Abstract
Purpose
The Open Lichtenstein technique, the Laparoscopic Trans-Abdominal PrePeritoneal (TAPP), the Totally Extra Peritoneal (TEP), and the robotic TAPP (rTAPP) are commonly performed. The aim of the present network meta-analysis was to globally compare short-term outcomes within these major surgical techniques for primary unilateral inguinal hernia repair.
Methods
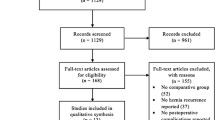
PubMed, EMBASE, and Web of Science were consulted. A fully Bayesian network meta-analysis was performed.
Results
Sixteen studies (51.037 patients) were included. Overall, 35.5% underwent Open, 33.5% TAPP, 30.7% TEP, and 0.3% rTAPP. The postoperative seroma risk ratio (RR) was comparable considering TAPP vs. Open (RR 0.91; 95% CrI 0.50–1.62), TEP vs. Open (RR 0.64; 95% CrI 0.32–1.33), TEP vs. TAPP (RR 0.70; 95% CrI 0.39–1.31), and rTAPP vs. Open (RR 0.98; 95% CrI 0.37–2.51). The postoperative chronic pain RR was similar for TAPP vs. Open (RR 0.53; 95% CrI 0.27–1.20), TEP vs. Open (RR 0.86; 95% CrI 0.48–1.16), and TEP vs. TAPP (RR 1.70; 95% CrI 0.63–3.20). The recurrence RR was comparable when comparing TAPP vs. Open (RR 0.96; 95% CrI 0.57–1.51), TEP vs. Open (RR 1.0; 95% CrI 0.65–1.61), TEP vs. TAPP (RR 1.10; 95% CrI 0.63–2.10), and rTAPP vs. Open (RR 0.98; 95% CrI 0.45–2.10). No differences were found in term of postoperative hematoma, surgical site infection, urinary retention, and hospital length of stay.
Conclusions
This study suggests that Open, TAPP, TEP, and rTAPP seem comparable in the short term. The surgical management of inguinal hernia is evolving and the effect of the adoption of innovative minimally invasive techniques should be further investigated in the long term. Ultimately, the choice of the most suitable treatment should be based on individual surgeon expertise and tailored on each patient.




Similar content being viewed by others
References
The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22(1):1–165. https://doi.org/10.1007/s10029-017-1668-x
Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362(9395):1561–1571
Wu JJ, Way JA, Eslick GD, Cox MR (2018) Transabdominal pre-peritoneal versus open repair for primary unilateral inguinal hernia: a meta-analysis. World J Surg 5:1304–1311. https://doi.org/10.1007/s00268-017-4288-9
National Institute for Health and Care Excellence (2016) NICE technology appraisal guidance no. 83: laparoscopic surgery for inguinal hernia repair. https://www.nice.org.uk/guidance/ta83. Accessed 9 May 2019
Waite KE, Herman MA, Doyle PJ (2016) Comparison of robotic versus laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair. J Robot Surg 10:239–244. https://doi.org/10.1007/s11701-016-0580-1
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
Higgins JP, Altman DG, Gotzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Sterne JA, Hernan MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 4919:i355
Mills EJ, Thorlund K, Ioannidis JPA (2013) Demystifying trial networks and network meta-analysis. BMJ 346:f2914–f2914
Aiolfi A, Tornese S, Bonitta G, Rausa E, Micheletto G, Bona D (2019) Roux-En-Y gastric bypass: systematic review and Bayesian network meta-analysis comparing open, laparoscopic, and robotic approach. Surg Obes Relat Dis. https://doi.org/10.1016/j.soard.2019.03.006 (In press)
Warn DE, Thompson SG, Spiegelhalter DJ (2002) Bayesian random effects meta-analysis of trials with binary outcomes: methods for the absolute risk difference and relative risk scales. Stat Med 21(11):1601–1623
