Abstract
Purpose
To evaluate preoperative asymptomatic bacteriuria (ASB) treatment to reduce early-periprosthetic joint infections (early-PJIs) after hip hemiarthroplasty (HHA) for fracture.
Methods
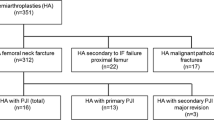
Open-label, multicenter RCT comparing fosfomycin-trometamol versus no intervention with a parallel follow-up cohort without ASB. Primary outcome: early-PJI after HHA.
Results
Five hundred ninety-four patients enrolled (mean age 84.3); 152(25%) with ASB (77 treated with fosfomycin-trometamol/75 controls) and 442(75%) without. Despite the study closed without the intended sample size, ASB was not predictive of early-PJI (OR: 1.06 [95%CI: 0.33–3.38]), and its treatment did not modify early-PJI incidence (OR: 1.03 [95%CI: 0.15–7.10]).
Conclusions
Neither preoperative ASB nor its treatment appears to be risk factors of early-PJI after HHA. ClinicalTrials.gov Identifier: Eudra CT 2016-001108-47


Similar content being viewed by others
References
Edwards C, Counsell A, Boulton C, Moran CG (2008) Early infection after hip fracture surgery. J Bone Jt Surg Ser B 90:770–777. https://doi.org/10.1302/0301-620X.90B6.20194
Cordero-Ampuero J, De Dios M (2010) What are the risk factors for infection in hemiarthroplasties and total hip arthroplasties? Clin Orthop Relat Res 468:3268–3277. https://doi.org/10.1007/s11999-010-1411-8
Phillips JRA, Moran CG, Manktelow ARJ (2013) Periprosthetic fractures around hip hemiarthroplasty performed for hip fracture. Injury 44:757–762. https://doi.org/10.1016/j.injury.2012.09.015
Gallardo-Calero I, Larrainzar-Coghen T, Rodriguez-Pardo D, Pigrau C, Sánchez-Raya J, Amat C et al (2016) Increased infection risk after hip hemiarthroplasty in institutionalized patients with proximal femur fracture. Injury 47. https://doi.org/10.1016/j.injury.2015.12.032
Vigilància de la infecció nosocomial als hospitals de Catalunya (VINCat), informe 2017. https://catsalut.gencat.cat/web/.content/minisite/vincat/documents/informes/informe-2017.pdf
Nicolle LE, Gupta K, Bradley SF, Colgan R, DeMuri GP, Drekonja D et al (2019) Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 update by the Infectious Diseases Society of Americaa. Clin Infect Dis 68:1611–1615. https://doi.org/10.1093/cid/ciz021
Sousa R, Muñoz-Mahamud E, Quayle J, Da Costa LD, Casals C, Scott P et al (2014) Is asymptomatic bacteriuria a risk factor for prosthetic joint infection? Clin Infect Dis 59:41–47. https://doi.org/10.1093/cid/ciu235
Cordero-Ampuero J, González-Fernández E, Martínez-Vélez D, Esteban J (2013) Are antibiotics necessary in hip arthroplasty with asymptomatic bacteriuria? Seeding risk with/without treatment. Clin Orthop Relat Res 471:3822–3829. https://doi.org/10.1007/s11999-013-2868-z
Drekonja DM, Zarmbinski B, Johnson JR (2013) Preoperative urine cultures at a veterans affairs medical center. JAMA Intern Med 173:71. https://doi.org/10.1001/2013.jamainternmed.834
Bouvet C, Lübbeke A, Bandi C, Pagani L, Stern R, Hoffmeyer P, et al. (2014) Is there any benefit in pre-operative urinary analysis before elective total joint replacement? Bone Joint J [cited 2021 14];96-B:390–4. https://pubmed.ncbi.nlm.nih.gov/24589797/. https://doi.org/10.1302/0301-620x.96b3.32620
Mayne AIW, Davies PSE, Simpson JM (2018) Antibiotic treatment of asymptomatic bacteriuria prior to hip and knee arthroplasty; a systematic review of the literature. Surgeon [cited 2021 14];16:176–82. https://pubmed.ncbi.nlm.nih.gov/29174023/. https://doi.org/10.1016/j.surge.2017.08.007
Langenhan R, Bushuven S, Reimers N, Probst A (2018) Peri-operative antibiotic treatment of bacteriuria reduces early deep surgical site infections in geriatric patients with proximal femur fracture. Int. Orthop [cited 2021 14];42:741–6. https://pubmed.ncbi.nlm.nih.gov/29224055/. https://doi.org/10.1007/s00264-017-3708-7
Moher D, Schulz KF, Altman DG, Lepage L (2001) The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. Ann Intern Med 134:657–662. https://doi.org/10.7326/0003-4819-134-8-200104170-00011
