Abstract
Parkinson’s disease (PD) is characterized by motor symptoms often experienced in concomitance with non-motor symptoms (NMS), such as depression, apathy, pain, sleep disorders, and urinary dysfunction. The present study aimed to explore the effect of safinamide treatment on NMS and quality of life in motor-fluctuating PD patients. VALE-SAFI is an observational single-centre study performed in fluctuating PD patients starting safinamide treatment and followed for 6 months. The effects of safinamide on NMS, sleep, fatigue, depression and pain were assessed through validated sales. Changes in the scales from baseline to the 6-month follow-up visit were analysed. 60 PD patients (66.67% males) were enrolled at baseline, and 45 patients completed the 6-month follow-up. PD patients improved motor symptoms at follow-up, with the significant reduction of motor fluctuations. The global score of the NMS Scale significantly decreased between baseline and the follow-up. Regarding pain domains, patients reported a significant improvement in discolouration and oedema/swelling. Further, a significant improvement was observed from baseline to follow-up in sleep quality measured through the Pittsburgh Sleep Quality Index, while no changes were documented in daytime sleepiness. No differences were found in depression and fatigue between baseline and follow-up. Finally, the patient’s perception of the impact of PD on functioning and well-being decreased from baseline to follow-up. The present findings confirmed the beneficial effect of safinamide on both motor and non-motor symptoms, also improving the quality of life of PD patients. Furthermore, these data support the positive effects of safinamide on pain and mood, as well as on sleep quality and continuity.
Similar content being viewed by others
Introduction
Motor symptoms such as bradykinesia, rigidity, postural instability and tremor are the main target of treatment in patients with Parkinson’s disease (PD). Nonetheless, these motor symptoms are often experienced in concomitance with non-motor symptoms (NMS), which include depression, psychosis, apathy, pain, sleep disorders, and urinary dysfunction (Poewe et al. 2017; Schapira et al. 2017; Church 2021). NMS have proven to be present as intrinsic events of the disease, but may also be exacerbated by the dopaminergic treatment (Zis et al. 2015; De Micco et al. 2021). Moreover, the presence of NMS in motor-fluctuating PD patients is consistently high, as recently documented (Fernandes et al. 2021). The frequency of NMS increases with the progression of the disease, in particular when motor fluctuations appear and show a strong negative impact on PD patient well-being and quality of life (Martinez-Martin et al. 2011; Antonini et al. 2012). Despite their clinical relevance, NMS are often under-recognized, and even when are identified through clinicians’ assessment or patients and/or caregivers reports, the range of treatment options is restricted (De Micco et al. 2021). This is probably due to the unclear pathophysiology of NMS, which seems to be related to dysfunction of both the dopaminergic and non-dopaminergic systems (Schapira et al. 2017).
Safinamide is a monoamine oxidase B inhibitors (iMAO-B) currently used as an add-on treatment to a stable dose of Levo-Dopa (LD) in motor-fluctuating PD patients (Mancini et al. 2018; García et al. 2021b). In the last years, safinamide become a useful treatment for both motor and non-motor symptoms in PD patients. Different studies demonstrated the beneficial effects of safinamide on NMS (Liguori et al. 2018a, b; Cattaneo et al. 2020; Geroin et al. 2020; Grigoriou et al. 2021), however, it is important to note that most of these studies had a retrospective design, included small groups of heterogeneous patients, or counted PD patients treated with safinamide in monotherapy. Therefore, the present observational single-centre study aimed to better understand the impact of safinamide treatment on motor impairment and NMS, namely fatigue, sleep depression and pain, as well as on the quality of life in motor-fluctuating PD patients.
Methods
Study design
For this observational single-centre study, patients affected by idiopathic PD diagnosed according to the UK Parkinson’s Disease Society Brain Bank criteria were enrolled between September 2018 and March 2020 at the UOSD Parkinson owing to the Neurology Clinic of the University Hospital of Rome “Tor Vergata”. All PD patients included in the study started treatment with safinamide according to clinical practice and guidelines. In particular, the starting administered dose of safinamide was 50 mg/day in the morning for two weeks and then increased to 100 mg/day from the third week of treatment.
The inclusion criteria were the following: (1) adult male and female patients (aged > 18 years); (2) patients able of giving signed informed consent; (3) patients on stable LD treatment, with or without a COMT inhibitor, and/or on a stable dose of dopamine-agonist for at least 4 weeks before the baseline visit; and (4) patients that would be treated with safinamide as an add-on therapy independently of this study. The exclusion criteria were: (1) patients enrolled in other studies and (2) patients in therapy with iMAO-B. In these patients, a washout period of at least 2 weeks was performed to include patients in the present study.