Friede T, Röver C, Wandel S, Neuenschwander B (2017) Meta-analysis of few small studies in orphan diseases. Res Synth Methods 8(1):79–91
Turner RM, Davey J, Clarke MJ, Thompson SG, Higgins JP (2012) Predicting the extent of heterogeneity in meta-analysis, using empirical data from the Cochrane database of systematic reviews. Int J Epidemiol 41(3):818–827
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Smith BJ (2007) boa: an R package for MCMC output convergence assessment and posterior inference. J Stat Softw 21:1–37. https://doi.org/10.18637/jss.v021.i11
Dias S, Welton NJ, Caldwell DM, Ades AE (2010) Checking consistency in mixed treatment comparison meta-analysis. Stat Med 29(7–8):932–944
Salanti G, Del Giovane C, Chaimani A, Caldwell DM, Higgins JPT (2014) Evaluating the quality of evidence from a network meta-analysis. PLoS One 9(7):e99682
Higgins JPT, Green S (2011) The Cochrane Collaboration. Cochrane handbook for systemic reviews of interventions, version 5.1.0. The Cochrane Collaboration, Australia. https://training.cochrane.org/handbook. Accessed 9 May 2019
Plummer M (2003) JAGS: a program for analysis of Bayesian graphical models using Gibbs sampling. In: Proceedings of the 3rd international workshop on distributed statistical computing, Vienna, Austria, 20–22 March 2003
R Core Team (2019) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Iraniha A, Peloquin J (2018) Long-term quality of life and outcomes following robotic assisted TAPP inguinal hernia repair. J Robot Surg 12:261–269. https://doi.org/10.1007/s11701-017-0727-8
Anadol ZA, Ersoy E, Taneri F, Tekin E (2004) Outcome and cost comparison of laparoscopic transabdominal preperitoneal hernia repair versus Open Lichtenstein technique. J Laparoendosc Adv Surg Tech A 14(3):159–163
Lau H, Patil NG, Yuen W (2006) Day-case endoscopic totally extraperitoneal inguinal hernioplasty versus open Lichtenstein hernioplasty for unilateral primary inguinal hernia in males: a randomized trial. Surg Endosc 1:76–81
Butters M, Redecke J, Köninger J (2007) Long-term results of a randomized clinical trial of Shouldice, Lichtenstein and transabdominal preperitoneal hernia repairs. Br J Surg 94:562–565
Pokorny H, Klingler A, Schmid T, Fortelny R, Hollinsky C, Kawji R, Steiner E, Pernthaler H, Függer R, Scheyer M (2008) Recurrence and complications after laparoscopic versus open inguinal hernia repair: results of a prospective randomized multicenter trial. Hernia 12:385–389. https://doi.org/10.1007/s10029-008-0357-1
Eklund AS, Montgomery AK, Rasmussen IC, Sandbue RP, Bergkvist LA, Rudberg CR (2009) Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair: a randomized, multicenter trial with 5-year follow-up. Ann Surg 249:33–38. https://doi.org/10.1097/SLA.0b013e31819255d0
Hamza Y, Gabr E, Hammadi H, Khalil R (2010) Four-arm randomized trial comparing laparoscopic and open hernia repairs. Int J Surg 8:25–28. https://doi.org/10.1016/j.ijsu.2009.09.010
Gong K, Zhang N, Lu Y, Zhu B, Zhang Z, Du D, Zhao X, Jiang H (2011) Comparison of the open tension-free mesh-plug, transabdominal preperitoneal (TAPP), and totally extraperitoneal (TEP) laparoscopic techniques for primary unilateral inguinal hernia repair: a prospective randomized controlled trial. Surg Endosc 1:234–239. https://doi.org/10.1007/s00464-010-1165-0
Abbas AE, Abd Ellatif ME, Noaman N, Negm A, El-Morsy G, Amin M, Moatamed A (2012) Patient-perspective quality of life after laparoscopic and open hernia repair: a controlled randomized trial. Surg Endosc 26:2465–2470. https://doi.org/10.1007/s00464-012-2212-9