Zimmerli W, Trampuz A, Ochsner PE (2004) Current concepts: prosthetic-joint infections. N Engl J Med 351:1645–1654. https://doi.org/10.1056/NEJMra040181
Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM et al (2013) Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 56:e1–e25. https://doi.org/10.1093/cid/cis803
Glynn MKSJ (1984) The significance of asymptomatic bacteriuria in patients undergoing hip/knee arthroplasty. Clin Orthop Relat Res 185:151–154
David TS, Vrahas MS (2000) Perioperative lower urinary tract infections and deep sepsis in patients undergoing total joint arthroplasty. J Am Acad Orthop Surg 8:66–74. https://doi.org/10.5435/00124635-200001000-00007
Rajamanickam A, Noor S, Usmani A (2007) Should an asymptomatic patient with an abnormal urinalysis (bacteriuria or pyuria) be treated with antibiotics prior to major joint replacement surgery? Cleve Clin J Med 74:17–18. https://doi.org/10.3949/ccjm.74.Electronic_Suppl_1.S17
Otermin I, Rivero M, Hidalgo Á (2009) Es necesario retrasar o suspender la cirugía en el caso de una posible bacteriuria asintomática? ¿y una cirugía con implantes en ortopedia? Enferm Infecc Microbiol Clin 27:252–253. https://doi.org/10.1016/j.eimc.2008.03.005
Nicolle L (2019) Symptomatic urinary tract infection or asymptomatic bacteriuria? Improving care for the elderly. Clin Microbiol Infect 25:779–781. https://doi.org/10.1016/j.cmi.2019.03.013
Bosch-Nicolau P, Falcó V, Viñado B, Andreu A, Len O, Almirante B et al (2017) A cohort study of risk factors that influence empirical treatment of patients with acute pyelonephritis. Antimicrob Agents Chemother 61:1–11. https://doi.org/10.1128/AAC.01317-17
Falagas ME, Kastoris AC, Kapaskelis AM, Karageorgopoulos DE (2010) Fosfomycin for the treatment of multidrug-resistant, including extended-spectrum β-lactamase producing, Enterobacteriaceae infections: a systematic review. Lancet Infect Dis 10:43–50. https://doi.org/10.1016/S1473-3099(09)70325-1
Patel SS, Balfour JA, Bryson HM (1997) Fosfomycin Tromethamine. A review of its antibacterial activity, pharmacokinetic properties and therapeutic efficacy as a single-dose oral treatment for acute uncomplicated lower urinary tract infections. Drugs 53:637–656. https://doi.org/10.2165/00003495-199753040-00007
Sousa RJG, Abreu MA, Wouthuyzen-Bakker M, Soriano AV (2019) Is routine urinary screening indicated prior to elective total joint arthroplasty? A systematic review and meta-analysis. J Arthroplast 34:1523–1530. https://doi.org/10.1016/j.arth.2019.03.034
Sprowson AP, Jensen C, Chambers S, Parsons NR, Aradhyula NM, Carluke I et al (2016) The use of high-dose dual-impregnated antibiotic-laden cement with hemiarthroplasty for the treatment of a fracture of the hip the fractured hip infection trial. Bone Jt J 98-B:1534–1541. https://doi.org/10.1302/0301-620X.98B11.34693
Jameson SS, Jensen CD, Elson DW et al (2013) Cemented versus cementless hemiar- throplasty for intracapsular neck of femur fracture--a comparison of 60,848 matched patients using national data. Injury 44:730–734
Middleton RG, Uzoigwe CE, Young PS et al (2014) Peri-operative mortality after hemi- arthroplasty for fracture of the hip: does cement make a difference? Bone Jt J 96-B:1185–1191
Barbero JM, Montero E, Vallés A, Plasencia MA, Romanyk J, Gómez J (2016) Prosthetic joint infection in patients with hip fracture. Differences from infection of elective prosthesis. Rev Esp Quimioter 29:273–277
Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM (2005) Infectious diseases society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis 40:643–654. https://doi.org/10.1086/427507
Acknowledgements
We thank Maria Romero (Trialance, S.C.C.L.) for medical writing support, Santiago Perez Hoyos (Unitat d’Estadística i Bioinformàtica (UEB)) for the statistical calculations, and Mercedes Vila for her assistance in the methodology and implementation of the project.