Patients with PD underwent a neurological evaluation and completed self-reported scales at baseline and after 6 months of treatment with safinamide.
Measures
The Non-Motor Symptoms Scale (NMSS) includes 30 items that assess a wide range of non-motor symptoms grouped in the following 9 domains: cardiovascular (2 items), sleep/fatigue (4 items), mood/cognition (6 items), perceptual problems/hallucinations (3 items), attention/memory (3 items), gastrointestinal tract (3 items); urinary (3 items), sexual function (2 items) and miscellaneous (4 items) (Chaudhuri et al. 2007; Cova et al. 2017).
PD patient’s quality of life was measured with the 39-Item Parkinson's Disease Questionnaire (PDQ-39), which is used to evaluate how often PD patients experience difficulties across 8 dimensions of daily living: mobility (10 items), activities of daily living (6 items), emotional well-being (6 items), stigma (4 items), social support (3 items), cognition (4 items), communication (3 items) and bodily discomfort (3 items) (Jenkinson et al. 1997; Galeoto et al. 2018).
Sleep quality was assessed through the Pittsburgh Sleep Quality Index (PSQI), which is based on 19 self-questions that combined form 7 component scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction (Buysse et al. 1989; Curcio et al. 2013). Moreover, excessive daytime sleepiness was evaluated through the Epworth Sleepiness Scale (ESS), which help to evaluate patient propensity to doze or fall asleep during 8 common daily activities (Johns 1991; Vignatelli et al. 2003).
Depression symptoms was measured with the Beck Depression Inventory-II (BDI-II), which is a 21-item self-report rating inventory that measures characteristic attitudes and symptoms of depression including: increase or decrease in sleep and appetite, agitation, concentration difficulty and loss of energy (Beck et al. 1996; Sica and Ghisi 2007).
The burden of pain in the context of PD was assessed through the King’s Parkinson’s Disease Pain Scale (King PD) (Jost et al. 2018). This scale is composed of 7 domains including 14 items: musculoskeletal pain (1 item); chronic pain (2 items); fluctuation-related pain (3 items); nocturnal pain (2 items); oro-facial pain (3 items); discoloration, oedema/swelling (2 items); radicular pain (1 item) (Jost et al. 2018).
The Parkinson’s Disease Fatigue Scale (PDFS-16) was used to measure fatigue which is one of the non-motor symptoms of Parkinson Disease (Brown et al. 2005; Siciliano et al. 2019). This scale allows to determine the presence of fatigue (7 items) and its impact on daily function (9 items) (Brown et al. 2005; Siciliano et al. 2019).
The Unified Parkinson's Disease Rating Scale part III (UPDRS-III) and part IV (UPDRS-IV) were used to perform an accurate motor examination (Fahn and Elton 1987).
Clinical data and scores were collected at baseline (T0) and at 6-month follow-up visit (T1). Moreover, tolerability and adverse events (AEs) were collected throughout the entire study period.
The study was approved by the local ethics committee (Tor Vergata CE 160/18) and followed CONSORT guidelines. All patients gave their written consent to the study.
Statistical analyses
Data were analysed using the SPSS statistical software package for Windows, release 25.0 (IBM. SPSS—Statistical Package for Social Sciences 2020). Continuous variables are expressed as mean and SD; categorical variables are presented as frequencies and percentages. The changes in primary and secondary outcomes between T0 (baseline) and T1 (follow-up) were also assessed using the Wilcoxon Rank-Sum test for comparing continuous variables. A value of p < 0.05 was considered statistically significant.
Results
Participants and clinical data
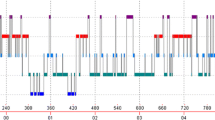
Sixty patients were enrolled in this study, completed the baseline evaluation and started safinamide treatment. After 6 months, 45 patients completed the follow-up visit and presented a significant reduction of both UPDRS-III and -IV (Table 1). Patients’ baseline demographic and clinical characteristics are presented in Fig. 1.
Global NMS and quality of life data
Regarding the NMS, the global score of the NMS scale significantly decreased between baseline and follow-up. Considering the single-domain analysis of NMS scale, there was only a significant reduction from baseline to follow-up on domain 9, which assesses different aspects of NMS in PD (pain among them).