Dhankhar DS, Sharma N, Mishra T, Kaur N, Singh S, Gupta S (2014) Totally extraperitoneal repair under general anesthesia versus Lichtenstein repair under local anesthesia for unilateral inguinal hernia: a prospective randomized controlled trial. Surg Endosc 28:996–1002. https://doi.org/10.1007/s00464-013-3269-9
Wang WJ, Chen JZ, Fang Q, Li JF, Jin PF, Li ZT (2013) Comparison of the effects of laparoscopic hernia repair and Lichtenstein tension-free hernia repair. J Laparoendosc Adv Surg Tech A 23:301–305. https://doi.org/10.1089/lap.2012.0217
Dahlstrand U, Sandblom G, Ljungdahl M, Wollert S, Gunnarsson U (2013) TEP under general anesthesia is superior to Lichtenstein under local anesthesia in terms of pain 6 weeks after surgery: results from a randomized clinical trial. Surg Endosc 27:3632–3638. https://doi.org/10.1007/s00464-013-2936-1
Aigner F, Augustin F, Kaufmann C, Schlager A, Ulmer H, Pratschke J, Schmid T (2014) Prospective, randomized-controlled trial comparing postoperative pain after plug and patch open repair with totally extraperitoneal inguinal hernia repair. Hernia 18:237–242. https://doi.org/10.1007/s10029-013-1123-6
Pedroso LM, DE-Melo RM, DA-Silva NJ (2017) Comparative study of postoperative pain between the Lichtenstein and laparoscopy surgical techniques for the treatment of unilateral primary inguinal hernia. Arq Bras Cir Dig 30:173–176. https://doi.org/10.1590/0102-6720201700030003
Charles EJ, Mehaffey JH, Tache-Leon CA, Hallowell PT, Sawyer RG, Yang Z (2018) Inguinal hernia repair: is there a benefit to using the robot? Surg Endosc 32:2131–2136. https://doi.org/10.1007/s00464-017-5911-4
Muysoms F, Van Cleven S, Kyle-Leinhase I, Ballecer C, Ramaswamy A (2018) Robotic-assisted laparoscopic groin hernia repair: observational case–control study on the operative time during the learning curve. Surg Endosc 32:4850–4859. https://doi.org/10.1007/s00464-018-6236-7
Köckerling F, Bittner R, Kofler M, Mayer F, Adolf D, Kuthe A, Weyhe D (2019) Lichtenstein versus total extraperitoneal patch plasty versus transabdominal patch plasty technique for primary unilateral inguinal hernia repair: a registry-based, propensity score-matched comparison of 57,906 patients. Ann Surg 269:351–357. https://doi.org/10.1097/SLA.0000000000002541
Campanelli G, Bruni PG, Morlacchi A, Lombardo F, Cavalli M (2017) Primary inguinal hernia: the open repair today pros and cons. Asian J Endosc Surg 10:236–243. https://doi.org/10.1111/ases.12394
Colvin HS, Rao A, Cavalli M, Campanelli G, Amin AI (2013) (2013) Glue versus suture fixation of mesh during open repair of inguinal hernias: a systematic review and meta-analysis. World J Surg 37:2282–2292. https://doi.org/10.1007/s00268-013-2140-4
Wagner JP, Schroeder AD, Espinoza JC, Hiatt JR, Mellinger JD, Cusick RA, Fitzgibbons RJ, Campanelli G, Cavalli M, Roll S, Silva RA, Reinpold W, Télémaque LF, Matthews BD, Filipi CJ, Chen DC (2017) Global outreach using a systematic, competency-based training paradigm for inguinal hernioplasty. JAMA Surg 152:66–73. https://doi.org/10.1001/jamasurg.2016.3323
Rausa E, Asti E, Kelly ME, Aiolfi A, Lovece A, Bonitta G, Bonavina L (2019) Open inguinal hernia repair: a network meta-analysis comparing self-gripping mesh, suture fixation, and glue fixation. World J Surg 2019(43):447–456. https://doi.org/10.1007/s00268-018-4807-3
Scheuermann U, Niebisch S, Lyros O, Jansen-Winkeln B, Gockel I (2017) Transabdominal preperitoneal (TAPP) versus Lichtenstein operation for primary inguinal hernia repair—a systematic review and meta-analysis of randomized controlled trials. BMC Surg 17(1):55. https://doi.org/10.1186/s12893-017-0253-7
