Abstract
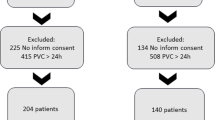
A high percentage of venous lines (VLs) are placed in non-ICU patients, particularly those treated in the internal medicine department (IMD). We assessed adherence to VL care after a training program aimed at nurses and clinicians attending patients admitted to Spanish IMDs. We performed a multicenter prospective observational point prevalence study in 14 Spanish IMDs in 2013 and 2016. We included all adult patients (> 18 years) admitted to IMDs on the study day and reviewed nursing records for patients with VL in place before and after a 1-year training program during 2015. Answers from an interview with head nurses of the IMDs regarding commonly used practices in the daily management of VLs were also compared. A total of 638 and 693 patients were seen during each period, respectively, and 530 and 598 patients had ≥ 1 VL implanted (83.1 vs. 86.3%). Catheters were considered unnecessary in 12.8 and 15.0% of cases (p = 0.28). Daily recording of the need for catheter use increased from 43.8 to 71.8% (p < 0.001). Furthermore, daily monitoring of the insertion site remained very frequent (94.4 vs. 92.2%; p = 0.16). The date of insertion was recorded in 86.3 and 85.5% of cases (p = 0.73), and no combination of closed connectors with open caps increased from 74.8 to 90.3% (p < 0.001). Overall, head nurses’ knowledge improved in 4 out of 14 recommendations assessed (28.6%). A simple and easy program for training on management of VLs in Spanish IMDs was associated with improved quality of care.
Similar content being viewed by others
References
Pittet D, Tarara D, Wenzel RP (1994) Nosocomial bloodstream infection in critically ill patients: excess length of stay, extra costs, and attributable mortality. JAMA 271(20):1598–1601
Blot SI, Depuydt P, Annemans L et al (2005) Clinical and economic outcomes in critically ill patients with nosocomial catheter-related bloodstream infections. Clin Infect Dis 41(11):1591–1598
Barsanti MC, Woeltje KF (2009) Infection prevention in the intensive care unit. Infect Dis Clin N Am 23(3):703–725
Chatzinikolaou I, Raad II (2000) Intravascular catheter-related infections: a preventable challenge in the critically ill. Semin Respir Infect 15(4):264–271
Chittick P, Sherertz RJ (2010) Recognition and prevention of nosocomial vascular device and related bloodstream infections in the intensive care unit. Crit Care Med 38(8 Suppl):S363–S372
Coopersmith CM, Zack JE, Ward MR et al (2004) The impact of bedside behavior on catheter-related bacteremia in the intensive care unit. Arch Surg 139(2):131–136
Pronovost P, Needham D, Berenholtz S et al (2006) An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 355(26):2725–2732
Guembe M, Perez-Parra A, Gomez E et al (2012) Impact on knowledge and practice of an intervention to control catheter infection in the ICU. Eur J Clin Microbiol Infect Dis 31(10):2799–2808
Perez Parra A, Cruz Menarguez M, Perez Granda MJ, Tomey MJ, Padilla B, Bouza E (2010) A simple educational intervention to decrease incidence of central line-associated bloodstream infection (CLABSI) in intensive care units with low baseline incidence of CLABSI. Infect Control Hosp Epidemiol 31(9):964–967
Palomar M, Alvarez-Lerma F, Riera A et al (2013) Impact of a national multimodal intervention to prevent catheter-related bloodstream infection in the ICU: the Spanish experience. Crit Care Med 41(10):2364–2372
Freixas N, Bella F, Limon E, Pujol M, Almirante B, Gudiol F (2013) Impact of a multimodal intervention to reduce bloodstream infections related to vascular catheters in non-ICU wards: a multicentre study. Clin Microbiol Infect 19(9):838–844
Kallen AJ, Patel PR, O’Grady NP (2010) Preventing catheter-related bloodstream infections outside the intensive care unit: expanding prevention to new settings. Clin Infect Dis 51(3):335–341
Guembe M, Perez-Granda MJ, Capdevila JA et al (2015) Nationwide study on the use of intravascular catheters in internal medicine departments. J Hosp Infect 90(2):135–141
O’Grady NP, Alexander M, Burns LA et al (2011) Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis 52(9):e162–e193
Bassetti M, Molinari MP, Mussap M, Viscoli C, Righi E (2013) Candidaemia in internal medicine departments: the burden of a rising problem. Clin Microbiol Infect 19(6):E281–E284
Garcia-Rodriguez JF, Alvarez-Diaz H, Vilarino-Maneiro L et al (2013) Epidemiology and impact of a multifaceted approach in controlling central venous catheter associated blood stream infections outside the intensive care unit. BMC Infect Dis 13:445
Guembe M, Pérez-Granda MJ, Capdevila JA et al (2017) Nationwide study on peripheral venous catheter-related bloodstream infections in internal medicine departments. Poster Eur Congr Clin Microbiol and Infect Dis 2017:22–25 Vienna
Capdevila JA, Guembe M, Barberan J et al (2016) Expert consensus document on prevention, diagnosis and treatment of short-term peripheral venous catheter-related infections in adult. Rev Esp Quimioter 29(4):230–238
Labeau SO, Vandijck DM, Rello J et al (2009) Centers for Disease Control and Prevention guidelines for preventing central venous catheter-related infection: results of a knowledge test among 3405 European intensive care nurses. Crit Care Med 37(1):320–323
Acknowledgements
We thank Thomas O’Boyle for his help in the preparation of the manuscript.