PD Patients reported a significant decrease in PDQ-39 global score from baseline to follow-up, which indicates an improvement on patients’ quality of life after safinamide treatment. Moreover, at the follow-up visit, a significant change in different domains of the questionnaire was evident, namely emotional well-being, stigma, social support, communication. All NMS and quality of life data are reported in Table 1.
Depression and fatigue data
Regarding the depressive symptoms assessed by BDI-II, no differences were found between baseline and follow-up in the global score. The mean score of item 17, which measures irritability, showed a significant reduction from baseline to the follow-up visit. Moreover, no differences were evident between baseline and follow-up either in the global or in the sub-item scores of the PDFS-16 scale. All depression and fatigue data are reported in Table 2.
Pain data
Regarding pain evaluated through the KPDPS, only a significant result from baseline to follow-up was found, specifically a decrease in discolouration oedema/swelling (domain 6). Pain data are reported in Table 3.
Sleep and daytime sleepiness data
Finally, a significant reduction of the global score of the PSQI was observed from baseline to follow-up, indicating an increase in sleep quality. Moreover, different components of the PSQI significantly improved between baseline and follow-up (C1, subjective sleep quality; C2, sleep latency; C4, habitual sleep efficiency; C5, sleep disturbances; C7, daytime dysfunction). Considering the excessive daytime sleepiness, no significant changes were evident between baseline and follow-up on ESS scores (Table 4).
Discussion
NMS frequently occur in patients with PD, and it has been estimated that their prevalence can reach 90% along with the disease progression. Moreover, PD patients with motor fluctuations can present an increased prevalence of NMS from 80% to more than 90% in patients with high H&Y stages and long disease duration (Fernandes et al. 2021).
The main result of the present study is the significant reduction of NMSS global score between baseline and follow-up, which ameliorated in parallel with the significant improvement of UPDRS-III and -IV scores. These findings confirmed the beneficial effect of safinamide on both motor and non-motor PD symptoms. This significant improvement reflects also the amelioration of patients’ QoL and well-being measured through the PDQ-39. Consistently, several items related to the impact of PD symptoms on QoL improved from baseline to follow-up, thus highlighting the significant effect of safinamide on different aspects of daytime activities, social relations, and emotional well-being.
The significant improvement of domain 9 of NMSS, that measures pain and miscellaneous NMS, was also evident, and sleep quality and continuity significantly improved after safinamide treatment, which did not affect daytime vigilance, since the ESS scores did not change between baseline and follow-up.
NMS increasingly show a critical role in the clinical characterization of patients with PD due to their disabling nature, challenges in the management, and negative impact on patients’ and caregivers’ well-being. Sleep disorders and psychiatric symptoms are the main NMS in motor-fluctuating PD patients, although pain and fatigue commonly affect those patients (Fernandes et al. 2021). There is still no evidence of beneficial effects of dopaminergic treatment on the entire NMS spectrum, possibly since NMS may refer to multi-system networks, involving not only the dopaminergic but also the other monoaminergic or orexinergic, glutamatergic and GABA-ergic systems (Miguelez et al. 2020). Therefore, it has been suggested that the best hypothetical treatment for NMS should present a multi-neurotransmitting system effect.
One of the most recent drugs approved for the treatment of motor-fluctuating PD patients is safinamide, which consists of an orally administered α-aminoamide derivative able to target both dopaminergic and glutaminergic systems through its multiple mechanism of action. In particular, safinamide can act as a selective and reversible iMAO-B and can also block voltage-dependent sodium and calcium channels, with inhibition of dopamine reuptake and modulation of glutamate and GABA release (Bianchi et al. 2019).
Aside from motor symptoms improvement, different recent reports demonstrated a significant effect of safinamide on NMS (Bianchi et al. 2019; Geroin et al. 2020; De Micco et al. 2021; Grigoriou et al. 2021; Peña et al. 2021). The single open-label prospective study on different NMS performed in Spain included fifty PD patients but not all were treated with safinamide as an add-on treatment to LD (García et al. 2021a, b; Labandeira et al. 2021; Santos García et al. 2021). The first published result showed the significant reduction of NMSS global score after 6 months of safinamide treatment in PD patients. Moreover, the items related to sleep and fatigue, mood, apathy, attention and memory, gastrointestinal and urinary symptoms, and pain were significantly reduced at the follow-up (García et al. 2021b). Following this report, other results have been published from this multi-centre study, but separately analysed, documenting an improvement of sleep, daytime sleepiness, depression, and pain (García et al. 2021a; Labandeira et al. 2021; Santos García et al. 2021). Considering the importance of a comprehensive and prospective analysis including an homogeneous large sample of motor-fluctuating PD patients treated by safinamide as add-on treatment to LD, the present study collectively evaluated all these NMS at baseline and after 6 months of stable treatment in a group of sixty motor-fluctuating PD patients.