Mui WL, Ng CS, Fung TM, Cheung FK, Wong CM, Ma TH, Bn MY, Ng EK (2006) Prophylactic ilioinguinal neurectomy in open inguinal hernia repair: a double-blind randomized controlled trial. Ann Surg 244(1):27–33
Hsu W, Chen CS, Lee HC, Liang HH, Kuo LJ, Wei PL, Tam KW (2012) Preservation versus division of ilioinguinal nerve on open mesh repair of inguinal hernia: a meta-analysis of randomized controlled trials. World J Surgs 36:2311–2319. https://doi.org/10.1007/s00268-012-1657-2
Charalambous MP, Charalambous CP (2018) Incidence of chronic groin pain following open mesh inguinal hernia repair, and effect of elective division of the ilioinguinal nerve: meta-analysis of randomized controlled trials. Hernia 22:401–409. https://doi.org/10.1007/s10029-018-1753-9
Junge K, Rosch R, Klinge U, Schwab R, Peiper Ch, Binnebösel M, Schenten F, Schumpelick V (2006) Risk factors related to recurrence in inguinal hernia repair: a retrospective analysis. Hernia 10(4):309–315
Schjøth-Iversen L, Refsum A, Brudvik KW (2017) Factors associated with hernia recurrence after laparoscopic total extraperitoneal repair for inguinal hernia: a 2-year prospective cohort study. Hernia 21:729–735. https://doi.org/10.1007/s10029-017-1634-7
Escobar Dominguez JE, Ramos MG, Seetharamaiah R, Donkor C, Rabaza J, Gonzalez A (2016) Feasibility of robotic inguinal hernia repair, a single-institution experience. Surg Endosc 9:4042–4048. https://doi.org/10.1007/s00464-015-4717-5
Tam V, Rogers DE, Al-Abbas A, Borrebach J, Dunn SA, Zureikat AH, Zeh HJ 3rd, Hogg ME (2019) Robotic inguinal hernia repair: a large health system’s experience with the first 300 cases and review of the literature. J Surg Res 235:98–104. https://doi.org/10.1016/j.jss.2018.09.070
Henriksen NA, Jensen KK, Muysoms F (2019) Robot-assisted abdominal wall surgery: a systematic review of the literature and meta-analysis. Hernia 23:17–27. https://doi.org/10.1007/s10029-018-1872-3
Shrier I, Boivin JF, Steele RJ (2007) Should meta-analyses of interventions include observational studies in addition to randomized controlled trials? A critical examination of underlying principles. Am J Epidemiol 166:1203–1209
McCulloch P, Taylor I, Sasako M (2002) Randomised trials in surgery: problems and possible solutions. BMJ 324(7351):1448–1451
Funding
None.
Author information
Authors and Affiliations
Contributions
AA, FL, AM, and GC did the literature search; AA, FL, and GC formed the study design; Data collection was done by AA, FL, MC, and AM. AA, GB, and DB analysed the data; AA, GM, and DB interpreted the data; AA, GB, and DB wrote the manuscript; AA, DB, and GC critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
AA, MC, GM, FL, GB, AM, PGB, GC, and Db declare no conflicts of interest.
Ethical approval
Approval from the Institutional review board was not required for this study.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this systematic review and meta-analysis, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The article is part of the Topical Collection “Forum on primary monolateral uncomplicated inguinal hernia”.
Rights and permissions
About this article
Cite this article
Aiolfi, A., Cavalli, M., Micheletto, G. et al. Primary inguinal hernia: systematic review and Bayesian network meta-analysis comparing open, laparoscopic transabdominal preperitoneal, totally extraperitoneal, and robotic preperitoneal repair. Hernia 23, 473–484 (2019). https://doi.org/10.1007/s10029-019-01964-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-019-01964-2