We thank the members of the NUVE study group for their contribution to the study:
Hospital General Universitario Gregorio Marañón (Madrid): Jesús Millán, Carlos Pérez de Oteyza, Antonio Muiño, Mariví Villalba, Carmen Cuenca, Jesús García Castaño, Cecilia Muñoz Delgado, Sonia Zamorano, Beatriz Gómez, and José Manuel Collado.
Hospital L’Esperit Sant (Cataluña): Miguel Torres Salinas, Alex Smithson Amat, and Javier Ramos Lázaro.
Hospital de Santa Bárbara (Castilla La Mancha): Valentín del Villar Sordo and Mario del Valle Sánchez.
Hospital de Mataró (Cataluña): Ángela Felip Benach, Elena Vidal, and Laia Albiach.
Hospital de Txagorritxu (País Vasco): José Manuel Agud Aparicio and Esther Saéz de Adana Arroniz.
Hospital Santa Creu i Sant Pau (Cataluña): Jordi Casademont i Pou and Virginia Pomar Solchaga.
Hospital Reina Sofía (Navarra): Fernando Escolar Castellón and Teresa Rubio Obanos.
Hospital Universitario de Cruces (País Vasco): Maria Victoria Egurbide Arberas, Javier Nieto Arana and Eduardo García López.
Hospital Universitario Sant Joan de Reus (Cataluña): Antonio Castro Salomó and Simona Micaela Iftimie.
Hospital General La Mancha Centro (Castilla La Mancha): Antonio Martín Castillo and José Ramón Barberá Farré.
Hospital de Tortosa Verge de la Cinta (Cataluña): Amat Ortí Lavería, Mercé Cardona Ribera and Naya Bellaubí Pallarés.
Hospital Santos Reyes (Burgos): Pedro Cancelo Suárez, Francisco Javier Cepeda Piorno, Noelia Arenal Andrés and Raquel Elisa Rodríguez Tarazona.
Hospital Universitario de Guadalajara (Castilla La Mancha): Manuel Miguel Rodríguez Zapata and María Asunción Costa Cerdá.
Hospital Comarcal de Valdeorras (Galicia): José Felipe Morales Martín and Josep Masferrer Serra.
Hospital Universitario de Bellvitge (Cataluña): Xavier Corbella, Miquel Pujol, Eunice Pere and Ana Hornero.
Funding
M. Guembe is supported by the Miguel Servet Program (ISCIII-MICINN, CP13/00268) from the Health Research Fund (FIS) of the Carlos III Health Institute (ISCIII), Madrid, Spain. The study was partially funded by the European Regional Development Fund (FEDER) “A way of making Europe” (PI14/01933) and Fundación Española de Medicina Interna (FEMI).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee of Hospital Gregorio Marañón.
Informed consent
The Ethics Committee of Hospital Gregorio Marañón required written informed consent to be obtained from the patients included in the study.
Rights and permissions
About this article
Cite this article
Guembe, M., Pérez-Granda, M.J., Capdevila, J.A. et al. Impact of a training program on adherence to recommendations for care of venous lines in internal medicine departments in Spain. Eur J Clin Microbiol Infect Dis 37, 1163–1168 (2018). https://doi.org/10.1007/s10096-018-3236-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3236-4