Pain improvement after safinamide treatment was evident already in the post-hoc analysis of the registrative trials (Cattaneo et al. 2020). Consistently, real-world data confirmed this preliminary observation on pain symptoms also through the use of self-reported questionnaires and scales that assess this specific NMS (Chaudhuri et al. 2007; Cova et al. 2017). In line with this evidence, the present study documented a significant reduction from baseline to follow-up in discolouration oedema/swelling (domain 6 of the KPPS scale) in PD patients treated with safinamide, which was already described in previous studies (Geroin et al. 2020; García et al. 2021a; Grigoriou et al. 2021). Regarding mood, the improvement in irritability, a symptom commonly reported during a depressive episode and a frequent behavioural symptom in PD patients, was evident at follow-up. Further investigations regarding the effect of the drug on irritability and behaviour should be planned to confirm this preliminary data. Finally, a significant effect of safinamide on subjective sleep quality, sleep latency, sleep efficiency, and then on sleep disturbances was observed between baseline and follow-up. This finding concords with previous and preliminary reports about the effects of safinamide on sleep measured either objectively through polysomnographic recording or subjectively with different scales (Liguori et al. 2018a, b; Santos García et al. 2021).
No effects of safinamide treatment were evident on fatigue, although item 7 that measured daytime productivity presented a trend in improvement at follow-up, as well as on daytime sleepiness, which can be considered as a positive indicator since other dopaminergic drugs have been associated with sleep attacks and excessive daytime sleepiness (Hauser et al. 2000; Chaudhuri et al. 2002; O’Suilleabhain and Dewey 2002; Valko et al. 2010; Yeung and Cavanna 2014). Notably, the beneficial effect of safinamide on daytime dysfunction was evident on the PSQI component, with a reduction of this component at follow-up.
In conclusion, the present study confirmed the previous evidence about the beneficial effect of safinamide on NMS in motor-fluctuating PD patients. The mechanism of action of the drug, including not only the dopaminergic effect but also the modulation of glutamatergic and GABA-ergic systems (Morari et al. 2018; Pisanò et al. 2020), may substantiate the clinical evidence achieved in this study. The open-label design and the 6-month follow-up analysis were limitations of this study. Further investigations with a longer follow-up should be planned to test the maintenance of the positive effect on NMS and its correlation with motor symptoms and motor fluctuations.
Data availability statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Antonini A, Barone P, Marconi R et al (2012) The progression of non-motor symptoms in Parkinson’s disease and their contribution to motor disability and quality of life. J Neurol 259:2621–2631. https://doi.org/10.1007/s00415-012-6557-8
Beck AT, Steer RA, Brown G (1996) Beck depression inventory–II. Psychol Assess
Bianchi MLE, Riboldazzi G, Mauri M, Versino M (2019) Correction to: Efficacy of safinamide on non-motor symptoms in a cohort of patients affected by idiopathic Parkinson’s disease (Neurological Sciences, (2019), 40, 2, (275–279), https://doi.org/10.1007/s10072-018-3628-3). Neurol Sci 40:281. https://doi.org/10.1007/s10072-018-3658-x
Brown RG, Dittner A, Findley L, Wessely SC (2005) The Parkinson fatigue scale. Park Relat Disord 11:49–55. https://doi.org/10.1016/j.parkreldis.2004.07.007
Buysse DJ, Reynolds CF III, Monk TH et al (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Cattaneo C, Jost WH, Bonizzoni E (2020) Long-term efficacy of safinamide on symptoms severity and quality of life in fluctuating Parkinson’s Disease patients. J Parkinsons Dis 10:89–97. https://doi.org/10.3233/JPD-191765
