Abstract
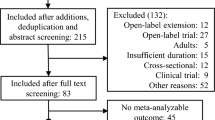
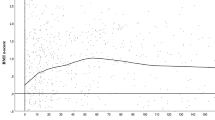
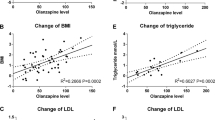
To analyze weight gain, metabolic hormones, and homocysteine (Hcys) levels in children and adolescents on antipsychotics (AP) during a year-long follow-up. 117 patients, AP-naïve or quasi-naïve (less than 30 days on AP), were included. Weight, body mass index (BMI), BMI z-score (z-BMI), and levels of leptin, insulin, insulin resistance (HOMA-IR), adiponectin, ghrelin, thyroid stimulating hormone (TSH), free thyroxine (FT4), and Hcys were measured at baseline, and at 3, 6, and 12 months, while patients remained on the same AP. Patients (mean age: 14.4 ± 3 years; 64.1 % male) were on risperidone (N = 84), olanzapine (N = 20) or quetiapine (N = 13) from baseline up to 1-year follow-up and significantly increased weight (5.8 ± 4.3 kg at 3-month, 8.1 ± 6.1 kg at 6-month, and 11.6 ± 7.0 kg at 1 year), BMI, and z-BMI. Leptin levels significantly increased from baseline to 3 and 6 months, as did TSH levels from baseline to 3 months, while FT4 levels decreased from baseline to 3 and 6 months. Patients with BMI >85th percentile at baseline (N = 16) significantly increased weight, BMI, and z-BMI, more than patients with normal BMI over time. Higher baseline levels of insulin, HOMA-IR, and leptin were associated with increased weight/BMI during follow-up, while higher baseline levels of FT4, adiponectin, and ghrelin were associated with lower weight/BMI during follow-up. All AP were associated with increased weight and BMI/z-BMI in all of the assessments; however, at 1-year assessment, this increase was significantly higher for patients on quetiapine. Both higher baseline levels of insulin, HOMA-IR, and leptin, as well as being overweight/obese at baseline were associated with increased weight/BMI during 1-year follow-up in children and adolescents on AP. Awareness of weight-related parameters in this population may help inform decisions regarding AP prescriptions.


Similar content being viewed by others
References
Baeza I, De la Serna E, Calvo-Escalona R, Morer A, Merchán-Naranjo J, Tapia C, Martínez-Cantarero MC, Andrés P, Alda JA, Sánchez B, Arango C, Castro-Fornieles J (2014) Antipsychotic use in children and adolescents. A 1-year follow-up study. J Clin Psychopharmacol 5:613–619
Olfson M, Blanco C, Liu SM, Wang S, Correll CU (2012) National trends in the office-based treatment of children, adolescents, and adults with antipsychotics. Arch Gen Psychiatry 69:1247–1256
Fraguas D, Correll CU, Merchán-Naranjo J, Rapado-Castro M, Parellada M, Moreno C, Arango C (2011) Efficacy and safety of second-generation antipsychotics in children and adolescents with psychotic and bipolar spectrum disorders: comprehensive review of prospective head-to-head and placebo-controlled comparisons. Eur Neuropsychopharmacol 21:621–645
Arango C (2015) Present and future of developmental neuropsychopharmacology. Eur Neuropsychopharmacol 25:703–712
Correll CU, Manu P, Olshanskiy V, Napolitano B, Kane JM, Malhotra AK (2009) Cardiometabolic risk of second-generation antipsychotic medications during first-time use in children and adolescents. JAMA 302:1765–1773
Fleischhaker C, Heiser P, Hennighausen K, Herpertz-Dahlmann B, Holtkamp K, Mehler-Wex C, Rauh R, Remschmidt H, Schulz E, Warnke A (2006) Clinical drug monitoring in child and adolescent psychiatry: side effects of atypical neuroleptics. J Child Adolesc Psychopharmacol 16:308–316
Safer DJ (2004) A comparison of risperidone-induced weight gain across the age span. J Clin Psychopharmacol 24:429–436
Martínez-Ortega JM, Funes-Godoy S, Díaz-Atienza F, Gutiérrez-Rojas L, Pérez-Costillas L, Gurpegui M (2013) Weight gain and increase of body mass index among children and adolescents treated with antipsychotics: a critical review. Eur Child Adolesc Psychiatry 22:457–479
Cohn TA, Sernyak MJ (2006) Metabolic monitoring for patients treated with antipsychotic medications. Can J Psychiatry 51:492–501
Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC (1999) Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry 156:1686–1696
