Abstract
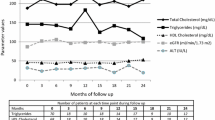
We analysed the efficacy and safety of switching from a regimen based on nonnucleoside reverse transcriptase inhibitors (NNRTI) or integrase inhibitors (INI) to ABC/3TC + RPV in virologically suppressed HIV-infected patients. This multicentre, retrospective study comprised asymptomatic HIV-infected patients who switched from 2 NRTI + NNRTI or 2 NRTI + INI to ABC/3TC + RPV between February 2013 and December 2013; all had undetectable HIV viral load prior to switching. Efficacy and safety, and changes in lipids and cardiovascular risk (CVR) were analysed at 48 weeks. Of 85 patients (74.1 % men, mean age 49.5 years), 83 (97.6 %) switched from a regimen based on NNRTI (EFV 74, RPV 5, ETV 2, NVP 2), and 45 (53 %) switched from TDF/FTC to ABC/3TC. The main reasons for switching were toxicity (58.8 %) and convenience (29.4 %). At 48 weeks, 78 (91.8 %) patients continued taking the same regimen; efficacy was 88 % by intention to treat, and 96 % by per protocol. Two patients were lost to follow-up and five ceased the new regimen (4 due to adverse effects and 1 virologic failure). Mean CD4 cell counts increased (744 vs. 885 cells/μL; p = 0.0001), and there were mean decreases in fasting total cholesterol (–15.9 mg/dL; p < 0.0001) and LDL-cholesterol (–11.0 mg/dL; p < 0.004), with no changes in HDL-cholesterol, triglycerides, total cholesterol:HDL-cholesterol ratio, and CVR. ABC/3TC + RPV is effective and safe in virologically-suppressed patients on antiretroviral therapy (ART). Forty-eight weeks after switching the lipid profile improved with decreases in total and LDL cholesterol.
Similar content being viewed by others
Introduction
Switching antiretroviral therapy in stable, virologically suppressed patients with the aim of improving tolerability and convenience is an expanding strategy in clinical practice [1]. Rilpivirine (RPV), a second-generation nonnucleoside reverse-transcriptase inhibitor (NNRTI), is active against wild-type viruses and remains efficient against some NNRTI-resistant HIV strains [2]. RPV and its coformulation with emtricitabine (FTC) and tenofovir disoproxil fumarate (TDF) as a single-tablet regimen ([STR] RPV/FTC/TDF) is a good option for simplification strategies [3]. Significant improvements in clinical and analytical adverse events have been observed in virologically suppressed HIV-infected patients switching to RPV/FTC/TDF from a ritonavir-boosted protease inhibitor (PI/r) and NNRTI based regimens [4–6]. However, few data on RPV plus abacavir/lamivudine (ABC/3TC) are available, all of them concerning naïve patients [3].
The objective of this study was to analyse, in a real-world setting, the efficacy and safety of switching from a regimen based on NNRTI or integrase inhibitors (INI) to ABC/3TC plus RPV in virologically suppressed HIV-infected patients.
Methods
A cohort of 7,270 HIV-infected patients was followed prospectively in five hospitals from Andalusia, southern Spain. In this open-label, multicentre, non-controlled study, we retrospectively analysed the asymptomatic patients from this cohort who switched from a regimen based on two nucleoside reverse transcriptase inhibitors (NRTI) plus a NNRTI or INI to ABC/3TC plus RPV from February 2013 to December 2013. All the patients had to have had an undetectable (<50 copies/mL) viral load (VL) for at least the last 3 months prior to switching. Patients with previous failures on ART including ABC and/or 3TC, or with genotype tests showing resistance to ABC, 3TC or RPV were excluded. We assessed the percentage of patients with an undetectable VL and the CD4 responses with the new regimen at 48 weeks, and the percentage of patients who ceased ABC/3TC plus RPV due to adverse events. Changes were analysed in the lipid profile, including total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglycerides (TG), and the TC to HDL-C ratio, and in the cardiovascular risk (CVR) assessed by the Framingham equation, between baseline and 48 weeks after switching.
Institutional review board/ethics committee approval was obtained for the study protocol for the analysis of anonymous routine clinical data of patients. The study was sponsored by the Sociedad Andaluza de Enfermedades Infecciosas (SAEI) and registered as the SAEI 00/0067 study.
Data for each patient were included in a database for statistical analysis. A descriptive analysis of the variables was done with point estimation and 95 % confidence interval. Continuous variables are shown as the mean and standard deviation or the median, depending on the distribution. Categorical variables are shown as frequencies or percentages. Comparison of continuous data between baseline and 48 weeks was done with the Student t test for paired samples. The statistical program used was SPSS version 17.0 (SPSS, Chicago, IL, USA).
Results
Of the initial 97 patients recruited 12 were excluded as they did not fulfil the inclusion criteria (3 were naïve, 7 had already been treated with IP/r, 1 with three NTRI, and 1 with a regimen that included maraviroc), giving a final study sample of 85 cases. The median age was 47.4 (42.5–53.7) years, and 74.1 % were male. Most of the patients switched from a regimen based on NNRTI (97.6 %), mainly efavirenz (EFV). The main reason for switching was the presence of adverse events. The clinical characteristics of the patients at the time of switching are shown in Table 1.
