasma lysophosphatidylcholine species in obesity and weight loss. PLoS ONE 9(10):e111348. https://doi.org/10.1371/journal.pone.0111348
Lehmann R, Franken H, Dammeier S et al (2013) Circulating lysophosphatidylcholines are markers of a metabolically benign nonalcoholic fatty liver. Diabetes Care 36(8):2331–2338. https://doi.org/10.2337/dc12-1760
Wallace M, Morris C, O’Grada CM et al (2014) Relationship between the lipidome, inflammatory markers and insulin resistance. Mol BioSyst 10(6):1586–1595. https://doi.org/10.1039/c3mb70529c
Fabbrini E, Sullivan S, Klein S (2010) Obesity and nonalcoholic fatty liver disease: biochemical, metabolic, and clinical implications. Hepatology (Baltimore, MD) 51(2):679–689. https://doi.org/10.1002/hep.23280
Lehmann R, Zhao X, Weigert C et al (2010) Medium chain acylcarnitines dominate the metabolite pattern in humans under moderate intensity exercise and support lipid oxidation. PLoS ONE 5(7):e11519. https://doi.org/10.1371/journal.pone.0011519
Gazquez A, Ruiz-Palacios M, Larque E (2017) DHA supplementation during pregnancy as phospholipids or TAG produces different placental uptake but similar fetal brain accretion in neonatal piglets. Br J Nutr 118(11):981–988. https://doi.org/10.1017/s0007114517002951
Marseglia L, Manti S, D’Angelo G et al (2014) Oxidative stress in obesity: a critical component in human diseases. Int J Mol Sci 16(1):378–400. https://doi.org/10.3390/ijms16010378
Dudzik D, Zorawski M, Skotnicki M et al (2014) Metabolic fingerprint of gestational diabetes mellitus. J Proteomics 103:57–71. https://doi.org/10.1016/j.jprot.2014.03.025
Gillman MW, Rifas-Shiman S, Berkey CS, Field AE, Colditz GA (2003) Maternal gestational diabetes, birth weight, and adolescent obesity. Pediatrics 111(3):e221–e226
Hillier TA, Pedula KL, Schmidt MM, Mullen JA, Charles MA, Pettitt DJ (2007) Childhood obesity and metabolic imprinting: the ongoing effects of maternal hyperglycemia. Diabetes Care 30(9):2287–2292. https://doi.org/10.2337/dc06-2361
Baptiste-Roberts K, Nicholson WK, Wang N-Y, Brancati FL (2012) Gestational diabetes and subsequent growth patterns of offspring: the National Collaborative Perinatal Project. Matern Child Health J 16(1):125–132. https://doi.org/10.1007/s10995-011-0756-2
Cole TJ, Singhal A, Fewtrell MS, Wells JC (2016) Weight centile crossing in infancy: correlations between successive months show evidence of growth feedback and an infant-child growth transition. Am J Clin Nutr 104(4):1101–1109. https://doi.org/10.3945/ajcn.116.139774
Beauchamp G, Mennella J (2009) Early flavor learning and its impact on later feeding behavior. J Pediatr Gastroenterol Nutr 48(1):S25–S30. https://doi.org/10.1097/mpg.0b013e31819774a5
Mennella JA (2014) Ontogeny of taste preferences: basic biology and implications for health. Am J Clin Nutr 99(3):704s–711s. https://doi.org/10.3945/ajcn.113.067694
Acknowledgements
The authors thank the study participants, the obstetricians, paediatricians and technicians of the EURISTIKOS team and the PREOBE team at the University of Granada. We are grateful to Stephanie Winterstetter, Alexander Haag and Tina Honsowitz for their support in the analysis.
Funding
This work was supported by Andalusian Ministry of Economy, Science and Innovation, PREOBE Excellence Project (Ref. P06-CTS-02341), Spanish Ministry of Economy and Competitiveness (Ref. BFU2012-40254-C03-01 and Ref. SAF2015-69265-C2-2-R), the European Research Council Advanced Grant META-GROWTH (ERC-2012-AdG 322605), European Commission research projects EarlyNutrition, FP7–FP7 KBBE-2011-1 (289346 y) and Horizon2020 DynaHEALTH (633595).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors reports conflicts of interest.
Ethical approval
The study was approved by the Bioethical Committees for Clinical Research of the Clinical University Hospital San Cecilio, the Mother-Infant University Hospital of Granada, Spain.
Informed consent
Participation was voluntary, and written informed consent was obtained from participants at study entry.
Additional information
Managed by Antonio Secchi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shokry, E., Marchioro, L., Uhl, O. et al. Transgenerational cycle of obesity and diabetes: investigating possible metabolic precursors in cord blood from the PREOBE study. Acta Diabetol 56, 1073–1082 (2019). https://doi.org/10.1007/s00592-019-01349-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-019-01349-y