Deng C, Weston-Green K, Huang X (2010) The role of histaminergic H1 and H3 receptors in food intake: a mechanism for atypical antipsychotic-induced weight gain? Prog Neuropsychopharmacol Biol Psychiatry 34:1–4
Baptista T (1999) Body weight gain induced by antipsychotic drugs: mechanisms and management. Acta Psychiatr Scand 100:3–16
Cuerda C, Velasco C, Merchán-Naranjo J, García-Peris P, Arango C (2014) The effects of second-generation antipsychotics on food intake, resting energy expenditure and physical activity. Eur J Clin Nutr 68:146–152
Havel PJ (2001) Peripheral signals conveying metabolic information to the brain: short-term and long-term regulation of food intake and energy homeostasis. Exp Biol Med (Maywood). 226:963–977
Friedman JM (2002) The function of leptin in nutrition, weight, and physiology. Nutr Rev 60:S1–14 (discussion S68–84, 85–87)
Sentissi O, Epelbaum J, Olié JP, Poirier MF (2008) Leptin and ghrelin levels in patients with schizophrenia during different antipsychotics treatment: a review. Schiz Bull 34:1189–1199
Barsh GS, Schwartz MW (2002) Genetic approaches to studying energy balance: perception and integration. Nat Rev Genet 3:589–600
Nakazato M, Murakami N, Date Y, Kojima M, Matsuo H, Kangawa K, Matsukura S (2001) A role for ghrelin in the central regulation of feeding. Nature 409:194–198
Lucidi P, Murdolo G, Di Loreto C, Parlanti N, De Cicco A, Ranchelli A, Fatone C, Taglioni C, Fanelli C, Santeusanio F, De Feo P (2004) Meal intake similarly reduces circulating concentrations of octanoyl and total ghrelin in humans. J Endocrinol Invest 27:RC12–5
Heilbronn LK, Smith SR, Ravussin E (2003) The insulin-sensitizing role of the fat derived hormone adiponectin. Curr Pharm Des 9:1411–1418
Weyer C, Funahashi T, Tanaka S, Hotta K, Matsuzawa Y, Pratley RE, Tataranni PA (2001) Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinmia. J Clin Endocrinol Metab 86:1930–1935
Reinehr T (2010) Obesity and thyroid function. Mol Cel Endocrinol 316:165–171
Reinehr T (2011) Thyroid function in the nutritionally obese child and adolescent. Curr Opin Pediatrics 23:415–420
Aypak C, Türedi O, Yüce A, Görpelioğlu S (2013) Thyroid-stimulating hormone (TSH) level in nutritionally obese children and metabolic co-morbidity. J Pediatr Endocrinol Metab 26:703–708
Jacobellis G, Ribaudo MC, Zappaterreno A, Iannucci CV, Leonetti F (2005) Relationship of thyroid function with body mass index, leptin, insulin sensitivity and adiponectin in euthyroid obese women. Clin Endocrinol 62:487–491
Roef G, Lapauw B, Goemaere S, Zmierczak HG, Toye K, Kaufman JM, Taes Y (2012) Body composition and metabolic parameters are associated with variation in thyroid hormone levels among euthyroid young men. Eur J Endocrinol 167:719–726
Martí-Carvajal AJ, Solà I, Lathyris D, Karakitsiou DE, Simancas-Racines D (2013) Homocysteine-lowering interventions for preventing cardiovascular events. Cochrane Database Syst Rev 1:CD006612. doi:10.1002/14651858.CD006612.pub3
Karatela RA, Sainani GS (2009) Plasma homocysteine in obese, overweight and hypertensive subjects in Mumbai. Indian Heart 61:156–159
Vayá A, Carmona P, Badia N, Pérez R, Hernandez Mijares A, Corella D (2011) Homocysteine levels and the metabolic syndrome in a Mediterranean population: a case-control study. Clin Hemorheol Microcirc 47:59–66
Yakub M, Schulze KJ, Khatry SK, Stewart CP, Christian P, West KP Jr (2014) High Plasma Homocysteine increases risk of metabolic syndrome in 6–8 year old children in rural Nepal. Nutrients 6:1649–1661
Jin H, Meyer JM, Mudaliar S, Jeste DV (2008) Impact of atypical antipsychotic therapy on leptin, ghrelin and adiponectin. Schiz Res 100:70–85
Palik E, Birkas KD, Faludi G, Karádi I, Cseh K (2005) Correlation of serum ghrelin levels with body mass index and carbohydrate metabolism in patients treated with atypical antipsychotics. Diabetes Res Clin Pract 68(suppl 1):S60–S64
Perez-Iglesias R, Vazquez-Barquero JL, Amado JA, Berja A, Garcia-Unzueta MT, Pelayo-Terán JM, Carrasco-Marín E, Mata I, Crespo-Facorro B (2008) Effect of antipsychotics on peptides involved in energy balance in drug-naive psychotic patients after 1 year of treatment. J Clin Psychopharmacol 28:289–295