At 48 weeks after switching to ABC/3TC plus RPV, 78 (91.8 %) patients were still taking the same regimen, with an increase in CD4 count (855 vs. 718 cells/μL); efficacy was 88 % by intention to treat (75 out of 85 with <50 copies/ml at 48 weeks), and 96 % by per protocol. Two of the other seven patients were lost to follow-up, and 5 (5.9 %) ceased the new regimen; there were four due to adverse events (2 digestive intolerance, 1 nephrotoxicity and 1 arthralgias) and one due to virologic failure with emergence of the E138K mutation. In addition to this last case, there were two patients with 64 cop/mL and 61 cop/mL at 48 weeks, which were considered blips. The mean levels of fasting TC and LDL-C fell at 24 and 48 weeks, with no changes detected in TG, HDL-C, TC to HDL-C ratio or CVR; lipid profile did not change in patients who switched from TDF (Table 2). The mean level of creatinine increased at 48 weeks (0.93 vs 0.97 mg/dL; p = 0.02), but it did not reach statistical significance when analysed depending on previous TDF or ABC use (0.95 vs 0.99 mg/dL; p = 0.1, and 0.91 vs 0.95 mg/dL; p = 0.08, respectively). All patients who switched from EFV improved CNS adverse events.
Discussion
This study shows that stable suppressed patients who switch from a regimen of NRTI plus first-generation NNRTI or INI to ABC/3TC + RPV maintained good immuno-virologic control at 48 weeks and showed an improvement in their lipid profile. RPV has proven to have a better lipid profile compared with EFV in naïve patients [7]. Although more than half of the patients changed from the fixed dose TDF/FTC to ABC/3TC, we observed an improvement in lipid components, with decreases in TC and LDL-C. TDF has a better lipid profile than ABC. Although previous switch studies from ABC/3TC to TDF/FTC also show improvements in the lipid profile, the third antiretroviral is maintained in all these studies [8–10]. Here with the benefit seen in the lipid profile in our study, attributable mainly to RPV. Only five patients discontinued ABC/3TC plus RPV, four due to adverse events and one due to virologic failure. Although after discontinuation, EFV has an extended inductive effect on cytochrome P450 (CYP) 3A4 that, after switching, may reduce RPV exposure, this strategy was safe, as has been previously reported [6]. The main advantage of this scheme is the avoidance of TDF. Large meta-analyses have demonstrated a significantly greater loss of renal function in those on TDF compared to non-TDF-containing regimens [11] and TDF-induced tubular dysfunction in patients randomly assigned to either a TDF- or ABC-containing regimen [12]. Moreover, TDF is associated with increased bone toxicity [13]. In the randomized ASSERT study, patients on TDF experienced a significantly greater decline in hip bone mineral density compared to those in the ABC arm [14]. On the other hand, RPV has an excellent tolerance, without the central nervous system effects of EFV, and with few adverse events leading to suspension.
This study has certain limitations. First, the absence of a control group prevents us determining the evolution of the lipid profile and the effectiveness and safety in patients who would have continued with the prior regimen. The second limitation concerns the retrospective design of the study, and perhaps the small number of patients included.
In summary, at 48 weeks after switching from a regimen based on NRTI plus NNRTI or INI to ABC/3TC plus RPV, good immuno-virologic control was maintained and the lipid profile improved. This strategy therefore seems convenient for many HIV-infected patients.
