Abstract
Objectives
The aim of this study was to conduct a systematic review to compare the survival rates between short implants (length < 10 mm) versus standard-length implants (≥ 10 mm) inserted in grafted bone. As secondary outcomes, marginal bone loss and survival rates of the implant supported prostheses were also analysed.
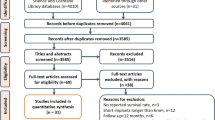
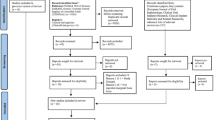
Materials and methods
Randomised controlled trials (RCT) that compared both techniques were searched on three electronic databases till June 2016, a manual search was performed on the bibliography of the collected articles, and the authors were contacted for additional references. The estimates of the interventions were expressed in relative risk (RR), mean implant survival rates and mean differences in marginal bone.
Results
Eight RCTs were included in this study. From a total of 458 short implants, 15 failed (mean survival rates = 96.7%), While from 488 regular implants, 13 failed (mean survival rates = 97.3%). The technique did not significantly affect: the implant failure rate (P > 0.05), with RR of 1.34 (95% CI 0.67–2.87), the mean differences of marginal bone loss (P = 0.18; MD − 0.04 mm [− 0.10; 0.02] 95% CI), at loading or prosthesis failures rates (RR:0.98; 95% CI 0.40–2.41). The mean differences of marginal bone at 1 year follow-up (post loading) presented significant marginal changes in the short implant group (P = 0.002; MD − 0.10 mm [− 0.16; − 0.03] 95% CI) although a significant high heterogeneity was found between groups.
Conclusions
This systematic review suggests no difference between both techniques in the treatment of atrophic arches. However, more long-term RCTs are needed to evaluate the predictability at the long run.
Clinical relevance
The use of short implants might be considered an alternative treatment, since it usually requires fewer surgical phases and tends to be a more affordable option.






Similar content being viewed by others
References
Muneeb AKB, Jamil B (2013) Causes and pattern of partial edentulism/exodontia and its association with age and gender: semi rural population, Baqai Dental college, Karachi, Pakistan. Idjsr 1(3):13–18
van der Velden U, Amaliya A, Loos BG, Timmerman MF, van der Weijden FA, Winkel EG, Abbas F (2015) Java project on periodontal diseases: causes of tooth loss in a cohort of untreated individuals. J Clin Periodontol 42(9):824–831. https://doi.org/10.1111/jcpe.12446
Baelum V, van Palenstein HW, Hugoson A, Yee R, Fejerskov O (2007) A global perspective on changes in the burden of caries and periodontitis: implications for dentistry. J Oral Rehabil 34(12):872–906; discussion 940. https://doi.org/10.1111/j.1365-2842.2007.01799.x
Madhankumar S, Mohamed K, Natarajan S, Kumar VA, Athiban I, Padmanabhan TV (2015) Prevalence of partial edentulousness among the patients reporting to the Department of Prosthodontics Sri Ramachandra University Chennai, India: an epidemiological study. J Pharm Bioallied Sci 7(Suppl 2):S643–S647. https://doi.org/10.4103/0975-7406.163580
Adell R, Lekholm U, Rockler B, Branemark PI (1981) A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 10(6):387–416
Pennington JPS (2012) Improving quality of life using removable and fixed implant prostheses. Compend Contin Educ Dent 33(4):268–270 272, 274-266
Karthik K, Sivakumar S, Thangaswamy V (2013) Evaluation of implant success: a review of past and present concepts. J Pharm Bioallied Sci 5(Suppl 1):S117–S119. https://doi.org/10.4103/0975-7406.113310
Santiago Junior JF, Pellizzer EP, Verri FR, de Carvalho PS (2013) Stress analysis in bone tissue around single implants with different diameters and veneering materials: a 3-D finite element study. Mater Sci Eng C Mater Biol Appl 33(8):4700–4714
Urban IA, Jovanovic SA, Lozada JL (2009) Vertical ridge augmentation using guided bone regeneration (GBR) in three clinical scenarios prior to implant placement: a retrospective study of 35 patients 12 to 72 months after loading. Int J Oral Maxillofac Implants 24(3):502–510
Monje A, Pikos MA, Chan HL, Suarez F, Gargallo-Albiol J, Hernandez-Alfaro F, Galindo-Moreno P, Wang HL (2014) On the feasibility of utilizing allogeneic bone blocks for atrophic maxillary augmentation. Biomed Res Int 2014:814578. https://doi.org/10.1155/2014/814578