Chaudhuri KR, Pal S, Brefel-Courbon C (2002) “Sleep attacks” or “unintended sleep episodes” occur with dopamine agonists: Is this a class effect? Drug Saf 25:473–483. https://doi.org/10.2165/00002018-200225070-00001
Chaudhuri KR, Martinez-Martin P, Brown RG et al (2007) The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: results from an international pilot study. Mov Disord 22:1901–1911
Church FC (2021) Review treatment options for motor and non-motor symptoms of parkinson’s disease. Biomolecules. https://doi.org/10.3390/biom11040612
Cova I, Di Battista ME, Vanacore N et al (2017) Validation of the Italian version of the non motor symptoms scale for Parkinson’s disease. Parkinsonism Relat Disord 34:38–42
Curcio G, Tempesta D, Scarlata S, et al (2013) Validity of the Italian Version of the Pittsburgh Sleep Quality Index (PSQI) 511–519. https://doi.org/10.1007/s10072-012-1085-y
De Micco R, Satolli S, Siciliano M et al (2021) Effects of safinamide on non-motor, cognitive, and behavioral symptoms in fluctuating Parkinson’s disease patients: a prospective longitudinal study. Neurol Sci. https://doi.org/10.1007/s10072-021-05324-w
Fahn S, Elton R (1987) Unified Parkinson’s Disease Rating Scale. In: Fahn S, Marsden C, Calne D, Goldstein M (eds) Recent developments in Parkinson’s disease. MacMillan Healthcare Information, Florham Park, pp 153–164
Fernandes M, Pierantozzi M, Stefani A et al (2021) Frequency of non-motor symptoms in Parkinson’s Patients with motor fluctuations. Front Neurol. https://doi.org/10.3389/fneur.2021.678373
Galeoto G, Colalelli F, Massai P et al (2018) Quality of life in Parkinson’s disease: Italian validation of the Parkinson’s Disease Questionnaire (PDQ-39-IT). Neurol Sci 39:1903–1909
García DS, Baña RY, Guerra CL et al (2021a) Pain improvement in parkinson’s disease patients treated with safinamide: results from the safinonmotor study. J Pers Med. https://doi.org/10.3390/JPM11080798
García DS, Guerra CL, Baña RY et al (2021b) Safinamide improves non-motor symptoms burden in parkinson’s disease: an open-label prospective study. Brain Sci 11:1–15. https://doi.org/10.3390/brainsci11030316
Geroin C, Di Vico IA, Squintani G et al (2020) Effects of safinamide on pain in Parkinson’s disease with motor fluctuations: an exploratory study. J Neural Transm 127:1143–1152. https://doi.org/10.1007/s00702-020-02218-7
Grigoriou S, Martínez-Martín P, Ray Chaudhuri K et al (2021) Effects of safinamide on pain in patients with fluctuating Parkinson’s disease. Brain Behav 11:1–9. https://doi.org/10.1002/brb3.2336
Hauser RA, Gauger L, Anderson WMD, Zesiewicz TA (2000) Pramipexole-induced somnolence and episodes of daytime sleep. Mov Disord 15:658–663. https://doi.org/10.1002/1531-8257(200007)15:4%3c658::AID-MDS1009%3e3.0.CO;2-N
Jenkinson C, Fitzpatrick RAY, Peto VIV et al (1997) The Parkinson’s Disease Questionnaire (PDQ-39): development and validation of a Parkinson’s disease summary index score. Age Ageing 26:353–357
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545. https://doi.org/10.1093/sleep/14.6.540
Jost WH, Rizos A, Odin P et al (2018) King’s Parkinson’s Disease Pain Scale. Nervenarzt 89:178–183
Labandeira CM, Alonso Losada MG, Yáñez Baña R et al (2021) Effectiveness of safinamide over mood in Parkinson’s disease patients: secondary analysis of the open-label study SAFINONMOTOR. Adv Ther 38:5398–5411. https://doi.org/10.1007/s12325-021-01873-w
Liguori C, Mercuri NB, Stefani A, Pierantozzi M (2018a) Effective treatment of restless legs syndrome by safinamide in Parkinson’s disease patients. Sleep Med 41:113–114. https://doi.org/10.1016/j.sleep.2017.09.017
Liguori C, Stefani A, Ruffini R et al (2018b) Safinamide effect on sleep disturbances and daytime sleepiness in motor fluctuating Parkinson’s disease patients: a validated questionnaires-controlled study. Park Relat Disord 57:80–81. https://doi.org/10.1016/j.parkreldis.2018.06.033
Mancini F, Di Fonzo A, Lazzeri G et al (2018) Real life evaluation of safinamide effectiveness in Parkinson’s disease. Neurol Sci 39:733–739. https://doi.org/10.1007/s10072-018-3272-y