Basoglu C, Oner O, Gunes C, Semiz UB, Ates AM, Algul A, Ebrinc S, Cetin M, Ozcan O, Ipcioglu O (2010) Plasma orexin A, ghrelin, cholecistokinin, visfasin, leptin and agouti-related protein levels during 6-week olanzapine treatment in first-episode male patients with psychosis. Int Clin Psychopharmacol 25:165–171
Richards AA, Hickman IJ, Wang AY, Jones AL, Newell F, Mowry BJ, Whitehead JP, Prins JB, Macdonald GA (2006) Olanzapine treatment is associated with reduced high molecular weight adiponectin in serum: a potential mechanism for olanzapine-induced insulin resistance in patients with schizophrenia. J Clin Psychopharmacol 26:232–237
Sporn AL, Bobb AJ, Gogtay N, Stevens H, Greenstein DK, Clasen LS, Tossell JW, Nugent T, Gochman PA, Sharp WS, Mattai A, Lenane MC, Yanovski JA, Rapoport JL (2005) Hormonal correlates of clozapine-induced weight gain in psychotic children: an exploratory study. J Am Acad Child Adolesc Psychiatry 44:925–933
Maayan LA, Vakhrusheva J (2010) Risperidone associated weight, leptin, and anthropometric changes in children and adolescents with psychotic disorders in early treatment. Human Psychopharmacol 25:133–138
Martin A, Scahill L, Anderson G, Aman M, Arnold LE, McCracken J, McDougle CJ, Tierney E, Chuang S, Vitiello B (2004) Weight and leptin changes among risperidone-treated youths with autism: 6-month prospective data. Am J Psychiatry 161:1125–1127
Calarge CA, Acion L, Kuperman S, Tansey M, Schlechte JA (2009) Weight gain and metabolic abnormalities during extended risperidone treatment in children and adolescents. J Child Adol Psychopharmacol 19:101–109
Merchan-Naranjo J, Tapia C, Bailón C, Moreno C, Baeza I, Calvo-Escalona R, Morer A, Martínez-Cantarero C, Nestares PA, Alda JÁ, Muñoz D, Arango C (2012) Secondary effects of antipsychotic treatment in naïve or quasi-naïve children and adolescents: design of a follow-up protocol and baseline results. Rev Psiquiatr Salud Ment 5:217–228
Andreasen NC, Pressler M, Nopoulos P, Miller D, Ho BC (2010) Antipsychotic dose equivalents and dose-years: a standardized method for comparing exposure to different drugs. Biol Psychiatry 67:255–262
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Sobradillo B, Aguirre A, Aresti U, Bilbao C, Fernández-Ramos A, Lizarraga H, Lorenzo L, Madariaga I, Rica I, Ruiz E, Sánchez C Santamaría, Serrano JM, Zabala A, Zurimendi B, Hernández M (2004) Curvas y tablas de crecimiento: estudios longitudinal y transversal. Fundación Faustino Orbegozo Eizaguirre, Bilbao
Flodmark CE, Lissau I, Moreno LA, Pietrobelli A, Widhalm K (2004) New insights into the field of children and adolescents’ obesity: the European perspective. Int J Obes Relat Metab Disord 28:1189–1196
Arango C, Giráldez M, Merchán-Naranjo J, Baeza I, Castro-Fornieles J, Alda JA, Martínez-Cantarero C, Moreno C, de Andrés P, Cuerda C, de la Serna E, Correll CU, Fraguas D, Parellada M (2014) Second-generation antipsychotic use in children and adolescents; a 6-month prospective cohort study in drug-naïve patients. J Am Acad Child Adol Psychiatry 53:1179–1190
McIntyre RS, Jerrell JM (2008) Metabolic and cardiovascular adverse events associated with antipsychotic treatment in children and adolescents. Arch Pediatr Adolesc Med 162:929–935
Faraone SV, Biederman J, Morley CP, Spencer TJ (2008) Effect of stimulants on height and weight: a review of the literature. J Am Acad Child Adolesc Psychiatry 47:994–1009
Penzner JB, Dudas M, Saito E, Olshanskiy V, Parikh UH, Kapoor S, Chekuri R, Gadaleta D, Avedon J, Sheridan EM, Randell J, Malhotra AK, Kane JM, Correll CU (2009) Lack of effect of stimulant combination with second-generation antipsychotics on weight gain, metabolic changes, prolactin levels, and sedation in youth with clinically relevant aggression or oppositionality. J Child Adolesc Psychopharmacol. 19:563–573
Gentile S (2009) Contributing factors to weight gain during long-term treatment with second-generation antipsychotics. A systematic appraisal and clinical implications. Obes Rev 10:527–542