List of collaborators/group of investigators for BARIFER clinical trial
This is a multicenter study. In each institution, there are many researchers that have helped to make this study possible. We are deeply indebted to these collaborators, who are:
Jaume Mestre and Maria del Mar Villar (Internal Medicine Department, Hospital Universitari Vall d’Hebron, Universitat Autònoma de Barcelona, Barcelona, Spain)
Álvaro Corrales Díaz and Myriam Rodríguez Rodríguez (Orthopedic Surgery Department Hospital Universitario Virgen Macarena, Seville, Spain)
Nerea Hernández González and Lorena Díez López (Orthopedic Surgery Department, Hospital Universitario Cruces, Vizcaya, Spain)
Javier Cobo (Infectious Diseases Department, Hospital Universitario Ramón y Cajal, Madrid, Spain) and Isabel Perez Millán (Geriatrics Department, Hospital Ramón y Cajal, Madrid, Spain).
Ma Isabel Perez Núñez (Orthopedic Surgery Department, Hospital Universitario Marqués de Valdecilla, Santander, Spain), M Carmen Fariñas Alvarez (Infectious Diseases Department, Hospital Universitario Marqués de Valdecilla, Santander, Spain), Hospital and Zoilo Yusta Escudero (Geriatrics Department, Hospital Universitario Marqués de Valdecilla, Santander, Spain),
Elena Muñez Rubio, Isabel Sánchez Romero (Hospital Universitario Puerta de Hierro, Majadahonda, Spain).
Cristina Dauder Gallego (Orthopedic Surgery Department, Hospital Universitario Fundación Alcorcón. Madrid, Spain), Oriol Martin Segarra (Internal Medicine Department, Infectious Diseases Division, Hospital Universitario Fundación Alcorcón. Madrid, Spain), Jesús Ignacio Collado Álvarez and Ma Mar Bermejo Olano (Internal Medicine Department Hospital Universitario Fundación Alcorcón. Madrid, Spain).
Oscar Murillo (Infectious Diseases Department, Hospital Universitari de Bellvitge, Barcelona, Spain), Salvador Pedrero (Orthopedic Surgery Department Hospital Universitari de Bellvitge, Barcelona, Spain).
Melcior Riera (Internal Medicine Department, Hospital Universitario Son Espasses, Palma de Mallorca, Spain).
María Gomáriz Díaz (Microbiology Department. Hospital Universitario Donostia), Gaspar De la Herrán (Orthopedic Surgery Department. Hospital Universitario Donostia), H. Azkune (Infectious Diseases Department Hospital Universitario Donostia, San Sebastián, Spain).
Marta Almenara Fernández, Eduard Ramírez Bermejo, Judit Martínez Zaragoza, (Infectious Diseses Department, Hospital Santa Creu i Sant Pau, Barcelona, Spain) Ferran Navarro Risueño (Microbiology Department, Hospital Santa Creu i Sant Pau, Barcelona, Spain)
Funding
This work was supported by the Spanish Clinical Research Network (SCReN), co-finaced by the ISCIII-Subdirección General de Evaluación y Fomento de la Investigación, through the project PI15/02161 and by the Plan Nacional de I+D+i 2013-016 and ISCIIII, Subdireccion General de Redes y Centros de Investigacion Cooperativa, Ministerio de Economia, Industria y Competitividad, Spanish Network for Research in Infectious Diseases (REIPI RD16/0016/0003)-co-financed by European Development Regional Fund “A way to achieve Europe,” Operative program Intelligent Growth 2014-2020.
Author information
Authors and Affiliations
Contributions
Dr Rodriguez-Pardo and Dr Pigrau contributed to its conception, clinical trial design, protocol, data collection, patient recruitment, data analysis, and writing the paper with the assistance of a medical writer. Dr Corona and Dr Almirante contributed to its conception, clinical trial design, and reviewing and editing the manuscript. All the other authors participated in patient recruitment, data collection, and reviewing and editing the manuscript. All authors approved the submitted versions, had full access to the data (under confidentiality agreements), and vouch for the accuracy and completeness of the data and for the fidelity of the trial to the protocol.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rodríguez-Pardo, D., del Toro, M.D., Guío-Carrión, L. et al. Role of asymptomatic bacteriuria on early periprosthetic joint infection after hip hemiarthroplasty. BARIFER randomized clinical trial. Eur J Clin Microbiol Infect Dis 40, 2411–2419 (2021). https://doi.org/10.1007/s10096-021-04241-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-021-04241-2