Pjetursson BE, Tan WC, Zwahlen M, Lang NP (2008) A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol 35(8 Suppl):216–240. https://doi.org/10.1111/j.1600-051X.2008.01272.x
Schwarz L, Schiebel V, Hof M, Ulm C, Watzek G, Pommer B (2015) Risk factors of membrane perforation and postoperative complications in sinus floor elevation surgery: review of 407 augmentation procedures. J Oral Maxillofac Surg 73(7):1275–1282. https://doi.org/10.1016/j.joms.2015.01.039
Jensen AT, Jensen SS, Worsaae N (2016) Complications related to bone augmentation procedures of localized defects in the alveolar ridge. A retrospective clinical study. Oral Maxillofac Surg 20(2):115–122. https://doi.org/10.1007/s10006-016-0551-8
Raviv E, Turcotte A, Harel-Raviv M (2010) Short dental implants in reduced alveolar bone height. Quintessence Int 41(7):575–579
das Neves FD, Fones D, Bernardes SR, do Prado CJ, Neto AJ (2006) Short implants—an analysis of longitudinal studies. Int J Oral Maxillofac Implants 21(1):86–93
Neldam CA, Pinholt EM (2012) State of the art of short dental implants: a systematic review of the literature. Clin Implant Dent Relat Res 14(4):622–632. https://doi.org/10.1111/j.1708-8208.2010.00303.x
Piero P, Lorenzo C, Daniele R, Rita G, Luca P, Giorgio P (2015) Survival of short dental implants ≤7 mm: A review. Int J Contemp Dent Med Rev 2015:Article ID: 011015. 10.15713/ins.ijcdmr.89
Egger MSG, Altman DG (2008) Chapter 2. Principles of and procedures for systematic reviews. BMJ Publishing Group, London. https://doi.org/10.1002/9780470693926.ch2
Pistilli R, Felice P, Piattelli M, Gessaroli M, Soardi E, Barausse C, Buti J, Corvino V (2013) Posterior atrophic jaws rehabilitated with prostheses supported by 5 x 5 mm implants with a novel nanostructured calcium-incorporated titanium surface or by longer implants in augmented bone. One-year results from a randomised controlled trial. Eur J Oral Implantol 6(4):343–357
Pistilli R, Felice P, Cannizzaro G, Piatelli M, Corvino V, Barausse C, Buti J, Soardi E, Esposito M (2013) Posterior atrophic jaws rehabilitated with prostheses supported by 6 mm long 4 mm wide implants or by longer implants in augmented bone. One-year post-loading results from a pilot randomised controlled trial. Eur J Oral Implantol 6(4):359–372
Felice P, Cannizzaro G, Barausse C, Pistilli R, Esposito M (2014 Winter) Short implants versus longer implants in vertically augmented posterior mandibles: a randomised controlled trial with 5-year after loading follow-up. Eur J Oral Implantol. 7(4):359–369
Esposito M, Pistilli R, Barausse C, Felice P (2014 Winter) Three-year results from a randomised controlled trial comparing prostheses supported by 5-mm long implants or by longer implants in augmented bone in posterior atrophic edentulous jaws. Eur J Oral Implantol 7(4):383–395
Felice P, Pistilli R, Barausse C, Bruno V, Trullenque-Eriksson A, Esposito M (2015 Winter) Short implants as an alternative to crestal sinus lift: a 1-year multicentre randomised controlled trial. Eur J Oral Implantol. 8(4):375–384
Esposito M, Barausse C, Pistilli R, Sammartino G, Grandi G, Felice P (2015 Autumn) Short implants versus bone augmentation for placing longer implants in atrophic maxillae: one-year post-loading results of a pilot randomised controlled trial. Eur J Oral Implantol. 8(3):257–268
Thoma DS, Haas R, Tutak M, Garcia A, Schincaglia GP, Hämmerle CH (2015 Jan) Randomized controlled multicentre study comparing short dental implants (6 mm) versus longer dental implants (11-15 mm) in combination with sinus floor elevation procedures. Part 1: demographics and patient-reported outcomes at 1 year of loading. J Clin Periodontol 42(1):72–80. https://doi.org/10.1111/jcpe.12323
Guljé FL, Raghoebar GM, Vissink A, Meijer HJA. (2014) Single crowns in the resorbed posterior maxilla supported by either 6-mm implants or by 11-mm implants combined with sinus floor elevation surgery: A 1-year randomised controlled trial. Eur J Oral Implantol 7(3):247–55
Esposito M, Felice P, Worthington HV (2014) Interventions for replacing missing teeth: augmentation procedures of the maxillary sinus. Cochrane Database Syst Rev (5):CD008397. doi:https://doi.org/10.1002/14651858.CD008397.pub2
Koszuta P, Grafka A, Koszuta A, Lopucki M, Szymanska J (2015) Effects of selected factors on the osseointegration of dental implants. Prz Menopauzalny 14(3):184–187. https://doi.org/10.5114/pm.2015.54343