Gonzaga NC, Medeiros CC, de Carvalho DF, Alves JG (2014) Leptin and cardiometabolic risk factors in obese children and adolescents. J Paediatr Child Health 50:707–712
Poveda E, Callas NE, Baracaldo CM, Castillo C, Hernández P (2007) Leptin levels in school age children associated with antropometric measurements and lipid profiles. Biomedica 27:505–514
Venner AA, Lyon ME, Doyle-Baker PK (2006) Leptin: a potencial biomarker for childhood obesity? Clin. Biochem 39:1047–1056
Karavani G, Strich D, Edri S, Gillis D (2014) Increases in thyrotropin within the near-normal range are associated with increased triiodothyronine but not increased thyroxine in the pediatric age. J Clin Endocrinol Metab 99(8):E1471–5. doi:10.1210/jc.2014-1441 (Epub 2014 May 30)
Marras V, Casini MR, Pilia S, Carta D, Civolani P, Porcu M, Uccheddu AP, Loche S (2010) Thyroid function in obese children and adolescents. Horm Res Paediatr 73:193–197
Margari L, Matera E, Craig F, Petruzzelli MG, Palmieri VO, Pastore A, Margari F (2013) Tolerability and safety profile of risperidone in a sample of children and adolescents. Int Clin Psychopharmacol 28:177–183
Misiak B, Frydecka D, Laczmanski L, Slezak R, Kiejna A (2014) Effects of second-generation antipsychotics on selected markers of one-carbon metabolism and metabolic syndrome components in first-episode schizophrenia patients. Eur J Clin Pharmacol. doi:10.1007/s00228-014-1762-2
Nasrallah HA (2008) Atypical antipsychotic-induced metabolic side effects: insights from receptor-binding profiles. Mol Psychiatry. 13:27–35
Catli G, Anik A, Tuhan HÜ, Kume T, Bober E, Abaci A (2014) The relation of leptin and soluble leptin receptor levels with metabolic and clinical parameters in obese and healthy children. Peptides 56:72–76
Friedemann C, Heneghan C, Mahtani K, Thompson M, Perera R, Ward AM (2012) Cardiovascular disease risk in healthy children and its association with body mass index: systematic review and meta-analysis. BMJ 345:e4759. doi:10.1136/bmj.e4759
Ratzoni G, Gothelf D, Brand-Gothelf A, Reidman J, Kikinzon L, Gal G, Phillip M, Apter A, Weizman R (2002) Weight gain associated with olanzapine and risperidone in adolescent patients: a comparative prospective study. J Am Acad Child Adol Psychiatry 41:337–343
Acknowledgments
We would like to thank the Center for Biomedical Research in the Mental Health Network (CIBERSAM), Madrid (Spain); for partial funding, the following: the Spanish Ministry of Health, Instituto de Salud Carlos III ≪Health Research Fund≫ (F.I.S.-PI04/0455); Madrid Mental Health Association (≪Miguel Angel Martín≫ Research Grant); ≪NARSAD 2005: Independent Investigator Award≫; Alicia Koplowitz and Mutua Madrileña foundations; and the Ministries of Science and Innovation, Community of Madrid, Biomedical R&D funding S2010/BMD-2422 AGES (Madrid) for their support. FP7-HEALTH-F4-2010-241959 (Project PERS—Pediatric European Risperidone Studies). The authors thank Mr. A.D.Pierce for his English editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
IB has received honoraria and travel support from Otsuka and Janssen, research support from Fundación Alicia Koplowitz and grants from the Spanish Ministry of Health, Instituto de Salud Carlos III. RCE has a grant from the Spanish Ministry of Health, Instituto de Salud Carlos III, and has received travel support from Shire. CA is a consultant for AstraZeneca, Bristol Myers Squibb, Janssen-Cilag, Pfizer and Servier; has received grants/support from the Spanish Ministry of Health, Instituto de Salud Carlos III, the European Comission, Fundación Alicia Koplowitz, Astra-Zeneca, Bristol Myers Squibb. JCF has been a consultant for Eli Lilly and has received grants from the Spanish Ministry of Health, Instituto de Salud Carlos III, the European Comission and Fundació La Marató de TV3. LV, ES, JMN and PRL declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Baeza, I., Vigo, L., de la Serna, E. et al. The effects of antipsychotics on weight gain, weight-related hormones and homocysteine in children and adolescents: a 1-year follow-up study. Eur Child Adolesc Psychiatry 26, 35–46 (2017). https://doi.org/10.1007/s00787-016-0866-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-016-0866-x