Martinez-Martin P, Rodriguez-Blazquez C, Kurtis MM, Chaudhuri KR (2011) The impact of non-motor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov Disord 26:399–406. https://doi.org/10.1002/mds.23462
Miguelez C, De Deurwaerdère P, Sgambato V (2020) Editorial: non-dopaminergic systems in Parkinson’s Disease. Front Pharmacol 11:10–11. https://doi.org/10.3389/fphar.2020.593822
Morari M, Brugnoli A, Pisanò CA et al (2018) Safinamide differentially modulates in vivo glutamate and GABA release in the rat hippocampus and basal ganglia. J Pharmacol Exp Ther 364:198–206. https://doi.org/10.1124/jpet.117.245100
O’Suilleabhain PE, Dewey RB (2002) Contributions of dopaminergic drugs and disease severity to daytime sleepiness in Parkinson disease. Arch Neurol 59:986–989. https://doi.org/10.1001/archneur.59.6.986
Peña E, Borrué C, Mata M et al (2021) Impact of SAfinamide on depressive symptoms in parkinson’s disease patients (SADness-PD Study): a multicenter retrospective study. Brain Sci 11:1–11. https://doi.org/10.3390/brainsci11020232
Pisanò CA, Brugnoli A, Novello S et al (2020) Safinamide inhibits in vivo glutamate release in a rat model of Parkinson’s disease. Neuropharmacology 167:108006. https://doi.org/10.1016/j.neuropharm.2020.108006
Poewe W, Seppi K, Tanner CM et al (2017) Parkinson disease. Nat Rev Dis Prim 3:1–21. https://doi.org/10.1038/nrdp.2017.13
Santos García D, Cabo López I, Labandeira Guerra C et al (2021) Safinamide improves sleep and daytime sleepiness in Parkinson’s disease: results from the SAFINONMOTOR study. Neurol Sci. https://doi.org/10.1007/s10072-021-05607-2
Schapira AHV, Chaudhuri KR, Jenner P (2017) Non-motor features of Parkinson disease. Nat Rev Neurosci 18:435–450. https://doi.org/10.1038/nrn.2017.62
Sica C, Ghisi M (2007) The Italian versions of the Beck Anxiety Inventory and the Beck Depression Inventory-II: Psychometric properties and discriminant power. In: Leading-edge psychological tests and testing research. Nova Science Publishers, Sica, Claudio: Dipartimento di Psicologia, University of Firenze Via San Niccolo, Firenze, Italy, 93, 50125, claudio.sica@unifi.it, pp 27–50
Siciliano M, Chiorri C, De Micco R et al (2019) Fatigue in Parkinson’s disease: Italian validation of the Parkinson Fatigue Scale and the Fatigue Severity Scale using a Rasch analysis approach. Park Relat Disord 65:105–110. https://doi.org/10.1016/j.parkreldis.2019.05.028
Valko PO, Waldvogel D, Weller M et al (2010) Fatigue and excessive daytime sleepiness in idiopathic Parkinson’s disease differently correlate with motor symptoms, depression and dopaminergic treatment. Eur J Neurol 17:1428–1436. https://doi.org/10.1111/j.1468-1331.2010.03063.x
Vignatelli L, Plazzi G, Barbato A et al (2003) Italian version of the Epworth sleepiness scale: external validity. Neurol Sci 23:295–300. https://doi.org/10.1007/s100720300004
Yeung EYH, Cavanna AE (2014) Sleep attacks in patients with Parkinson’s disease on dopaminergic medications: a systematic review. Mov Disord Clin Pract 1:307–316. https://doi.org/10.1002/mdc3.12063
Zis P, Erro R, Walton CC et al (2015) The range and nature of non-motor symptoms in drug-naive Parkinson’s disease patients: a state-of-the-art systematic review. Park Dis. https://doi.org/10.1038/npjparkd.2015.13
Acknowledgements
This study was supported by an unrestricted grant from Zambon to A.S.
Funding
Open access funding provided by Università degli Studi di Roma Tor Vergata within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was supported by an unrestricted grant from Zambon to A.S. No other financial disclosures or conflict of interests related to this study are present.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
De Masi, C., Liguori, C., Spanetta, M. et al. Non-motor symptoms burden in motor-fluctuating patients with Parkinson’s disease may be alleviated by safinamide: the VALE-SAFI study. J Neural Transm 129, 1331–1338 (2022). https://doi.org/10.1007/s00702-022-02538-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-022-02538-w