References
Van den Eynde E, Podzamczer D (2014) Switch strategies in antiretroviral therapy regimens. Expert Rev Anti Infect Ther 12:1055–1074
James C, Preininger L, Sweet M (2012) Rilpivirine: a second-generation nonnucleoside reverse transcriptase inhibitor. Am J Health Syst Pharm 69:857–861
Casado JL, Moreno S (2013) Potential role of rilpivirine in simplification regimens. Enferm Infec Microbiol Clin Suppl 2:30–35
Palella FJ, Fisher M, Tebas P, Gazzard B, Ruane P, Van Lunzen J et al (2014) Simplification to rilpivirine/emtricitabine/tenofovir disoproxil fumarate from ritonavir-boosted protease inhibitor antiretroviral therapy in a randomized trial of HIV-1 RNA-suppressed participants. AIDS 28:335–344
Allavena C, Dailly E, Reliquet V, Bonnet B, Pineau S, André-Garnier E et al (2014) Switching from tenofovir/emtricitabine and nevirapine to a tenofovir/emtricitabine/rilpivirine single-tablet regimen in virologically suppressed, HIV-1-infected subjects. J Antimicrob Chemother 69:2004–2008
Mills AM, Cohen C, Dejesus E et al (2013) Efficacy and safety 48 weeks after switching from efavirenz to rilpivirine using emtricitabine/tenofovir disoproxil fumarate-based single-tablet regimens. HIV Clin Trials 14:216–223
Tebas P, Sension M, Arribas J, Duiculescu D, Florence E, Hung CC, on behalf of the ECHO and THRIVE Studies et al (2014) Lipid levels and changes in body fat distribution in treatment-naive, HIV-1–infected adults treated with rilpivirine or efavirenz for 96 weeks in the ECHO and THRIVE Trials. Clin Infect Dis 59:425–434
Martínez E, Arranz JA, Podzamczer D, Loncá M, Sanz J, Barragán P, on behalf of BICOMBO Study Team et al (2009) A simplification trial switching from nucleoside reverse transcriptase inhibitors to once-daily fixed-dose abacavir/lamivudine or tenofovir/emtricitabine in HIV-1-infected patients with virological suppression. J Acquir Immune Defic Syndr 51:290–297
Campo R, DeJesus E, Bredeek UF, Henry K, Khanlou H, Logue K et al (2013) SWIFT: prospective 48-week study to evaluate efficacy and safety of switching to emtricitabine/tenofovir from lamivudine/abacavir in virologically suppressed HIV-1 infected patients on a boosted protease inhibitor containing antiretroviral régimen. Clin Infect Dis 56:1637–1645
Martin A, Bloch M, Amin J, Baker D, Cooper DA, Emery S et al (2009) Simplification of antiretroviral therapy with tenofovir-emtricitabine or abacavir-lamivudine: a randomized, 96-week trial. Clin Infect Dis 49:1591–1601
Cooper RD, Wiebe N, Smith N, Keiser P, Naicker S, Tonelli M (2010) Systematic review and meta-analysis: renal safety of tenofovir disoproxil fumarate in HIV-infected patients. Clin Infect Dis 51:496–505
Maggi P, Montinaro V, Bellacosa C, Pietanza S, Volpe A, Graziano G et al (2012) Early markers of tubular dysfunction in antiretroviral-experienced HIV-infected patients treated with tenofovir versus abacavir. AIDS Patient Care STDS 26:5–11
Bedimo R, Maalouf NM, Zhang S, Drechsler H, Tebas P (2012) Osteoporotic fracture risk associated with cumulative exposure to tenofovir and other antiretroviral agents. AIDS 26:825–831
Moyle GJ, Stellbrink HJ, Compston J, Orkin C, Arribas JR, Domingo P, on behalf of ASSERT Team et al (2013) 96-Week results of abacavir/lamivudine versus tenofovir/emtricitabine, plus efavirenz, in antiretroviral-naive, HIV-1-infected adults: ASSERT study. Antivir Ther 18:905–913
Acknowledgments
The authors would like to thank the study participants as well as the investigators. The authors also thank Ian Johnstone for help with the English language version of the text and the Sociedad Andaluza de Enfermedades Infecciosas for its support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study has been supported in part by the RD12/0017/0017 project (Plan Nacional R + D + I) and cofinanced by Instituto de Salud Carlos III-Subdirección General de Evaluación y el Fondo Europeo de Desarrollo Regional and a grant from by Janssen Cilag.
Conflict of interest
R.P., M.O., J.O., J.H.Q. and J.S. are on the scientific advisory board and speakers’ bureau for Janssen Cilag and have received grants and travel expenses for conferences from Janssen Cilag.
I.A.P.H., M.A.M., M.L.M., C.M.G.D., A.R., J.M.R. and I.P.C. have no personal disclosures.
Ethical approval
Institutional review board/ethics committee approval was obtained for the study protocol for the analysis of anonymous routine clinical data of patients.
Informed consent
Patients were informed about the nature of the study and accepted to be included.
Members of the SAEI 00/0067 study group
R. Palacios, I.A. Pérez-Hernández, C.M. González-Doménech, J. Ruiz, E. Nuño, M. Márquez, J. Santos (Hospital Clínico Universitario Vírgen de la Victoria, Málaga), M.I. Mayorga, M. Castaño (Hospital Regional Universitario Carlos Haya, Málaga), M.A. Martínez, D. Vinuesa, J. Hernández-Quero (Hospital Universitario San Cecilio, Granada), M. Omar (Hospital Universitario Ciudad de Jaén, Jaén), A. Romero (Hospital Universitario de Puerto Real, Cádiz), J.A. Romero, M.C. Gálvez (Hospital de Torrecárdenas, Almería) I. Pérez-Camacho (Hospital de Poniente, Almería), A. del Arco, J. de la Torre, J. Olalla, J.L. Prada (Hospital Costa del Sol, Marbella).
This study was partially presented at the HIV Drug Therapy Congress, Glasgow 2014.
Rights and permissions
About this article
Cite this article
Palacios, R., Pérez-Hernández, I.A., Martínez, M.A. et al. Efficacy and safety of switching to abacavir/lamivudine (ABC/3TC) plus rilpivirine (RPV) in virologically suppressed HIV-infected patients on HAART. Eur J Clin Microbiol Infect Dis 35, 815–819 (2016). https://doi.org/10.1007/s10096-016-2602-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2602-3