Abstract
Background
Intracranial arachnoid cysts are extra-axial benign lesions mainly found in the middle cerebral fossa. Rare case series report various cranial nerve dysfunctions associated with cerebellopontine angle (CPA) cysts and there is no consensus with regard to their surgical management; some reports claiming that subjective improvement in adults with intracranial arachnoid cysts cannot justify surgical treatment.
Methods
This retrospective study included all 12 consecutive adult patients treated by microsurgical fenestration for symptomatic CPA arachnoid cysts between 2010 and 2019 and using a retrosigmoid approach. Demographic, clinical, surgical, and radiological data were collected from medical files.
Results
The main symptoms were audiovestibular in 9 patients (75%) complaining of dizziness and 6 patients (50%) with hearing loss. In addition, 3 patients (25%) reported tinnitus, 3 patients (25%) presented vasovagal syncope, and 1 patient (8.3%) reported facial pain. Surgery improved 5 patients (83%) with pre-operative hearing loss, 7 patients (78%) reporting dizziness, and all patients with vasovagal syncope. All of the patients recovered from at least one symptom. No recurrence was observed with a mean follow-up of 5.5 years.
Conclusion
Although most arachnoid cysts are asymptomatic, the CPA location may lead to cranial nerve impairments. Microsurgical fenestration seems to be a simple, safe, and effective technique.

Similar content being viewed by others
References
Alaani A, Hogg R, Siddiq MA, Chavda SV, Irving RM (2005) Cerebellopontine angle arachnoid cysts in adult patients: what is the appropriate management? J Laryngol Otol 119(5):337–341
Al-Holou WN, Terman S, Kilburg C, Garton HJL, Muraszko KM, Maher CO (2013) Prevalence and natural history of arachnoid cysts in adults. J Neurosurg 118(2):222–231
Amelot A, Beccaria K, Blauwblomme T, Bourgeois M, Paternoster G, Cuny M-L, Zerah M, Sainte-Rose C, Puget S (2019) Microsurgical, endoscopic, and shunt management of pediatric temporosylvian arachnoid cysts: a comparative study. J Neurosurg Pediatr 23(6):749–757
Arai H, Sato K, Wachi A, Okuda O, Nobuaki T (1996) Arachnoid cysts of the middle cranial fossa: experience with 77 patients who were treated with cystoperitoneal shunting | Neurosurgery | Oxford Academic. Neurosurgery 39(6):1108–1113
Baguley DM, Moffat DA, Hardy DG (1992) What is the effect of translabyrinthine acoustic schwannoma removal upon tinnitus? J Laryngol Otol 106(4):329–331
Bonneville F, Savatovsky J, Chiras J (2007) Imaging of cerebellopontine angle lesions: an update. Part 1: enhancing extra-axial lesions. Eur Radiol 17(10):2472–2482
Cinalli G, Spennato P, Columbano L, Ruggiero C, Aliberti F, Trischitta V, Buonocore MC, Cianciulli E (2010) Neuroendoscopic treatment of arachnoid cysts of the quadrigeminal cistern: a series of 14 cases. J Neurosurg Pediatr 6(5):489–497
Cincu R, Agrawal A, Eiras J (2007) Intracranial arachnoid cysts: current concepts and treatment alternatives. Clin Neurol Neurosurg 109(10):837–843
Daoudi H, Lahlou G, Degos V, Sterkers O, Nguyen Y, Kalamarides M (2020) Improving facial nerve outcome and hearing preservation by different degrees of vestibular schwannoma resection guided by intraoperative facial nerve electromyography. Acta Neurochir 162(8):1983–1993
Hayes MJ, TerMaath SC, Crook TR, Killeffer JA (2019) A review on the effectiveness of surgical intervention for symptomatic intracranial arachnoid cysts in adults. World Neurosurg 123:259–272
Helland H, M L-J, K W (2010) Location, sidedness, and sex distribution of intracranial arachnoid cysts in a population-based sample. J Neurosurg doi: https://doi.org/10.3171/2009.11.JNS081663
Kameda K, Shono T, Hashiguchi K, Yoshida F, Sasaki T (2010) Effect of tumor removal on tinnitus in patients with vestibular schwannoma. J Neurosurg 112(1):152–157
Lang TA, Altman DG (2015) Basic statistical reporting for articles published in biomedical journals: the “Statistical Analyses and Methods in the Published Literature” or the SAMPL Guidelines. Int J Nurs Stud 52(1):5–9
Lanzino G, diPierro CG, Ruth RA, Helm G, Jane JA (1997) Recovery of useful hearing after posterior fossa surgery: the role of otoacoustic emissions: case report. Neurosurgery 41(2):469–472 discussion 472-473
No Authors (1995) Committee on Hearing and Equilibrium guidelines for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma). American Academy of Otolaryngology-Head and Neck Surgery Foundation, INC. Otolaryngol Head Neck Surg 113(3):179–180
Rabiei K, Hellström P, Högfeldt-Johansson M, Tisell M (2018) Does subjective improvement in adults with intracranial arachnoid cysts justify surgical treatment? J Neurosurg 128(1):250–257
Samii M, Carvalho GA, Schuhmann MU, Matthies C (1999) Arachnoid cysts of the posterior fossa. Surg Neurol 51(4):376–382
Tunes C, Flønes I, Helland C, Goplen F, Wester KG (2015) Disequilibrium in patients with posterior fossa arachnoid cysts. Acta Neurol Scand 132(1):23–30
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative (2008) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was not required for a retrospective study. Authorization was obtained from the ethics board of the French Society of Neurosurgery (n° IRB00011687 College de neurochirurgie IRB #1: 2020/32).
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgery general
Supplementary information
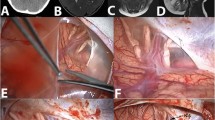
Supplementary Figure 1
– Examples of ABR. ABR on the left ear with normal waves I, III and V amplitude and normal wave V latency (< 5.8ms). ABR on the right ear show quantitative (decreased amplitude) and qualitative (wave V latency > 5.8ms) alterations (Patient 10) (JPG 118 kb)
Supplementary Figure 2
– Examples of VNG. (a) normoreflexia (Patient 12), (b) right compensated hyporeflexia (Patient 10) and (c) right non-compensated hyporeflexia (Patient 9) (JPG 96 kb)
Rights and permissions
About this article
Cite this article
Caudron, Y., Sterkers, O., Bernardeschi, D. et al. Objective improvement in adults with cerebellopontine angle arachnoid cysts after surgical treatment. Acta Neurochir 163, 753–758 (2021). https://doi.org/10.1007/s00701-021-04721-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-04721-6