Chambrone L, Preshaw PM, Ferreira JD, Rodrigues JA, Cassoni A, Shibli JA (2014) Effects of tobacco smoking on the survival rate of dental implants placed in areas of maxillary sinus floor augmentation: a systematic review. Clin Oral Implants Res 25(4):408–416. https://doi.org/10.1111/clr.12186
Bezerra Ferreira JD, Rodrigues JA, Piattelli A, Iezzi G, Gehrke SA, Shibli JA (2016) The effect of cigarette smoking on early osseointegration of dental implants: a prospective controlled study. Clin Oral Implants Res 27(9):1123–1128. https://doi.org/10.1111/clr.12705
Holahan CMWJ, Weaver A, Assad D, Koka S (2011) Relationship between systemic bone mineral density and local bone quality as effectors of dental implant survival. Clin Implant Dent Relat Res 13(1):29–33. https://doi.org/10.1111/j.1708-8208.2009.00206.x
Goiato MC, dos Santos DM, Santiago JF Jr, Moreno A, Pellizzer EP (2014) Longevity of dental implants in type IV bone: a systematic review. Int J Oral Maxillofac Surg 43(9):1108–1116. https://doi.org/10.1016/j.ijom.2014.02.016
Nisand D (2000) Renouard F (2014) short implant in limited bone volume. Periodontol 66(1):72–96. https://doi.org/10.1111/prd.12053
Engelhardt S, Papacosta P, Rathe F, Ozen J, Jansen JA, Junker R (2015) Annual failure rates and marginal bone-level changes of immediate compared to conventional loading of dental implants. A systematic review of the literature and meta-analysis. Clin Oral Implants Res 26(6):671–687. https://doi.org/10.1111/clr.12363
Chrcanovic BR, Albrektsson T, Wennerberg A (2015) Dental implants inserted in fresh extraction sockets versus healed sites: a systematic review and meta-analysis. J Dent 43(1):16–41. https://doi.org/10.1016/j.jdent.2014.11.007
Isidor F (2006) Influence of forces on peri-implant bone. Clin Oral Implants Res 17(Suppl 2):8–18. https://doi.org/10.1111/j.1600-0501.2006.01360.x
Blanes RJ (2009) To what extent does the crown-implant ratio affect the survival and complications of implant-supported reconstructions? A systematic review. Clin Oral Implants Res 20(Suppl 4):67–72. https://doi.org/10.1111/j.1600-0501.2009.01762.x
Sotto-Maior BS, Senna PM, da Silva-Neto JP, de Arruda Nobilo MA, Del Bel Cury AA (2015) Influence of crown-to-implant ratio on stress around single short-wide implants: a photoelastic stress analysis. J Prosthodont 24(1):52–56. https://doi.org/10.1111/jopr.12171
Ramos Verri F, Santiago Junior JF, de Faria Almeida DA, de Oliveira GB, de Souza Batista VE, Marques Honorio H, Noritomi PY, Pellizzer EP (2015) Biomechanical influence of crown-to-implant ratio on stress distribution over internal hexagon short implant: 3-D finite element analysis with statistical test. J Biomech 48(1):138–145. https://doi.org/10.1016/j.jbiomech.2014.10.021
Albrektsson TZG, Worthington P, Eriksson AR (1986) The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants 1(1):11–25
Qian J, Wennerberg A, Albrektsson T (2012) Reasons for marginal bone loss around oral implants. Clin Implant Dent Relat Res 14(6):792–807. https://doi.org/10.1111/cid.12014
Sanz M, Vignoletti F (2015) Key aspects on the use of bone substitutes for bone regeneration of edentulous ridges. Dent Mater 31(6):640–647. https://doi.org/10.1016/j.dental.2015.03.005
Monje A, Suarez F, Galindo-Moreno P, Garcia-Nogales A, Fu JH, Wang HL (2014) A systematic review on marginal bone loss around short dental implants (<10 mm) for implant-supported fixed prostheses. Clin Oral Implants Res 25(10):1119–1124. https://doi.org/10.1111/clr.12236
Galindo-Moreno P, Fauri M, Avila-Ortiz G, Fernandez-Barbero JE, Cabrera-Leon A, Sanchez-Fernandez E (2005) Influence of alcohol and tobacco habits on peri-implant marginal bone loss: a prospective study. Clin Oral Implants Res 16(5):579–586. https://doi.org/10.1111/j.1600-0501.2005.01148.x
Funding
The work was supported by the Evidence Based Dentistry Center, Lisbon University and Implant Dentistry Department, European University of Madrid.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this systematic review.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Palacios, J.A.V., Garcia, J.J., Caramês, J.M.M. et al. Short implants versus bone grafting and standard-length implants placement: a systematic review. Clin Oral Invest 22, 69–80 (2018). https://doi.org/10.1007/s00784-017-2205-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-017-2205-0